An AI-guided Pacemaker For the Brain Boosts Learning
Published in Neuroscience

Quick: what do you get when you combine an AI, a dozen electrodes and the human brain?
Answer: a boost in memory. Specifically, verbal memory that helps you remember a list of random words, a speech or maybe parts of a book you recently read. Plus it happens without any effort on your part or outside interference.
Duh, you’re probably thinking, I’ve heard this before. Yes, brain stimulation has been on a roll for the past few years. There’s direct transcranial stimulation (tDCS), where you put on a cap of electrodes and the current zaps across the brain. You can also meddle with your brain’s electrical firings with magnets or even ultrasound.
(Sometimes tDCS helps with learning, but it doesn’t always work.)
No, I’m talking about something a lot more hardcore: deep brain stimulation (DBS). Here, doctors use tiny electrodes directly inserted into the brain to deliver zaps that give brain circuits a boost.
Obviously no one wants to get brain surgery for a quick memory fix, so why care? The thing is, because electrodes can be implanted strategically, they can target focused circuits and lower the chance of interfering with the brain’s other normal functions.
In fact, DBS is already clinically approved to stop seizures in severe epilepsy and reduce tremors in Parkinson’s disease. Scientists also think that it could help people with memory loss from Alzheimer’s disease or trauma—hence the interest in its effect on learning.
What’s more, data gathered from implanted electrodes could guide the development of next-gen non-invasive devices, offering clues on where in the brain to target and when to zap.
The ultimate goal is to have a totally autonomous device that sits outside the brain, giving it a boost only when needed, like a caring guardian.
So far, however, results are mixed. This led researchers from the University of Pennsylvania to wonder: what if DBS only works when the brain isn’t functioning optimally? And more importantly—can we automate the process?
To test out the idea, the team recruited a precious resource: patients with severe epilepsy awaiting surgery. Doctors often implant hundreds of electrodes into various parts of their brains to track down the root of their seizures, with some expediently already in the brain’s memory circuits.
The researchers monitored the neural activity of 25 patients as they memorized a list of random words. Then, as a distraction, the patients solved some simple math problems, and then tried to recall as many words as possible. In this way, the team teased out the patterns of brain activity associated with successfully remembering a word or forgetting one.
It came down to activity in the lateral temporal cortex, a major node in the brain’s memory network. The firing patterns here had the best predictive power on whether a patient would later recall the word.
Here’s the clever part: using this data, the researchers taught a computer algorithm to decode in real-time whether the brain was in a “remembering” state. If not, the software would instruct the implanted electrodes to trigger a small zap to stimulate the lateral temporal cortex—otherwise they stayed off.
In other words, the algorithm is controlling when to zap or not—a large departure from previous generation DBS models that are constantly on.
The pacemaker seemed to work. In a series of memory tests, the patients tried to recall some word lists with the device on. Other lists, recalled with the device off, were used as a control.
Importantly, the patients couldn’t feel the stimulation. This “blinded” them to whether the device was actually working, which helps reduce placebo effects.
On average, the patients performed roughly 15 percent better with the device on. A modest boost, for sure, but the team has ideas to make it even better. For example, an implant that helps the brain fish out specific memories—rather then boosting storage—might further sharpen memories. (However, note that we don’t actually know if this “smart” device works better than the previous generation always-on devices: the authors never directly compared the two!)
Perhaps more important is that scientists are inching ever-so-close to understanding the patterns of brain activity that predicts a high-functioning brain state. With such a measure in place (likely different for each individual), scientists can then work on noninvasive ways to recreate those patterns in patients who need the boost.
Scientists at the University of Southern California and Wake Forest University, for example, are working on a “memory prosthesis” that recreates neural signals underlying memories. Using complex mathematical models, they’re attempting to extract the crucial electrical patterns that the hippocampus generates during learning, and deliver it back through electrodes if they’re ever forgotten.
It’s kind of like saving a digital copy of a memory, and then sending it back to the brain once the original has faded. (Pretty wild, hey?) Scientists have just begun exploring the idea in humans—so far it has has been tested on rats and monkeys only.
Although these devices are currently framed around rescuing failing memory, it’s tempting to broaden their use to the rest of us. After all, who doesn’t want a step up during those dreadful “brain fog” days?
The question is, would you be willing to go under the knife and risk a healthy brain for a small cognitive boost? If not, what if brain surgery, like LASIK, became simple and routine? And further, if a future ever comes when these devices are made non-invasive, like the smartphones in our pockets, what would that do to an already unequal society?
Follow the Topic
Your space to connect: The Psychedelics Hub
A new Communities’ space to connect, collaborate, and explore research on Psychotherapy, Clinical Psychology, and Neuroscience!
Continue reading announcement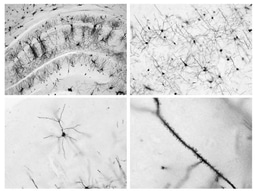




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in