Behind the Paper: How IL-6 shapes the anti-tumor battle and supports TGFβ immune modulatory vaccines in pancreatic cancer
Published in Bioengineering & Biotechnology, Cancer, and Immunology
What are immune modulatory vaccines?
In recent years, immune-modulatory vaccines have emerged as a promising strategy for cancer treatment, leveraging the immune system's ability to recognize and eliminate tumors. These vaccines target Tumor Microenvironment Antigens (TMAs), which are expressed by various cells within the tumor microenvironment. By focusing on these antigens, the vaccines aim to inflame the tumor microenvironment and counteract the mechanisms that allow cancer to evade immune responses.
One such TMA is transforming growth factor-β (TGFβ), a protein that tumors exploit to suppress immune activity and create a protective niche for their growth. A TGFβ-based immune modulatory vaccine trains the immune system to recognize and attack cells that overproduce TGFβ (Figure 1). This approach shows great promise, as it not only directly targets tumor cells but also reprograms the tumor microenvironment, rendering it less conducive to cancer progression.
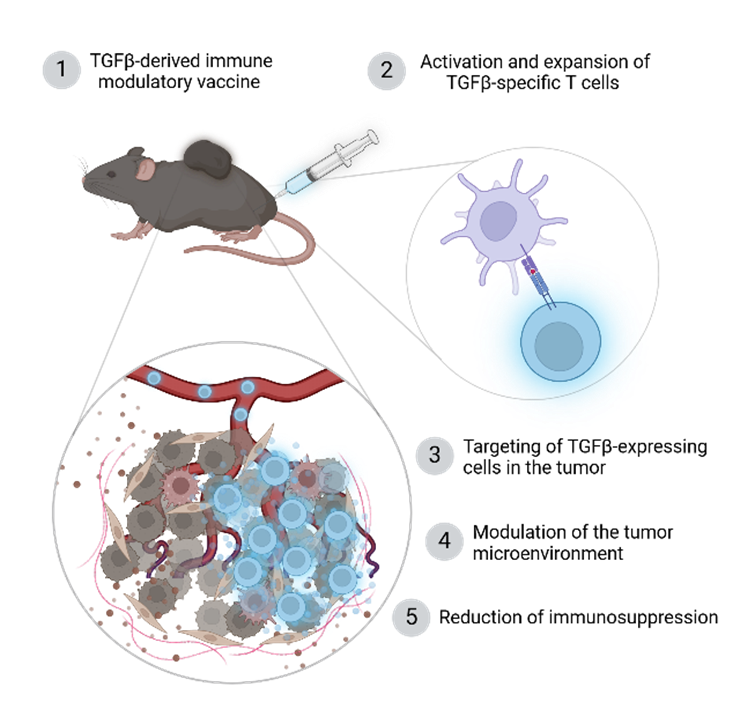
Figure 1. Mode of action of a TGFβ-based immune modulatory vaccines. Created in https://BioRender.com.
In this paper, we focused on this type of vaccine, exploring how it can be optimized for one of the most challenging cancers to treat: pancreatic cancer.
Introduction: turning IL-6, a tumor’s ally, into an immunotherapy asset
In the fight against pancreatic cancer, one of the most aggressive and lethal cancers, new strategies are urgently needed. Our research uncovers the surprising role of interleukin-6 (IL-6) in enhancing the immune system’s ability to fight tumors, specifically in the context of TGFβ immunity and TGFβ-based immune modulatory vaccines.
While IL-6 is typically seen as a villain in cancer progression, our work reveals its potential to support anti-tumor immunity in specific contexts. This unexpected finding has significant implications for the design of novel immunotherapies.
The challenge: finding allies in the tumor microenvironment
Our journey began with a puzzle: why did adding a drug to block IL-6 receptors (IL-6R) impaired the efficacy of radiotherapy and immunotherapy in a clinical trial for pancreatic cancer? Earlier studies suggested that IL-6 fosters tumor growth and suppresses immunity, so it seemed logical to try to block it. However, patients receiving this treatment, alongside immune checkpoint inhibitors and radiotherapy, didn’t benefit. Instead, their outcomes were worse compared to those who didn’t block IL-6.
To unravel this, we turned to the lab, using animal models of pancreatic cancer and analyzing data from patients. Our goal was to understand how IL-6 interacts with the immune system during an anti-tumor response, particularly in the context of the TGFβ-immune modulatory vaccine we’ve been studying.
A breakthrough: IL-6 as a positive immune modulator
The TGFβ vaccine works by training the immune system to recognize and attack cells that produce TGFβ. Interestingly, we discovered that treatment with the TGFβ vaccine increased the intratumoral levels of IL-6, a molecule that is traditionally considered a villain in the context of cancer (figure 2).
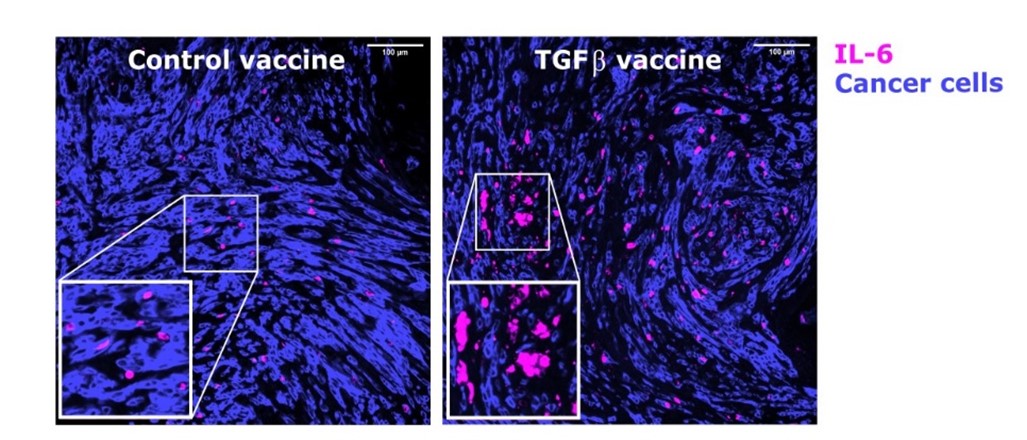
Figure 2. Treatment with the TGFβ vaccine increases the levels of IL-6 in the tumor in animal models of pancreatic cancer. Tumor cells are shown in blue, IL-6 is shown in pink. Data adapted from Figure 2 from Perez-Penco et al. The anti-tumor activity of TGFβ-specific T cells is dependent on IL-6 signaling. Cell Mol Immunol (2024).
However, blocking IL-6R in our animal models completely abrogated the vaccine’s effectiveness. Further experiments demonstrated that IL-6 plays a pivotal role in promoting the development and activity of specific immune cells, particularly T cells, within the tumor microenvironment.
Blocking IL-6 disrupted this process, leading to fewer T cells infiltrating the tumor and making the remaining ones less effective. Interestingly, we also observed a shift in other immune cells, like macrophages, towards a more suppressive state, further hampering the anti-tumor immune response that would be responsible for fighting and clearing the tumor (figure 3).
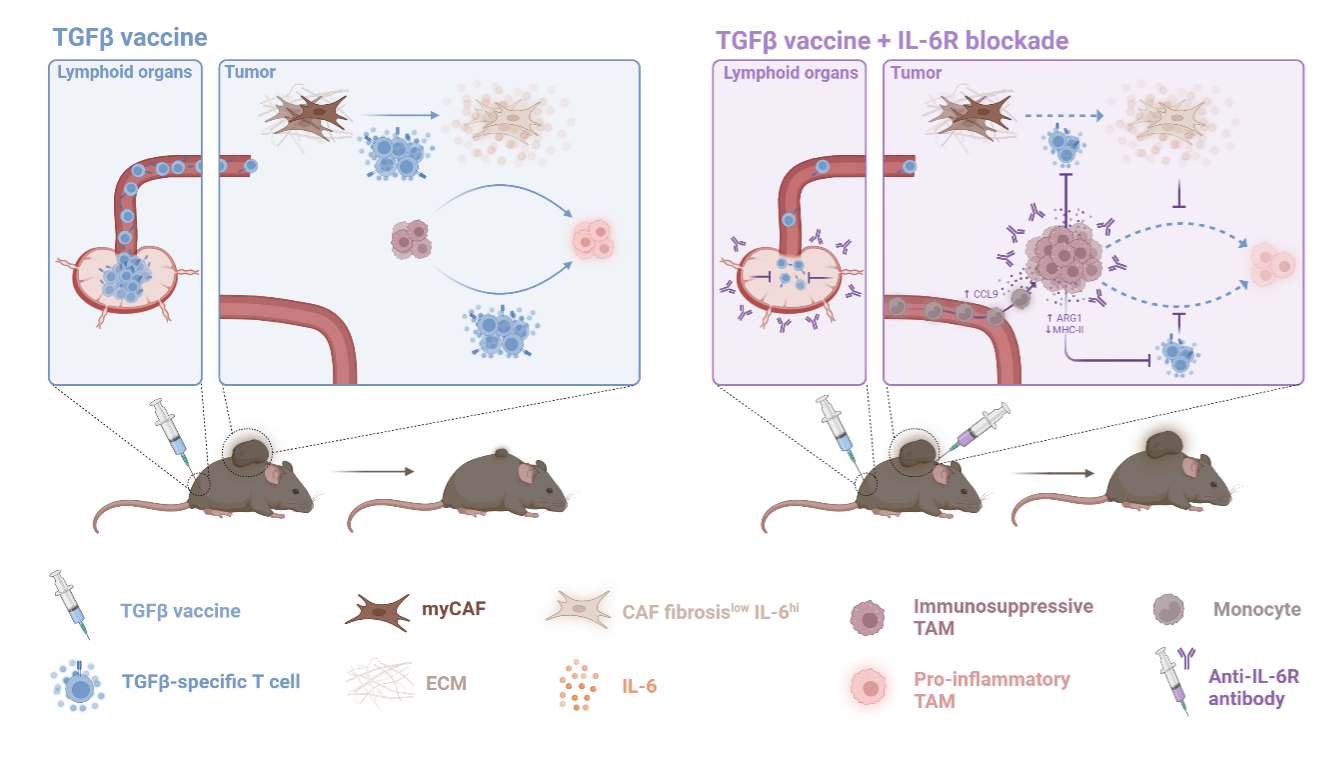
Figure 3. Suggested mechanism of how IL-6 might be beneficial for the anti-tumor efficacy of the TGFβ vaccine, particularly during tumor shrinkage caused by the vaccine. Reproduced from Supplementary Figure 2 from Perez-Penco et al. The anti-tumor activity of TGFβ-specific T cells is dependent on IL-6 signaling. Cell Mol Immunol (2024). Created in https://BioRender.com.
Lessons from patients: bridging bench and bedside
Looking at data from two clinical trials, we found that patients with strong TGFβ-specific immune responses at the start of treatment had better survival rates when IL-6 was not blocked. However, for those receiving IL-6R inhibitors, this survival advantage disappeared.
This confirmed what our lab and animal studies suggested: IL-6 is a crucial ally for certain types of cancer immunotherapy.
Challenges and surprises along the way
Conducting this research was not without its hurdles. One surprising moment came when we realized that IL-6, traditionally labeled as a tumor-promoting factor, could support anti-tumor immunity under the right conditions. This challenged our assumptions and required us to rethink how we approached the tumor microenvironment.
Another challenge was navigating the complexity of immune responses and cellular populations within the tumor. Cancer is not a single disease, and the role of the immune system varies significantly depending on the context. Untangling these intricate interactions required countless hours of experiments, thorough data analysis, and in-depth discussions.
The human element: why this work matters
Pancreatic cancer is notoriously challenging to treat, leaving patients and their families with limited options. The potential for a deeper understanding of IL-6 to open the door to more effective therapies has been a driving force behind our work.
For us, one of the most rewarding aspects of this journey was witnessing how a seemingly small detail—IL-6 signaling—could have such a profound impact on treatment outcomes. It’s a powerful reminder that in science, even the smallest discoveries can lead to the most transformative breakthroughs.
Looking ahead: a roadmap for future research
Our findings underscore the importance of caution when designing therapies that target IL-6. While it may be advantageous in some cancers or contexts, it could prove harmful in others. Future research will pinpoint the specific conditions under which IL-6 should be inhibited or preserved. By unraveling the complex interplay between the immune system and the tumor, we aspire to unlock new possibilities for effective and curative treatments.
Conclusion: redefining the role of IL-6 in cancer immunotherapy
This paper highlights the intricate complexity of cancer and the immune system. It reminds us that in the fight against cancer, nothing is as simple as it seems. IL-6, once thought to be an unequivocal villain, may just be the unexpected hero in the context of our TGFβ vaccine.
We are excited to share this journey with you and hope that it sparks discussions, conversations and collaborations in the broader scientific community. Cheers to unexpected findings!
Follow the Topic
-
Cellular & Molecular Immunology

A monthly journal from the Chinese Society of Immunology and the University of Science and Technology of China, covering both basic immunology research and clinical applications.



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in