Considering Patients' Perspectives and Expectations for OnabotulinumtoxinA Treatment and Physiotherapy and Rehabilitation Treatments in Chronic Migraine Patients
Published in Healthcare & Nursing, General & Internal Medicine, and Pharmacy & Pharmacology
OnabotulinumtoxinA and Chronic Migraine
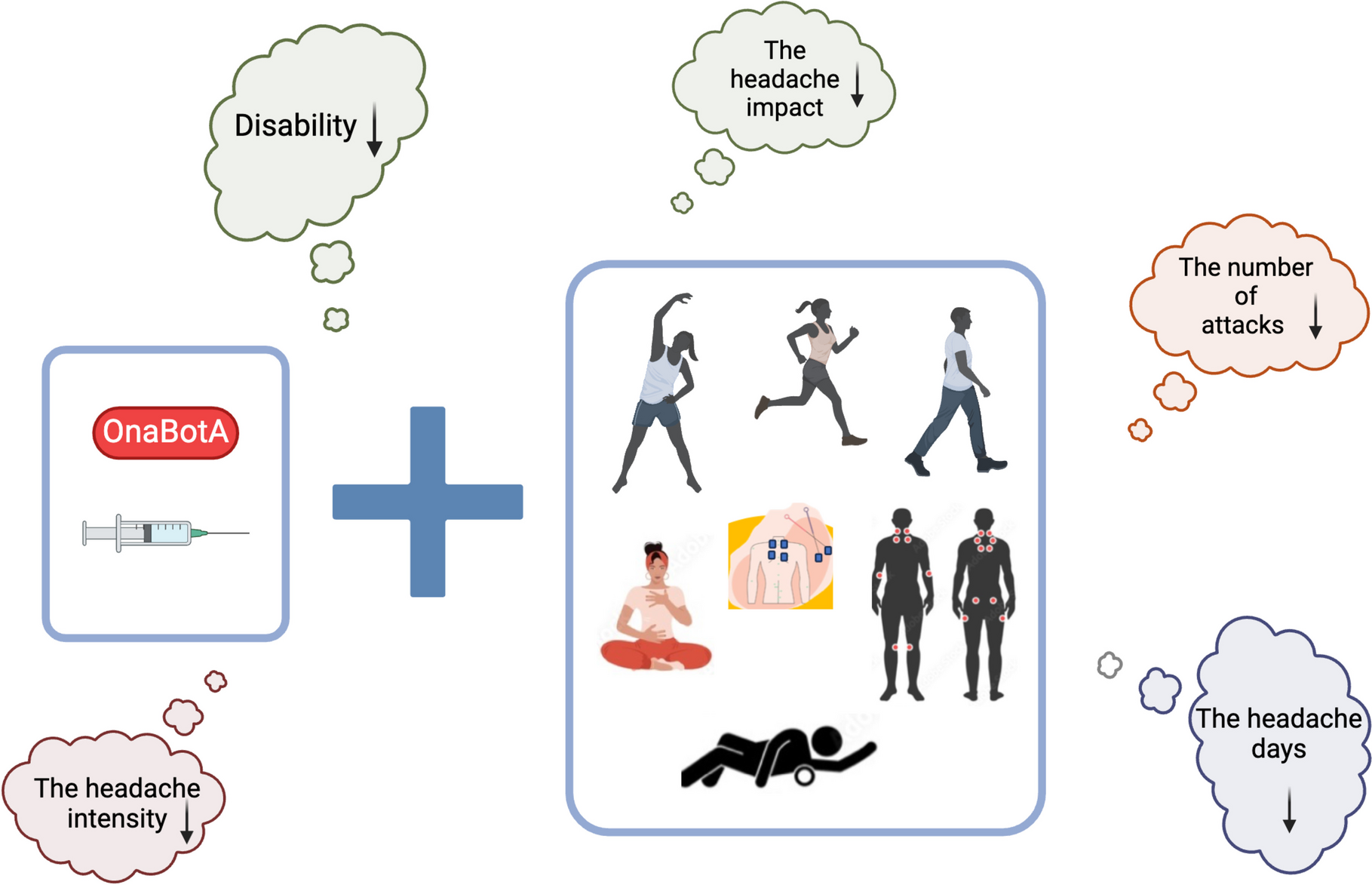
OnabotulinumtoxinA (OnaBotA) is administered to targeted head and neck muscle areas every three months to treat chronic migraine. It offers benefits such as reducing the number of headache days, frequency of attacks, headache intensity, disability, and improving quality of life (QoL). In addition to its limited effect duration of 3–4 months and the fact that OnaBotA treatment may not be covered by health insurance in hospitals, holistic complementary approaches are also recommended to prevent possible side effects from OnaBotA, reduce patients' dependence on medical treatments, support treatment compliance, and actively involve patients in migraine management.
So What Are Physiotherapy and Rehabilitation Treatments, Which Are Holistic Complementary Approaches?
Physiotherapy and rehabilitation treatments (PRT), exercises, hot-cold applications, electrical stimulation, massages and mobilizations, manipulations, and manual treatments such as osteopathy, which are the basic components of holistic complementary approaches, have minimal side effects and actively involve patients in the treatment processes.
Possible Benefits of OnabotulinumtoxinA and Physiotherapy and Rehabilitation Treatments When Applied Together
Considering the areas where OnaBotA is applied, strengthening the muscles in the head and neck, stretching the tissues to reduce stiffness, and improving cervical posture may increase the effectiveness of the treatment. Exercises, manual therapy and soft tissue release methods can provide varying degrees of PRT in the treatment of CM. In addition to OnaBotA application, which requires a repeat after 3–4 months, providing PRT applications that can show benefits over 3–4 months may lead to long-term improvements.
These treatments are reported to be applied less frequently in clinical migraine care, which may lead to healthcare professionals rarely prescribing PRT to patients. In some cases, patients may not have access to a physiotherapy and rehabilitation clinic dedicated to migraine in their hospital or city, potentially limiting their awareness of PRT options. Therefore, it is also important to consider patients' opinions regarding these treatments. In this study, we aimed to explore CM patients' perspectives and expectations regarding PRT combined with OnaBotA. Understanding these perspectives will help plan and implement evidence-based physiotherapy and rehabilitation strategies.
What did we find?
- PRT was recommended for 41.8% of the patients who received OnaBotA, compared to 18.9% in the group that did not receive OnaBotA. Neurologists were the primary recommenders for the OnaBotA group (38.2% vs. 7.5% in the group that did not receive OnaBotA).
- The percentage of patients who received neck stabilization exercises (12.7%) and pilates (12.7%) was higher in the OnaBotA group.
- The percentage of patients who received all expectations regarding PRT was higher in the OnaBotA group (76.4%) than in the group that did not receive OnaBotA (33.8%).
- The improvements in migraine symptoms in patients who received OnaBotA and PRT together were in disability, headache intensity, headache impact, number of attacks, and headache days.
- The responses to the question “How many months of physiotherapy and rehabilitation treatment do you think you need to get better?” were 3.83 ± 1.17 in the OnaBotA group and 3.06 ± 2.64 in the group non-receiving OnaBotA.
- The percentage of those who wanted to receive treatment from physiotherapists specializing in migraine was 96% in the OnaBotA group and 94% in the non-receiving group.
- The percentage of those who had easy access to physiotherapy and rehabilitation treatment was 34% in the OnaBotA group and 30% in the non-receiving group.
- Our findings provide insights into the potential benefits of combining OnaBotA with physiotherapy and rehabilitation in managing CM. Patients receiving OnaBotA may benefit from complementary therapies and may improve their overall treatment experience. Patients appear motivated to increase their awareness and participation in the treatment process.
Notes for Future Studies
- Future research should focus on conducting randomized controlled trials to systematically evaluate the combined effects of OnaBotA and PRT.
- Such studies should include larger sample sizes, standardized intervention protocols, and objective measurements to assess the benefits and limitations of this combined therapeutic approach.
- They should aim to provide robust evidence to guide clinical practice and improve patient outcomes in migraine management.
Follow the Topic
-
SN Comprehensive Clinical Medicine

A broadly based, peer reviewed journal that publishes original research in all disciplines of clinical medicine and their subspecialties, including all aspects of Imaging, Surgical and Medical studies related to diagnosis, treatment and management.
Related Collections
With Collections, you can get published faster and increase your visibility.
Obesity and type 2 diabetes
According to the recent esteems, more than 800 million adults have type 2 diabetes (T2D), with an increase of about 600 million in the last 30 years. The largest increases are in low-income and middle-income countries. As a matter of fact, a parallel increase has been constantly reported for the prevalence of obesity and overweight. Obesity has increased to fewer than 2 billion in the last 5 years. Obesity was recognized as a disease by WHO about 80 years ago and very recently by the Italian Parliament as a chronic, progressive, and relapsing disease.
A multifactorial etiology (both genetic and environmental factor) has been proposed for T2D with two main pathogenetic mechanisms (the defect of insulin production and insulin resistance). The dysfunction of β-cells is commonly attributed to the loss of β-cell mass (by exhaustion) or apoptosis (by glucotoxicity and lipotoxicity). More complex mechanisms and interactions are involved, such as dedifferentiation of β-cells, oxidative stress, induction of disallowed genes, dedifferentiation, transdifferentiation, endoplasmic reticulum stress, altered prostaglandin signaling, mitochondrial dysfunction and amyloidosis. The insulin resistance (IR) is represented by the reduced response to insulin in the target tissues. Many hormones affect the action of insulin (classically, growth factors and insulin-like growth factor 1, glucagon, glucocorticoids, and catecholamines). Beyond the genetics, obesity, sedentary lifestyle, dietary habits, chronic stress and sleep deprivation can all negatively impact insulin sensitivity, and, recently, gut microbiota has been considered in the pathophysiology of T2D.
The signaling pathway of insulin may disrupted at different levels, from upstream (the insulin receptor) to downstream (for example, the glucose transporter or GLUT1-4).
In the development of T2D, extra-pancreatic factors are essential, such as the IR at the level of the skeletal muscles, the adipose tissue and the liver. The detrimental effects of IR virtually involve every tissue of the body that present the insulin receptor, and growing evidence in the literature support an important damage at the central nervous system.
The well-known complications of T2D are: diabetic kidney disease (DKD), diabetic retinopathy (DR), diabetic neuropathy (DN), metabolic dysfunction-associated steatotic liver disease (MASLD), cardiovascular disease (CVD) (coronary artery disease or CAD, stroke and peripheral artery disease or PAD).
Considering obesity, several districts of the body are affected by this disease, such as the respiratory system (apnoeas/hypopnoeas and hypoventilation during sleep), cardiovascular system (preserved or reduced left ventricular systolic function - heart failure, arrythmias and atrial fibrillation, systemic and pulmonary artery hypertension, aortic valve stenosis), lower limbs lymphedema, deep venous system and/or pulmonary thromboembolic disease, metabolism (hyperglycaemia and T2D, high triglyceride levels, and low HDL cholesterol levels, metabolic syndrome), the liver (MASLD and hepatic fibrosis), the kidney (microalbuminuria, reduced glomerular filtration rate), urinary incontinence, reproduction (anovulation, oligo-menorrhea and polycystic ovary syndrome, male hypogonadism), musculoskeletal system (osteoarthritis).
The recent Delphi Consensus defined obesity an excessive adiposity (based on recent anthropometric measures), with or without abnormal distribution or function of the adipose tissue, caused by multifactorial pathogenetic mechanisms (genetic, environmental, neurobiological, psychological, socioeconomic, nutritional and metabolic factors) and still incompletely understood. Obesity can cause systemic, chronic illness (the so-called clinical obesity), resulting in distinct clinical manifestations with specific signs/symptoms or limitations of activities of daily living. Pre clinical obesity confers an increased risk of developing clinical obesity as well as several other non-communicable diseases (NCDs), including T2D, CVD, certain types of cancer and mental illness. Because remission of clinical obesity does not imply cure, treatment of clinical obesity with resolution of clinical manifestations of organ dysfunction is matter of debate in order to evaluate the timing of the ongoing pharmacologic treatment. Clinical obesity may lead to severe organ dysfunction and end-organ damage, causing life-altering and/or potentially life-threatening complications. Coexisting obesity-related diseases should be considered in decision-making about indications to treatment and type of treatment.
The aim of this Collection is to provide a better understanding of the molecular and integrative mechanisms of the development of obesity and T2D, to ameliorate the clinical aspects and the relationships between both the diseases. A deeper knowledge of the specific profile and their multiple components may give a chance to a more efficient treatment in a personalized manner.
Possible topics include: basic mechanisms and clinal profiles of the patients, oxidative stress, chronic inflammation, hormonal and metabolic dysregulation, as areas involved in the development of obesity and/or T2D. Preventing strategies and newly developed agents to enhance fit behaviors and to contrast the pathogenetic mechanisms. Debate and research on advantages and disadvantages of measures of obesity and T2D and the outcomes after specific treatments.
Publishing Model: Hybrid
Deadline: Sep 30, 2026
Clinical and Translational Science in Pain and Headaches
Publishing Model: Hybrid
Deadline: Jun 30, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in