Does the risk from Covid-19 change over time?
Published in Healthcare & Nursing
Throughout the course of the Covid-19 pandemic, one of the key metrics driving policy decisions across the world has been Covid-19 case fatality risk. Debates, sometimes lacking in scientific basis, have raged on social media and elsewhere as to whether the risk of death from Covid-19 differs to that from other viral diseases, such as influenza. Although, the scientific evidence overwhelmingly indicates a significantly higher mortality risk in Covid-19 compared to influenza (at least prior to effective vaccinations) risk is unlikely to be static over time. Previous epidemiological studies have shown variation in risk over time at a population level, but it has been unclear whether this was due to changes in the propensity of the virus to cause severe disease or changes in the clinical vulnerability of those infected.
The need for our work came about as part of an evaluation of a pulse oximetry remote monitoring programme introduced in the National Health Service in England for people with Covid-19. The programme aimed to support early detection of low oxygen levels in people with Covid-19 and allow for early escalation of care. To effectively evaluate the impact of the programme we needed to understand whether the risk of hospital admission or death from Covid-19 was stable over time, leading to this analysis.
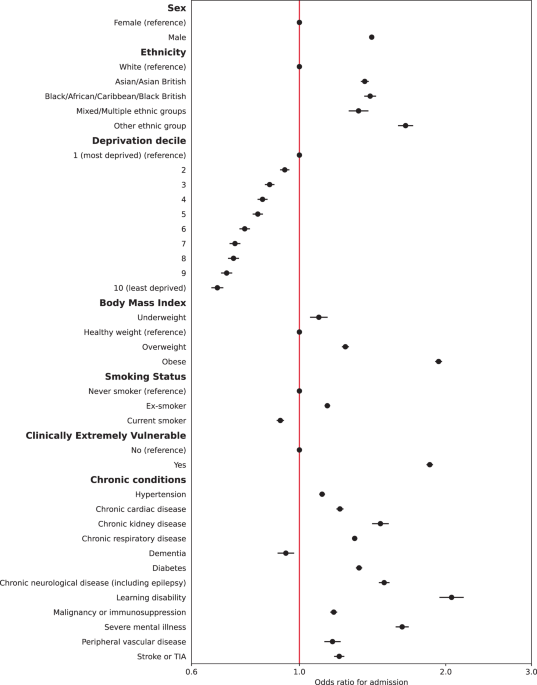
Our study found large variation in the case hospitalisation risk and case mortality risk within 28 days of a positive Covid-19 test from October 2020 to April 2021, with risk peaking in January 2021. Even after accounting for factors including age, sex, ethnicity, socioeconomic deprivation, BMI and presence of long-term conditions, there remained significant variation over time, indicating the role of factors external to the measurable clinical and demographic features of individuals in explaining Covid-19 risk. The alpha variant became the dominant Covid-19 strain in England from December 2020, which has been associated with higher virulence. Health system pressures may also play a role, with high bed occupancy in England over the winter of 2020/21. Our findings show a significant decline in mortality after January 2021, which is likely to be explained to a large extent by vaccinations. Exploration of these external factors was outside the scope of the current study and our available data but indicate a need for further research.
Previous studies, such as OpenSAFELY, have identified Covid-19 risk factors during the first wave of the pandemic. Our study confirmed many of the same risk factors as those from OpenSAFELY, including older age, being male, and in people from Asian or Black ethnic backgrounds or living in areas of higher socioeconomic deprivation. Our study looked at additional risk factors, such as learning disabilities and severe mental illness, finding that presence of either was associated with significantly higher odds of hospitalisation and death and indicating a need for interventions for those most at risk.
It is increasingly clear that as of April 2022, Covid-19 poses a different threat than it did in early 2020. While much of the world may have acquired a degree of immunity to the virus through infection or vaccination, over one third of the global population have not received a single dose. Viruses evolve, and there is a need for treatments and policy responses to evolve with them. As the pandemic progresses, it is crucial that research continues to consider how the risk posed by Covid-19 varies over time and between individuals to inform actions to protect those most at risk.
Follow the Topic
-
Nature Communications

An open access, multidisciplinary journal dedicated to publishing high-quality research in all areas of the biological, health, physical, chemical and Earth sciences.
Related Collections
With Collections, you can get published faster and increase your visibility.
Women's Health
Publishing Model: Hybrid
Deadline: Ongoing
Advances in neurodegenerative diseases
Publishing Model: Hybrid
Deadline: Mar 24, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in