Engaging Men: A Crucial Key to Ending HIV
Published in Ecology & Evolution, Sustainability, and Biomedical Research

What I know is that the pill is my life.
Sarah, age 43, is one of the many men and women in southern Uganda who are thankful for the antiretroviral drugs that allow them to manage her HIV.
Many men and women like Sarah in Uganda are living longer, healthier lives thanks to the widespread and rapid expansion of HIV treatment services in Africa. But on average, men are less likely to reach and maintain very low concentrations of HIV in their body thanks to treatment, sometimes because they need to travel for work, sometimes because clinics are closed when they are back home, or for other reasons. And because this means they remain infectious; they are more likely to pass on the virus to their female partners.
In our recently published study in Nature Microbiology Growing gender disparity in HIV infection in Africa: sources and policy implications, using data from the Rakai Community Cohort Study (RCCS) in southern Uganda, we report on how risks of HIV acquisition and heterosexual transmission are shifting by age and gender since the widespread adoption of HIV prevention and treatment measures. We further show that gender disparities in HIV viral suppression in this region are growing, and that closing these disparities could reduce HIV infections among women by half.
In southern Uganda more than 9% of adults are living with HIV, which is approximately 20 times higher than in the US. RCCS is the first and longest-running HIV population surveillance cohort in Africa and has been at the forefront of understanding the HIV epidemic. Since 2003, a period predating the widespread availability of antiretroviral therapy in Africa, RCCS has enrolled nearly 37,000 individuals, offering a unique vantage point into the evolving landscape of HIV infection through longitudinal data.
Our analysis tracked evolving heterosexual HIV epidemic dynamics in 36 communities in southern Uganda and covered a 15-year span of RCCS surveillance data, including records of new infections, deep sequence HIV genomic data, and behavioural information. RCCS data on HIV treatment uptake and viral suppression among persons with HIV were also integrated, enabling us to shed light on the mechanisms that drive changes in transmission dynamics, and where focused efforts might have greatest impact.
Changing Dynamics of HIV Incidence: A Shift from Adolescent Girls to Older Women
Historically, the highest number of new HIV cases in southern Uganda was among adolescent girls and young women aged 15-24 years. In our study, we document a significant shift in age patterns, with women 25-34 years becoming a new focal group, experiencing a slower decline in new infections than other age groups.
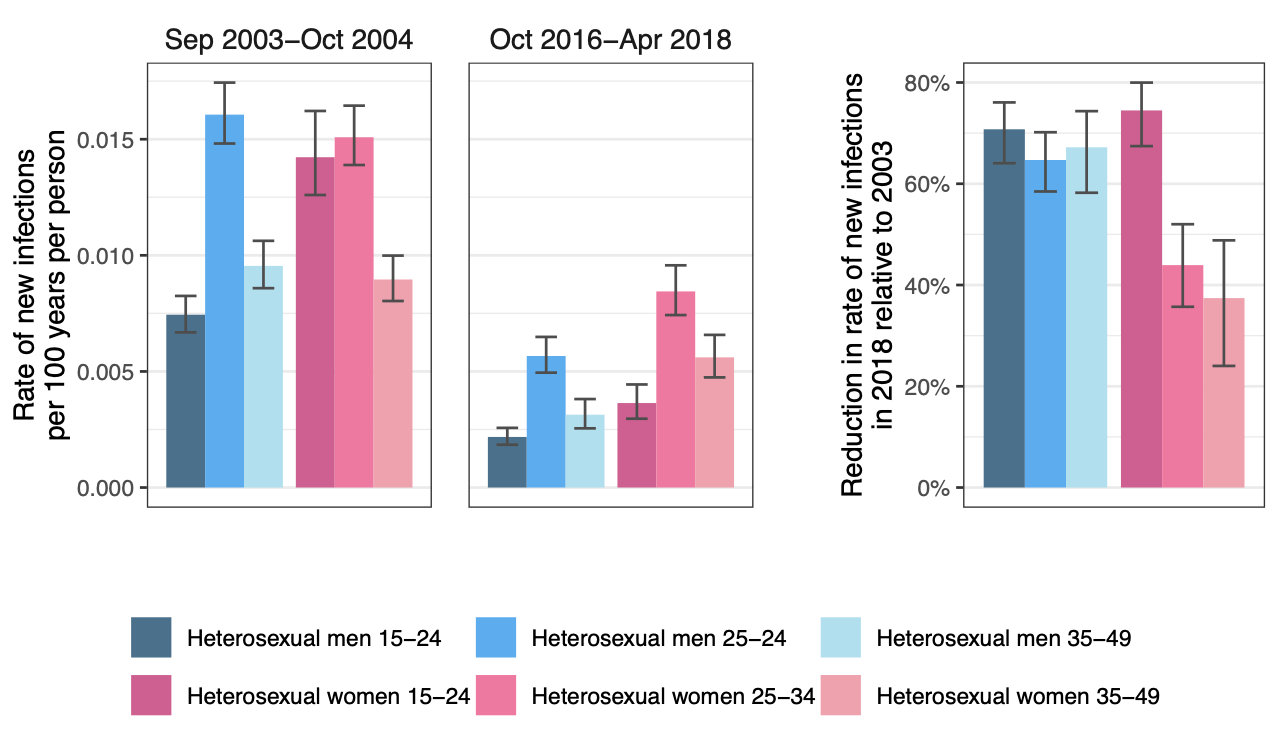
Shifting Dynamics: Men's Growing Role in HIV Transmission
We also document a significant difference in the rate of decline of new infections between men and women, with new infections among boys and men declining much faster. Additionally, by examining heterosexual transmission networks reconstructed from pathogen genomes, we show an increasing contribution of male-to-female transmission to new infections. This contribution has risen steadily from 57% to 63% over the period from 2003 to 2018, despite the fact that a greater number of women are living with HIV than men. Additionally, our analysis of transmission networks highlights that heterosexual male partners involved in transmission are now considerably older than they were a decade earlier, with most new infections originating from men aged 30 to 39 years.
Closing Viral Suppression Disparities: A Pathway to reducing new infections
Decades of extensive HIV research, including from RCCS, have consistently demonstrated that individuals on Antiretroviral Therapy (ART) who maintain suppressed HIV viral loads do not transmit HIV, reinforcing the concept that undetectable viral loads equate to untransmissible HIV (U=U). This insight is giving new hope and optimism into the lives of individuals living with HIV, as well as their partners and families.
Our data revealed growing gender disparity in the effectiveness of current healthcare services in achieving and sustaining viral suppression among men. Over time, we observed a consistent, more rapid increase in viral suppression rates among women in contrast to men. By the year 2018, this trend had resulted in female viral suppression rates being 1.5 to 2 times higher across all ages. This swifter ascent in viral suppression rates among women may, in part, explain the faster declines in HIV incidence rates among their male counterparts.
Overall, higher rates of ART uptake and viral suppression among women have contributed to a diminished risk of HIV transmission from female to their heterosexual male partners. This is not true to the same extent the other way round, with unsuppressed virus among heterosexual men leading to a higher likelihood of transmitting the virus to their female partners.
To estimate the likely impact of closing the viral suppression gap among men, we applied predictive statistical models grounded in the evolving transmission dynamics. Our projections indicate that closing the viral suppression gap in men could have effectively halved rates of new infections among women and eliminated gender disparities in acquiring HIV.
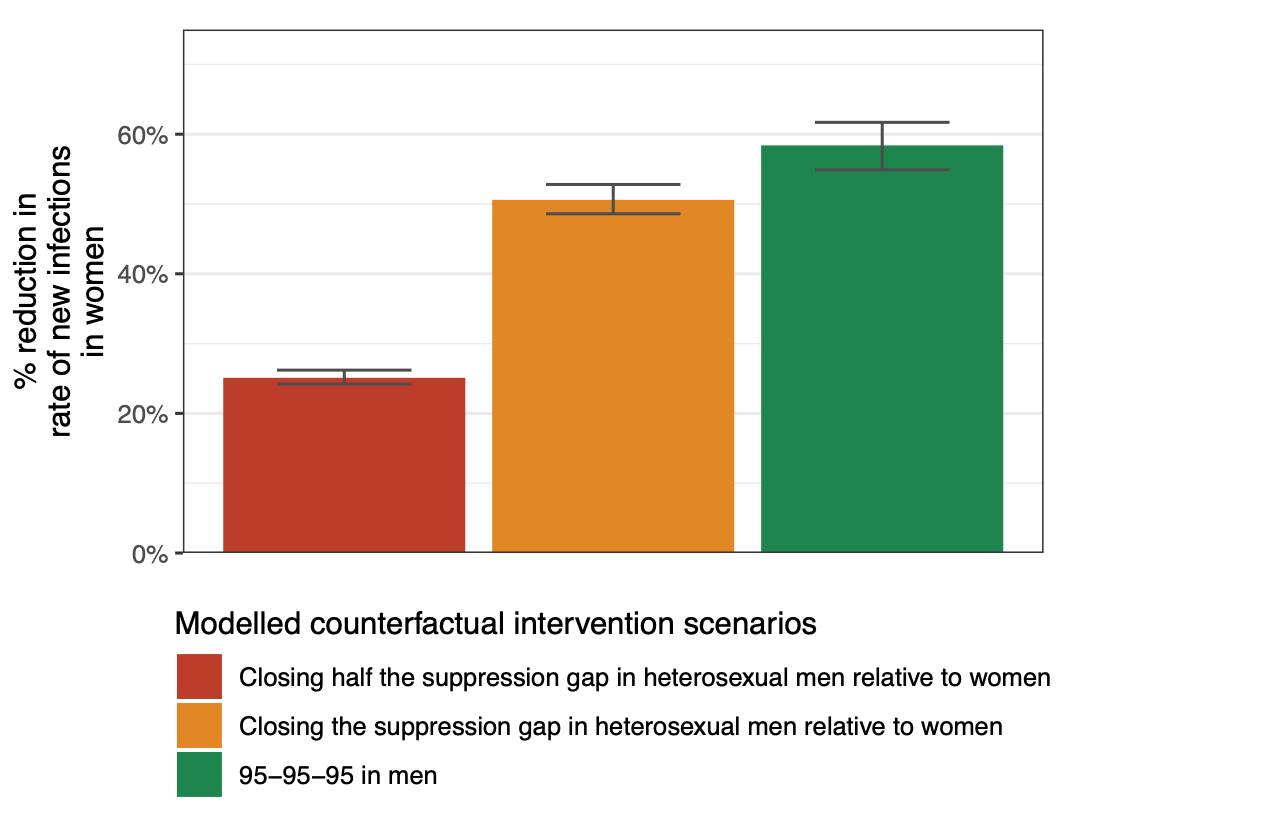
Figure 2: Projected reductions in the rate of new HIV infections in women during the last survey round analysed, under modelled counterfactual intervention scenarios.
Conclusions
With the scale up of various HIV interventions, including ART, we have witnessed a transition from adolescent girls and young women being the most affected to a shift towards older women. This shift is partly a result of gender disparities in viral suppression, with men lagging behind women in achieving and maintaining suppressed viral loads.
Our study findings emphasise the importance of addressing these disparities in ART uptake and viral suppression between men and women. By doing so, we can not only reduce HIV infections among women but also work towards closing the gender gap in HIV transmission. Achieving these goals will require concerted efforts, informed policies, and strengthened healthcare services.

Community leaders in southern Uganda and RHSP research staff participate in a community football tournament to raise awareness for HIV.
In this evolving battle against HIV, it is critical we adapt our strategies, bridge gaps in care, and ensure that individuals, regardless of their gender, have access to the lifesaving benefits of ART. Men often find it harder to stay in care owing to stigma, working hours and work-related mobility. It is important to design services in a way that everybody who would like to use them is able and feels empowered to do so. Routinely monitoring the changing dynamics of the epidemic and striving for equity in HIV care, we can move closer to the ultimate goal of controlling and, one day, eliminating HIV transmission.
Thanks to all my co-authors for their invaluable contributions to this blog post: Robert Ssekubugu , Kate Grabowski, Alexandra Blenkinsop, Lucie Abeler-Dörner, Louise Karlsson, and Oliver Ratmann.
Follow the Topic
-
Nature Microbiology

An online-only monthly journal interested in all aspects of microorganisms, be it their evolution, physiology and cell biology; their interactions with each other, with a host or with an environment; or their societal significance.
Related Collections
With Collections, you can get published faster and increase your visibility.
The Clinical Microbiome
Publishing Model: Hybrid
Deadline: Mar 11, 2026

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in