Establishing Digital Musculoskeletal Care as an Effective Alternative to In-Person Care
Published in Healthcare & Nursing and Pharmacy & Pharmacology

Context
The advent of digital health opens up a series of new possibilities for healthcare. In a context of pressing demand and financial constraints, the expectation is that technology, and, in particular, digital health, can help solve the imbalance between supply and demand, paving the way towards scalable care delivery models that are more accessible and inclusive. However, to achieve this, these models need to be developed and deployed in a way that ensures quality of care at scale.
Choosing the Disease Model
Musculoskeletal (MSK) conditions are the main cause of years lived with disability worldwide, and have a huge financial impact. Low back pain, in particular, is the single leading cause of disability worldwide, and therefore one of the major problems the healthcare community needs to address.
Digital Care Delivery in Musculoskeletal Conditions
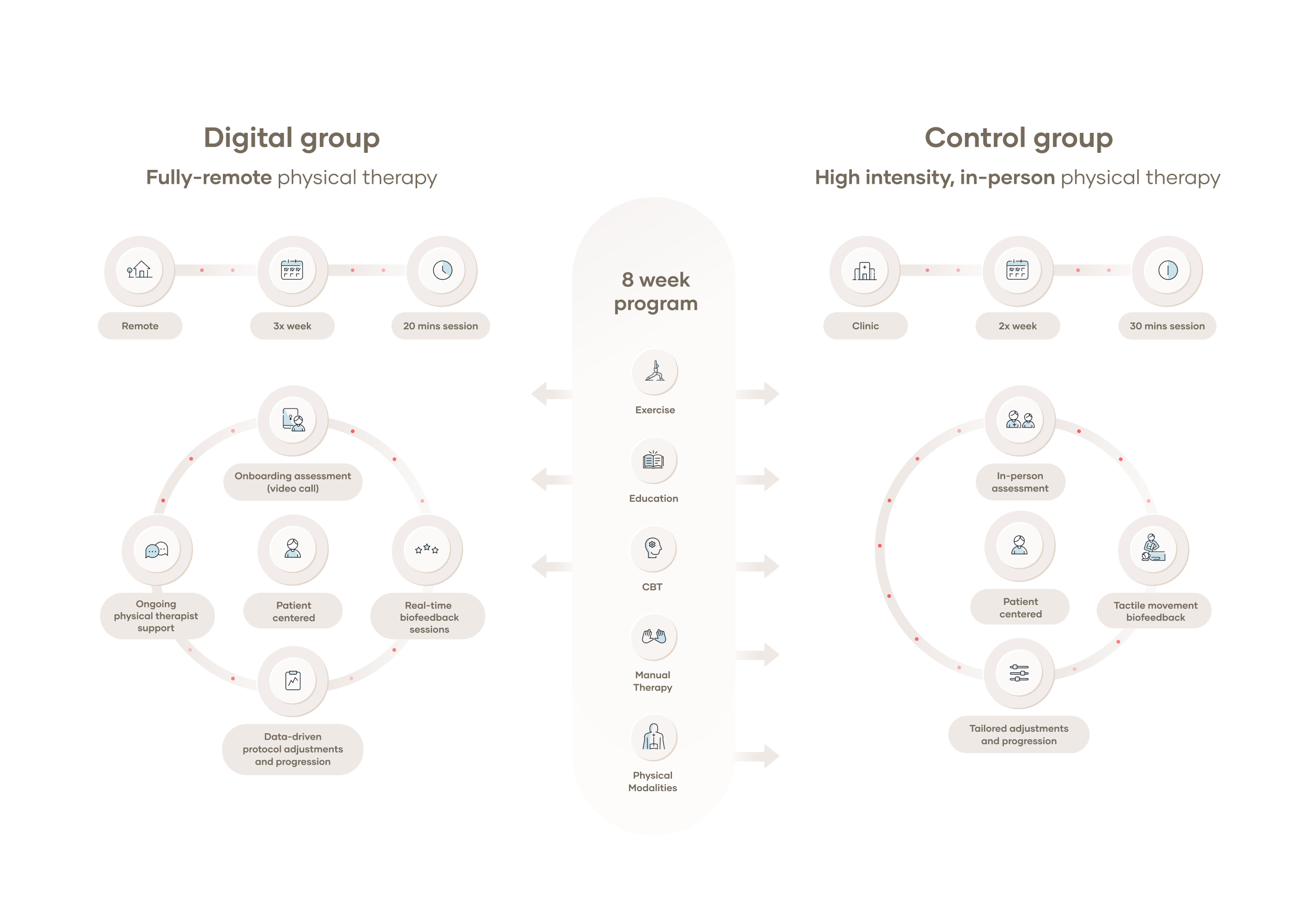
A wealth of literature on the management of MSK conditions supports therapeutic exercise, education, and behavioral interventions as the mainstay approaches. A digital program aiming to tackle these conditions should ideally encompass all of them in an integrated way. The digital care program that was studied in this randomized controlled trial is primarily based on therapeutic exercise, managed and monitored by physical therapists (PTs), and delivered through the use of a medical device that provides real-time feedback to the individual and relays information to the PT. This component is complemented with educational materials and behavioral health components also delivered digitally. Importantly, bi-directional communication tools were also developed, allowing for the establishment of an effective therapeutic alliance between the individual and the healthcare professional.
Designing the Study
In prior studies, we had compared digitally-delivered programs against in-person PT in a post-surgery scenario, and found greater improvements in the digital group. However, in this group, total treatment time was also higher, because the digital nature of the program allowed participants to do exercise sessions whenever and wherever they wanted. While this is an inherent advantage of digital care programs, it is also a potential source of bias towards the digital group.
In this study, we aimed to compare a digitally-delivered multimodal care program for the management of chronic low back pain against in-person physical therapy (PT). This time, however, we wanted to specifically understand how such a program would compare with in-person PT while controlling for total treatment time. Given that both digital and in-person programs are based on the same principles (mainly therapeutic exercise) and that both are managed by PTs, there would be no reason to assume that outcomes would be different between groups, for a similar treatment intensity. However, such assumptions still needed to be proven. Proving as much would help to further establish the value of digital care pathways as viable alternatives for the management of chronic low back pain in particular, and MSK conditions in general.
Finding the Right Partner
Randomized clinical trials are always challenging for all parties involved—participants, research centers, and sponsors alike. A clear alignment and close collaboration between sponsors and investigators on the research sites is therefore paramount to ensure the success of such a trial. In this trial, the collaboration between the sponsor and research site arose from a common belief, shared by both the PI at Emory (Dr. Cui Di) and the clinical lead on the sponsor side (Dr. Fernando Correia), that digital care pathways can hold the key to more sustainable healthcare delivery models. Moreover, Emory Spine Center, being a leading institution in the management of spine conditions, had both volume to meet the enrollment targets and the necessary expertise to deliver high-quality care to the participants.
Recruitment and Study Conduction
Launching and running a clinical trial involving an in-person and a digital arm during the pandemic was certainly challenging, in many foreseen and unforeseen ways. We faced severe delays in study setup (all non-essential clinical activities were suspended for several months), participant recruitment, and overall study duration, but we ultimately succeeded in driving the study to completion.
From the research site and sponsor sides, this endeavor required several adaptations to training, launching, and data monitoring activities, but was facilitated by the use of an electronic Data Capture System (Castor EDC).
On the participant side, we had many participants agreeing to participate in the study, but only if they were included in the digital group. This, of course, led to a high number of screening failures, but was also a clear indication of the acceptance of digital interventions brought about by the pandemic.
Study Results
Despite the many challenges faced during the study, we were able to answer the research question satisfactorily. We found no differences between primary or secondary outcomes between both groups, and also no differences between treatment intensity. These results contribute to strengthening the case towards progressive adoption of digital health solutions by showing that digital care programs can be viable alternatives to in-person care, with similar outcomes when controlling for treatment time.
We also observed a lower dropout rate in the digital group, probably resulting from a combination of: a) reduction of skepticism around digital solutions brought about by the pandemic; b) fear of contamination in in-person settings during the pandemic; c) restrictions to in-person visits or circulation directly caused by the pandemic; d) time and travel constraints in the in-person group (a known issue in in-person interventions). Still, these results show how digital solutions can be viable alternatives which are not restrained by some of the limitations inherent to in-person care.
Expectations for the Future
It is our belief that this and other studies—by our group and many others—may help pave the way to a more generalized adoption of digital care pathways, which do hold significant promise in improving access to high-quality care in a more affordable and scalable way. Subsequent studies should also focus on trying to understand who the best candidates for digital care pathways are, and what factors contribute to the success of these interventions. This will help providers develop hybrid care models that can cater to the needs of specific populations, while deploying resources efficiently.
Conflicts of Interest
The author of this blog post is the medical director of the study sponsor.
Follow the Topic
-
npj Digital Medicine

An online open-access journal dedicated to publishing research in all aspects of digital medicine, including the clinical application and implementation of digital and mobile technologies, virtual healthcare, and novel applications of artificial intelligence and informatics.
Related Collections
With Collections, you can get published faster and increase your visibility.
Digital Health Equity and Access
Publishing Model: Open Access
Deadline: Mar 03, 2026
Evaluating the Real-World Clinical Performance of AI
Publishing Model: Open Access
Deadline: Jun 03, 2026






Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in