Exploring Paths from Childhood Adversity to Adult Mental Health Challenges
Published in General & Internal Medicine and Behavioural Sciences & Psychology

The link between childhood adversity and adult mental health
Adverse childhood experiences, which include physical and sexual abuse, having parents who misuse substances, and witnessing violent crime, occur in up to half of children before age 18. Early exposure to trauma can have long-lasting effects on an adult’s mental health, increasing the odds of developing a substance use disorder, mood or anxiety disorder, or both. We found that people with these mental health conditions reported experiencing more adverse childhood events and lacking protective factors, such as close family connections, that can mitigate their harms.
There are multiple possible avenues through which people may develop both a substance use disorder and a mood or anxiety disorder following exposure to childhood adversity. For example, people who use substances to cope with depression or anxiety that stems from their exposure to trauma are at increased risk of developing a substance use disorder. This is often called the self-medication hypothesis, as individuals may be using substances to temporarily alleviate the symptoms of their mood or anxiety disorder. People with a substance use disorder could also develop a depressive or anxiety disorder due to the pharmacological and environmental effects of substance misuse. This is referred to as a substance-induced psychiatric disorder. Both these hypotheses have received empirical support, but it is not clear which may be more important.
Here we use a large diverse sample enriched for substance use disorders to test the two hypotheses to determine which accounts for more of the harmful effects of adverse childhood experiences on adult mental health. We analyzed data from a large sample of Black and White participants and in both found greater support for the self-medication hypothesis than that mood and anxiety disorders were substance-induced. Despite a strong direct association between adverse childhood experiences and the development of a mood or anxiety disorder, little of the association was explained by substance misuse. In contrast, a larger proportion of the association between childhood adversity and the development of substance dependence was explained by a preceding mood or anxiety disorder. Together, these findings suggest that children exposed to adverse events may benefit from interventions that help them to develop coping skills and emotional resilience, which could reduce their risk of future mood, anxiety, and substance use disorders.
How do genetic factors interact with childhood adversity to impact adult mental health?
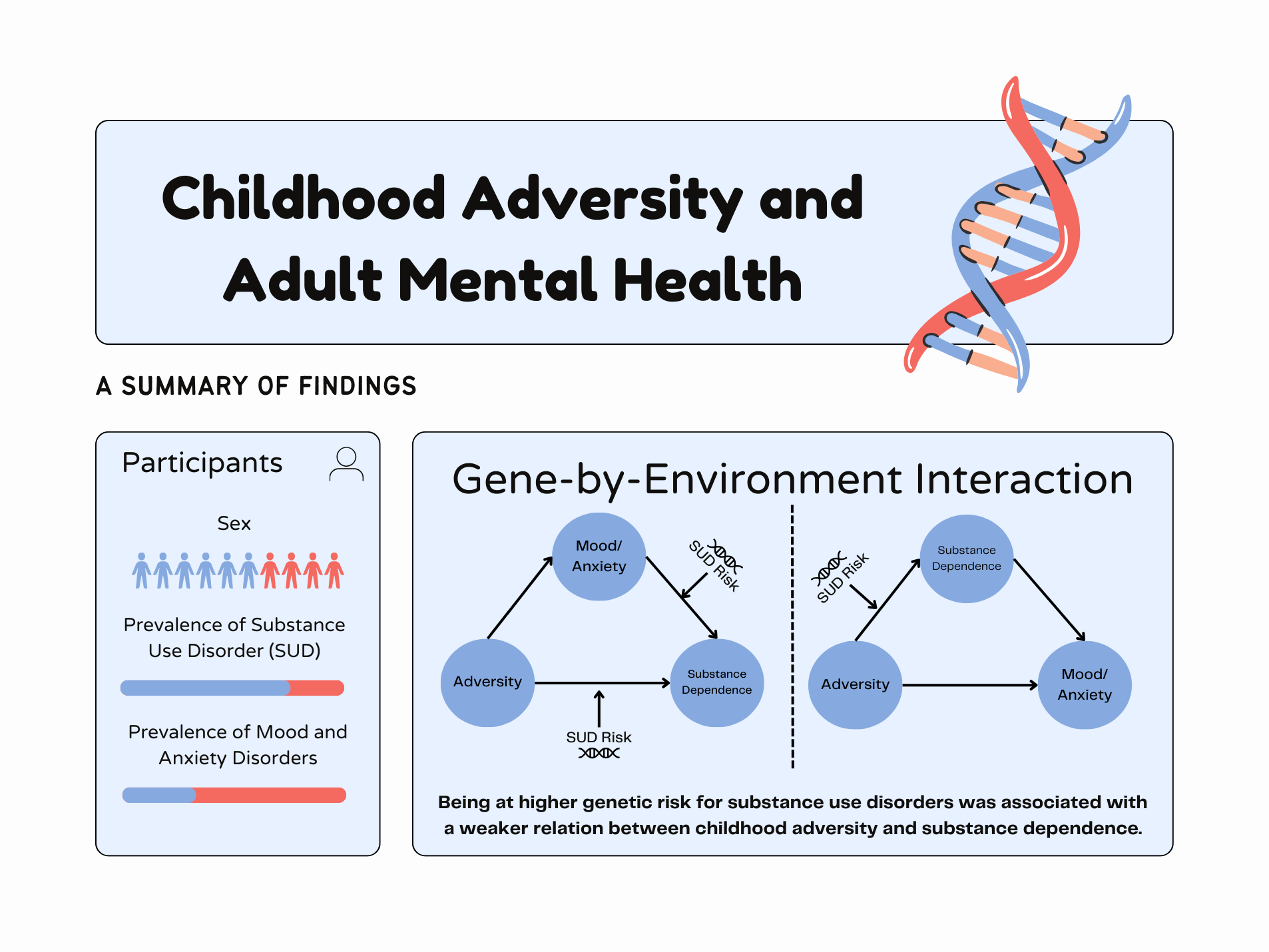
Despite the well-established link between childhood adversity and adult mental health disorders, many people with adverse childhood experiences do not develop a mental health or substance use disorder. The different outcomes among people may partially reflect genetic differences, as people vary in their genetic predisposition for developing these disorders. Among participants in our study, those with more genetic risk variants for substance use disorders were more likely to have a substance use disorder and at greater risk of developing a mood or anxiety disorder. A similar association was found among people with higher genetic risk for mood or anxiety disorders. Genetic risk for substance use disorders and mood or anxiety disorders also correlated with a higher likelihood of experiencing childhood adversity. Thus, we tested whether genetic differences in risk for these disorders interacted with adverse childhood experiences to influence adult mental health outcomes.
In contrast to what we anticipated, the association between childhood adversity and substance dependence was stronger among people with lower genetic risk for developing a substance use disorder. This finding suggests that among individuals at lower genetic risk for a substance use disorder, environmental adversity plays a greater role in determining their risk of developing substance dependence. In contrast, among people at higher genetic risk for a substance use disorder, the effect of childhood adversity on developing substance dependence is outweighed by the impact of genetics.
The interaction that we observed between a person’s genetic predisposition and their childhood environment underscores that there are multiple pathways that can lead to developing a substance use disorder following exposure to adverse childhood experiences. A better understanding of these pathways and their interactive or additive effects may help to identify people at risk early in life, and to design interventions to promote skills, such as emotion regulation, to help reduce their risk of developing a mental health disorder in adulthood.
Conclusion
We found that adverse childhood experiences were associated with an increased risk of both mood or anxiety disorders and substance use disorders. However, more of the association with substance use disorders was explained by a preceding mood or anxiety disorder, while the association with mood and anxiety disorders was due largely to a direct effect of childhood adversity. Genetic risk for substance use disorders also interacted with childhood adverse experiences to influence the risk of developing substance dependence. Because there are multiple pathways to the development of mental health conditions following exposure to childhood adversity, regular screening for adverse childhood experiences and targeted interventions to improve emotional regulation and other coping skills, may help to reduce the harmful impacts of childhood adversity. Given these findings, greater priority should be placed on both reducing children’s exposure to early traumatic experiences and increasing their access to protective factors, which may help prevent the need for future mental health interventions.
Follow the Topic
-
Nature Human Behaviour

Drawing from a broad spectrum of social, biological, health, and physical science disciplines, this journal publishes research of outstanding significance into any aspect of individual or collective human behaviour.
Your space to connect: The Psychedelics Hub
A new Communities’ space to connect, collaborate, and explore research on Psychotherapy, Clinical Psychology, and Neuroscience!
Continue reading announcement


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in