Hyperbaric Oxygenation, post-COVID syndrome and Speckle Tracking Imaging
Published in Healthcare & Nursing
Post-COVID complications have been widely studied, and it is evident that the virus can affect multiple organs, including the heart. Patients recovering from COVID-19 often present with cardiac manifestations, such as myocarditis, myocardial injury, and impaired cardiac function.
The pathophysiology responsible for the occurrence of subclinical myocardial dysfunction in patients with post-COVID syndrome remains not fully clear. Let's explore the intriguing question of why some patients with post-COVID complications exhibit reduced global longitudinal strain [GLS]. The development of cardiac dysfunction in post-COVID syndrome is thought to involve multiple mechanisms, one of which is the binding of viral spike S protein with ACE2 receptors, which are present on the surface of myocardial cells. This interaction between viral particles and ACE2 receptors has the potential to cause direct damage to the myocardium, resulting in impaired cardiac function.
We evaluated GLS that is transmural strain. Myocardial wall is composed of 3 myocardial layers, endocardium, epicardium and mid-layer and strain can be calculated in each of them [1], that may provide further insights into post-COVID complications. Which layer is responsible for decrease of GLS in post-COVID patients? In which myocardial layer myocytes are more vulnerable regarding the binding by viral particles? As we can see at Figure 1, endocardial strain is the highest and the epicardial strain is the lowest.
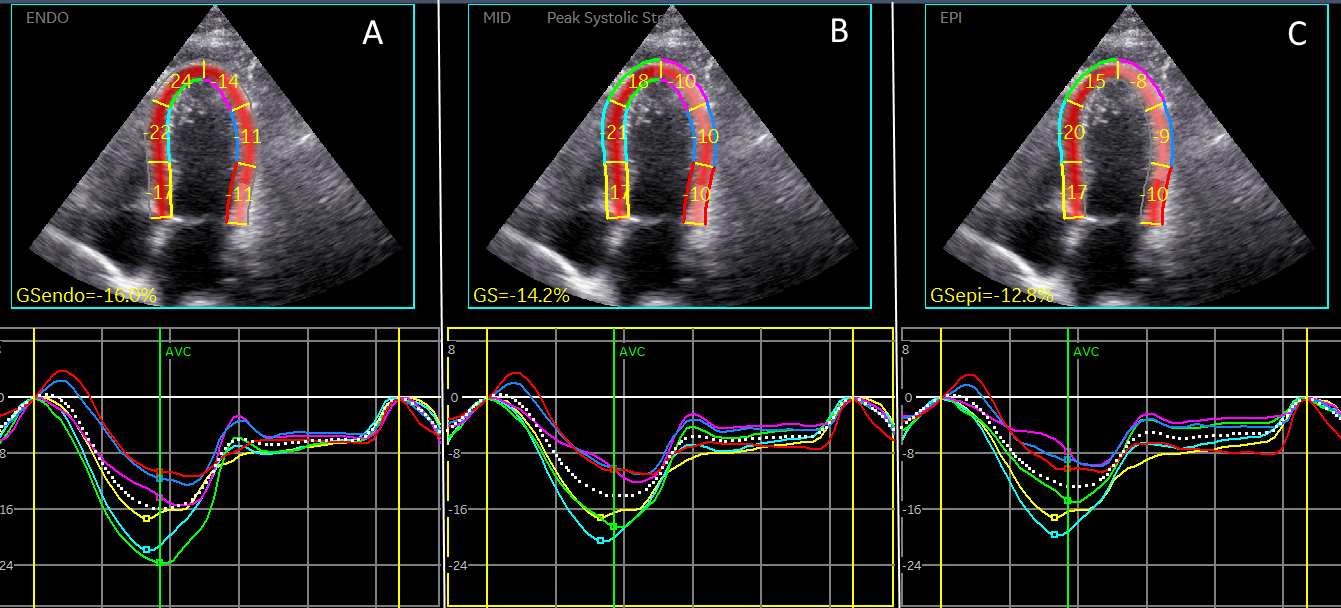
Figure 1. Strain in 3 myocardial layers in patient with post-COVID syndrome. Apical 4-chamber view.
- Endocardial strain.
- Mid-layer strain
- Epicardial strain.
The inflammatory response triggered by the viral infection can result in myocardial inflammation and fibrosis. These processes can further compromise myocardial contractility, ultimately leading to reduced GLS. Additionally, the indirect effects of systemic inflammation, such as cytokine storm, can contribute to myocardial injury and dysfunction. It's worth noting that the observed reduction in GLS may not be exclusive to COVID-19 but rather a common feature of viral myocarditis in general. Similar findings have been reported in other viral infections, highlighting the potential overlap in the mechanisms underlying myocardial injury across different viral etiologies. None of our patients exhibited symptoms consistent with myocarditis or myocardial infarction, suggesting that these conditions were not the underlying causes of cardiac dysfunction in post-COVID syndrome.
Myocardial involvement in inflammatory myocardial diseases usually epicardial and mid-myocardial and strain is decreased at basal and mid-ventricular segments [2]. In coronary artery disease endocardial layer is damaged first. What can we anticipate discovering in post-COVID patients who do not exhibit clinical signs of myocarditis or myocardial infarction? One area of interest is left atrial strain. Left atrial function is crucial for optimal cardiac performance, and strain analysis provides valuable insights into its contractile properties. Recent studies have shown that patients with post-COVID complications tend to have reduced left atrial strain compared to healthy individuals [3]. This reduction of strain suggests a potential impairment in left atrial function, which can have important implications for patients' overall cardiovascular health. Tropism of SARS-CoV-2 virus was found in the cardiomyocytes of the left atrium [4]. in this study we didn’t analyzed left atrial strain that can also help to elucidate the kind of cardiac dysfunction in patients with post COVID syndrome, Figure 2.
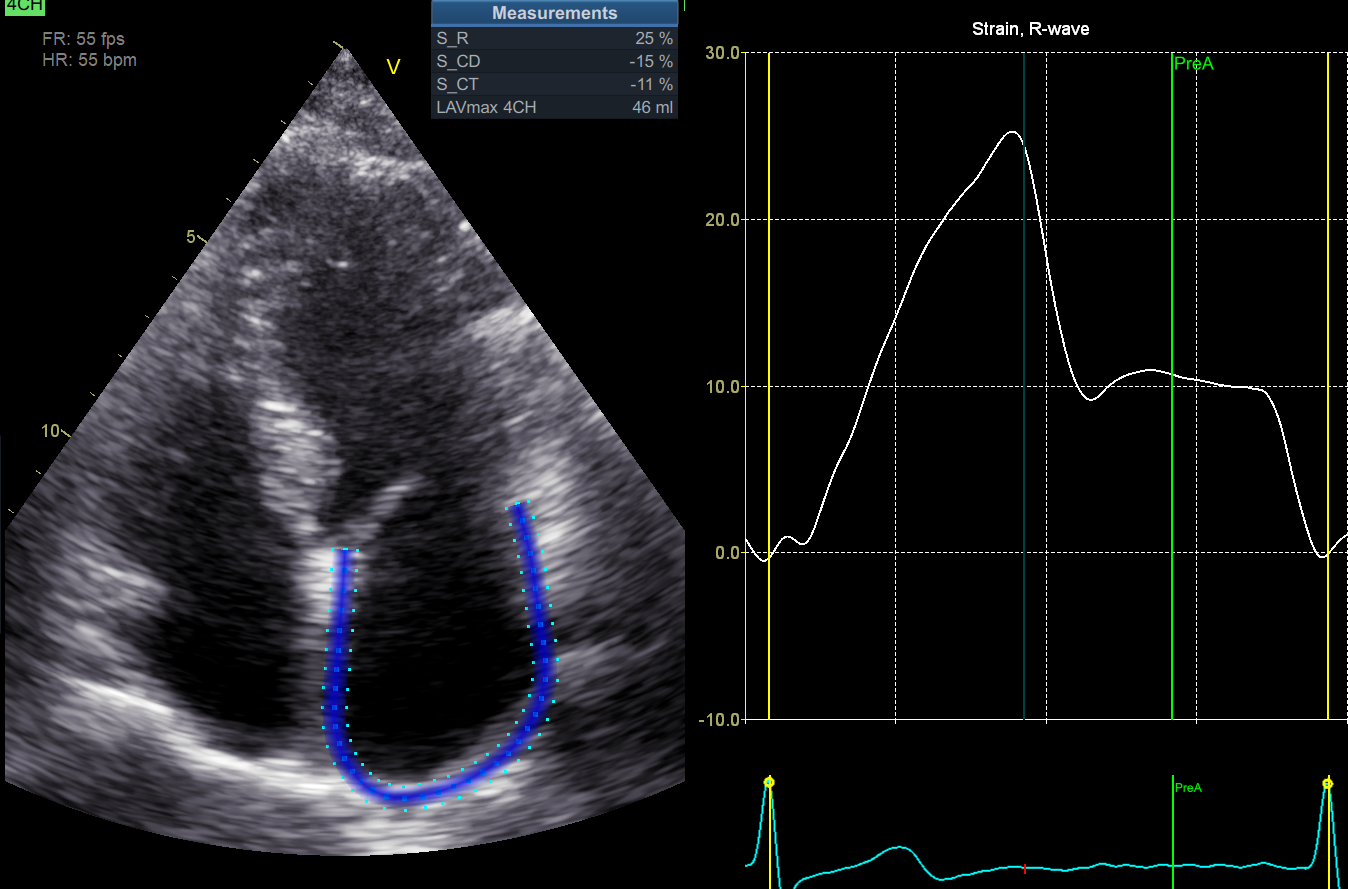
Figure 2. Left atrial strain of the patient with post-COVID syndrome.
Another report showed tropism of the virus towards endocardial endothelial cells [5] that is anatomically different from the damage due to myocarditis. ACE2-receptors also were found in epicardial adipocytes [6] that can be responsible for the decreased epicardial strain.
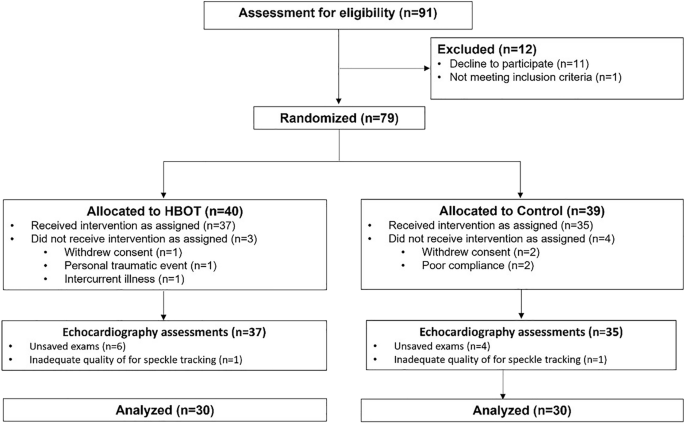
At which level hyperbaric oxygen therapy, [HBOT], can help? Regenerative and anti-inflammatory effect of hyperbaric oxygenation due to activation of natural myocardial healing processes seems a most relevant mechanism in the cases of persistent inflammation and long-term unremitting damage. HBOT has been used for various medical conditions and has shown beneficial effects with regards to brain damaged and cognitive decline related to post-COVID complications. HBOT improved cognitive functions, mental performance and fatigue. One notable aspect in the improvement in fatigue and physical functions can be related to the GLS improvement observed in patients undergoing hyperbaric oxygenation that we observed in the current study as well as in previous our study [7]. HBOT increases the oxygen supply to tissues, including the heart, by delivering oxygen at higher oxygen pressures than normal atmospheric conditions. This approach aims to improve tissue oxygenation, enhance cellular metabolism, induce angiogenesis (generation of new blood vessels) and promote cardiac-tissue healing.
In the context of post-COVID complications, HBOT may offer several benefits. Firstly, it can help mitigate the oxygen supply-demand mismatch that occurs in damaged or inflamed tissues. By increasing the availability of oxygen, HBOT may improve myocardial function and promote the recovery of cardiac tissue. Secondly, HBOT has anti-inflammatory properties. COVID-19 is characterized by an excessive inflammatory response, and this inflammation can contribute to cardiac damage and dysfunction. HBOT has been shown to reduce inflammation by modulating immune responses and decreasing the production of pro-inflammatory molecules. By mitigating inflammation, HBOT may help protect the myocardium and improve GLS. Thirdly, HBOT can promote tissue repair, stem cells proliferation and angiogenesis. Oxygen is essential for tissue healing and the formation of new blood vessels. By enhancing oxygen delivery to damaged cardiac tissue, HBOT may stimulate the regeneration of healthy myocardium.
In conclusion, left atrial strain and myocardial layer strain analysis are important elements in the assessment of patients suffering from post-COVID complications. Monitoring left atrial function and evaluating strain across different myocardial layers can provide valuable information for diagnosing and managing these complications effectively. While the precise mechanisms behind the reduced GLS in post-COVID patients are not yet fully understood, the binding of viral particles to ACE2 receptors and the subsequent inflammatory response likely play a significant role. HBOT is those far the only intervention proved in randomized, placebo control trial to improve cognitive function, mental performance and cardiac function of patients suffering from post-COVID unremitting complications, with our study reporting improvement in GLS. By enhancing tissue oxygenation, reducing inflammation, angiogenesis, improve mitochondrial function and stem cells proliferation and migration, HBOT can contribute to the recovery of myocardial functions. However, more research is needed to validate these findings and to determined the optimal HBOT protocol and who are the patients that can benefit the most. It should be noted, that any treatment if consider, should be given by professional team using medical hyperbaric facility that can delivered the exact protocol and quality assurance used in the study.
References:
- Leitman M, Lysiansky M, Lysyansky P, Friedman Z, Tyomkin V, Fuchs T, Adam D, Krakover R, Vered Z. Circumferential and longitudinal strain in 3 myocardial layers in normal subjects and in patients with regional left ventricular dysfunction. J Am Soc Echocardiogr. 2010 Jan;23(1):64-70. doi: 10.1016/j.echo.2009.10.004. PMID: 20122496.
- Leitman M, Bachner-Hinenzon N, Adam D, Fuchs T, Theodorovich N, Peleg E, Krakover R, Moravsky G, Uriel N, Vered Z. Speckle tracking imaging in acute inflammatory pericardial diseases. Echocardiography. 2011 May;28(5):548-55. doi: 10.1111/j.1540-8175.2010.01371.x. Epub 2011 May 4. PMID: 21539601.
- ZeinElabdeen SG, Sherif A, Kandil NT, Altabib AMO, Abdelrashid MA. Left atrial longitudinal strain analysis in long Covid-19 syndrome. Int J Cardiovasc Imaging. 2023 May;39(5):939-944. doi: 10.1007/s10554-023-02801-5. Epub 2023 Feb 14. PMID: 36786877; PMCID: PMC9927057.
- Sakamoto A., Kawakami R., Kawai K., Gianatti A., Pellegrini D., Kutys R., Guo L., Mori M., Cornelissen A., Sato Y., et al. ACE2 (Angiotensin-Converting Enzyme 2) and TMPRSS2 (Transmembrane Serine Protease 2) Expression and Localization of SARS-CoV-2 Infection in the Human Heart. Arterioscler. Thromb. Vasc. Biol. 2021;41:542–544. doi: 10.1161/ATVBAHA.120.315229.
- Dolhnikoff M., Ferreira Ferranti J., de Almeida Monteiro R.A., Duarte-Neto A.N., Soares Gomes-Gouvêa M., Viu Degaspare N., Figueiredo Delgado A., Montanari Fiorita C., Nunes Leal G., Rodrigues R.M., et al. SARS-CoV-2 in cardiac tissue of a child with COVID-19-related multisystem inflammatory syndrome. Lancet. Child Adolesc. Health. 2020;4:790–794. doi: 10.1016/S2352-4642(20)30257-1.
- Salamanna F, Maglio M, Landini MP, Fini M. Body Localization of ACE-2: On the Trail of the Keyhole of SARS-CoV-2. Front Med (Lausanne). 2020 Dec 3;7:594495. doi: 10.3389/fmed.2020.594495. PMID: 33344479; PMCID: PMC7744810.
- Leitman M, Efrati S, Fuchs S, Hadanny A, Vered Z. The effect of hyperbaric oxygenation therapy on myocardial function. Int J Cardiovasc Imaging. 2020;36(5):833-40.
Follow the Topic
-
Scientific Reports

An open access journal publishing original research from across all areas of the natural sciences, psychology, medicine and engineering.
Related Collections
With Collections, you can get published faster and increase your visibility.
Reproductive Health
Publishing Model: Hybrid
Deadline: Mar 30, 2026
Women’s Health
Publishing Model: Open Access
Deadline: Feb 28, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in