Impact of HIV exposure without infection on hospital course and mortality among young children in sub‑Saharan Africa: a multi‑site cohort study
Published in Biomedical Research, General & Internal Medicine, and Paediatrics, Reproductive Medicine & Geriatrics

Story behind the research:
This was a secondary data analysis from the Childhood Acute Illness and Nutrition (CHAIN) cohort study. The CHAIN study was a multi-country study that aimed to build an evidence base for the care of acutely ill malnourished children. In this study, I had an opportunity to collect data and provide clinical care to the study participants. As we kept discussing different participants in our study calls, we realized that the trajectory of children born to HIV-positive mothers, even when they had no HIV infection, was seemingly different from that of children born to HIV negative mothers.
Fast-forward, when I was doing my master’s degree in Public Health, I needed a research topic for my master’s dissertation. I wanted to compare different clinical outcomes among HIV positive children vs. HEU children vs. HIV-unexposed children. On further discussion with my research supervisor, it became clear that the outcomes of HIV positive children were known, and the knowledge gap was among the HEU vs HUU children. After identifying the research topic, I engaged my mentor (senior author), who reviewed my concept and supported me in getting the data request approved by the CHAIN Network. I did the data analysis, wrote my dissertation, and it was approved.
After surmounting that hurdle, the next step was transforming all the work from dissertation to manuscript format. That took some time. The senior author did extensive reviews, which necessitated changing a few things. The next step was circulating the draft to the co-authors, who provided detailed comments. Some comments required significant changes in analysis strategies, others required a change in the flow of content. It took me about one and a half years to transform the dissertation document into the first draft manuscript submitted to a scientific journal!
Why is the research valuable?
Successful Prevention of Mother to Child Transmission(PMTCT) interventions have resulted in a significant decrease in children infected with HIV and a high number of children who are HIV-exposed but not infected (HEU). In 2022, there were an estimated 15.4 million HEU children, with close to 90% residing in sub-Saharan Africa. Several studies have demonstrated an increased risk of morbidity and mortality among HEU children compared to HIV unexposed, uninfected (HUU) children. However, the drivers of mortality and morbidity among the HEU children remain unclear, which impedes efforts to improve outcomes in this vulnerable group. There have been few studies examining risk factors for poor outcomes among HEU children. In this study, the examined associations between HIV-exposure and mortality, nutritional status, illness severity at admission, hospital length of stay, and utilization of hospital resources. This analysis provides insight into the drivers of poor outcomes among HEU children. This contributes to the evidence for formulating interventions and further research for this vulnerable group of children.
What did the authors do?
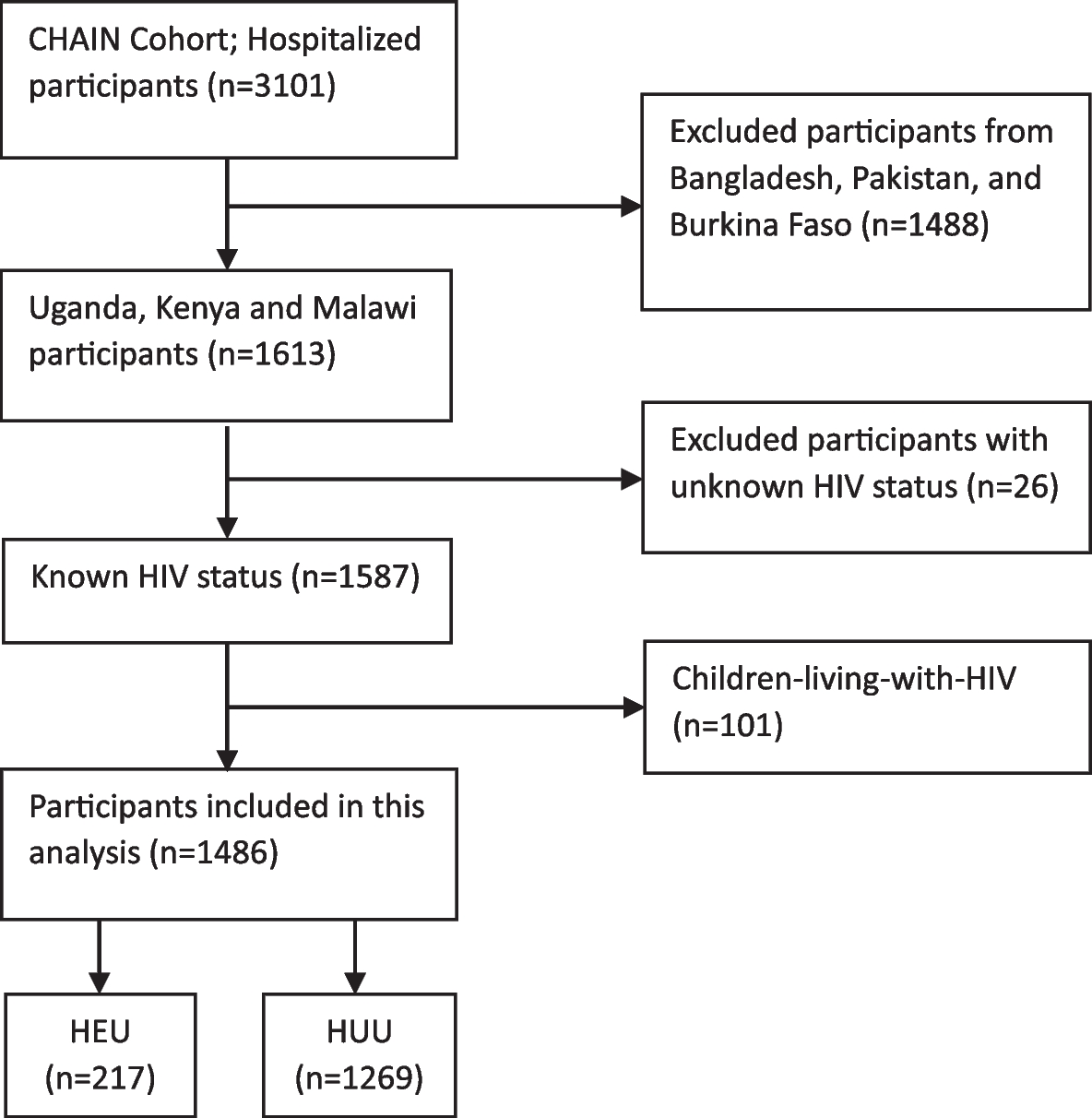
We did a secondary analysis of the CHAIN cohort study data. We analysed data from five CHAIN sites: Kampala (Uganda), Blantyre (Malawi), Migori (Kenya), Mbagathi (Nairobi, Kenya), and Kilifi (Kenya). A child was considered HEU if their mother was known to be living with HIV while pregnant, and the child’s confirmatory HIV test was negative, and/or a child < 18 months old had positive HIV rapid tests and the child’s confirmatory HIV DNA-PCR test was negative. We examined inpatient mortality and death within 30 days of admission among HEU children using logistic regression and survival analysis, respectively. We compared nutritional status (wasting and stunting), illness severity (high and low scores), and hospital length of stay (short or prolonged) using logistic regression. To assess the effect of HIV exposure on the occurrence of daily danger signs and resource utilization (oxygen use, nasogastric tube use, and antibiotic switch), days with any danger sign or the use of a specific resource were counted. A zero-inflated negative binomial regression model was applied because the days with a danger sign or use of any resource had leading zeros. In all the regression models, adjustment for appropriate child, caregiver, and household-level variables was done.
What did the researchers find?
HEU children had a higher risk of inpatient and 30-day mortality, were at an increased risk of wasting and stunting, and required a longer hospital stay, as compared to HUU children. There was no significant association between HIV exposure and illness severity, and no significant differences in the frequency and types of danger signs reported, as well as no differences in the requirement of hospital resources.
What are the implications of this study?
HEU children under 2 years of age are uniquely vulnerable to dying during hospitalization and the early post-discharge period, regardless of nutritional status. HEU children may be more vulnerable to undernutrition due to inadequate feeding practices, driven by a low prevalence of breastfeeding and a higher household food insecurity. The presence of sub-clinical infection(s) or acquisition of nosocomial infection(s) may have been more likely to complicate recovery among HEU children, resulting in prolonged hospital stay. Prolonged hospitalization not only places HEU children at increased risk for hospital-acquired infection and emergence of antimicrobial resistance but also increases the financial burden on the family, which further complicates the economic situation of these households.
Are there broader implications or applications of these findings? If so, what are they? What are the obvious limitations or caveats?
Our findings suggest that HEU children should be considered a high-risk population during hospitalization and in the early post-discharge period, regardless of perceived illness severity and nutritional status at admission
Additional biological factors that we were unable to quantify in our analysis, such as intestinal dysbiosis, metabolic derangements, and/ or subclinical infections such as cytomegalovirus, could have also contributed to wasting and the poor outcomes observed among HEU children.
What are the obvious next questions or steps to take this further? Are there aspects of the research that could be made stronger?
Longitudinal studies, preferably beginning in pregnancy, are likely to be required to understand how perinatal HIV exposure in the absence of infection compromises early childhood health. Identifying biological drivers of increased hospital mortality, wasting, and prolonged hospitalization among HEU children is essential to develop clinical care guidelines tailored to support this unique and vulnerable population.
Follow the Topic
-
BMC Medicine

This journal publishes outstanding and influential research in all areas of clinical practice, translational medicine, medical and health advances, public health, global health, policy, and general topics of interest to the biomedical and sociomedical professional communities.
Related Collections
With Collections, you can get published faster and increase your visibility.
Weight loss interventions and their health impacts
BMC Medicine is calling for submissions to our new Collection on weight loss interventions and their health impacts, emphasizing a variety of strategies, including dietary changes, physical activity, pharmacological treatments, and surgical options. We encourage submissions that explore the long-term effects of these interventions, adherence challenges, and strategies to address health inequities. The goal is to advance understanding and improve outcomes in weight management and overall health.
Weight loss interventions encompass a wide range of strategies aimed at reducing body weight and improving health outcomes. These interventions can include dietary changes, increased physical activity, pharmacological treatments, and surgical options such as bariatric surgery. As the global prevalence of obesity and related comorbidities continues to rise, understanding the efficacy and mechanisms of various weight loss interventions becomes increasingly crucial for public health. This Collection seeks to explore the diverse methodologies and outcomes associated with weight loss interventions, offering insights into their impacts on both individual and population health.
The significance of this research is underscored by the growing body of evidence linking obesity to numerous chronic health conditions, including diabetes, cardiovascular diseases, and certain types of cancer. Advances in pharmacological treatments, such as SGLT2 inhibitors and GLP-1 agonists, have emerged as promising options for weight management, demonstrating not only weight loss but also improved metabolic health. There are, however, challenges and limitations related to drug availability, healthcare delivery, and long-term treatment adherence with rapid weight gain when stopping treatment. Additionally, integrating behavioral strategies with nutritional and physical activity interventions has shown potential in enhancing adherence and long-term success. By further investigating these modalities, we can develop comprehensive approaches that address the multifactorial nature of obesity.
Continued research in this domain may yield innovative strategies that harness technology, such as mobile health applications and telehealth, to support weight loss interventions. As we deepen our understanding of the genetic, environmental, and behavioral factors influencing obesity, personalized interventions tailored to individual needs could emerge. This progress may lead to improved health outcomes, reduced health inequities, and ultimately a shift in the paradigm of obesity treatment and prevention.
We are looking for original manuscripts on topics including, but not limited to:
•Clinical trials investigating interventions for weight loss to promote health
•Real-world data on long-term effects and challenges of weight loss interventions
•Factors affecting long-term adherence to weight-loss or weight maintenance interventions
•Challenges and inequities in access to weight loss interventions
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
This Collection supports and amplifies research related to SDG 3: Good Health and Well-being.
Publishing Model: Open Access
Deadline: May 07, 2026
Climate change and human health
BMC Medicine is calling for submissions to our new Collection on the health impacts of climate change. The relationship between global warming and human health is increasingly becoming a focal point in public health research. Rising temperatures, shifting weather patterns, and extreme weather events are projected to have profound effects on various health outcomes. From increased prevalence of vector-borne diseases to heightened risks of heat-related illnesses, the health implications of climate change are vast and multifaceted. This Collection aims to explore the direct and indirect impacts of global warming on health, examining how these changes affect vulnerable populations and health systems worldwide.
Understanding the implications of global warming for human health is crucial for developing effective public health strategies and interventions. Recent research has highlighted the links between climate change and a variety of health issues, including air pollution, water-borne diseases, and undernutrition. Advances in climate modeling and epidemiological studies have enhanced our ability to predict health outcomes related to climate change, providing invaluable insights that can inform policy decisions and health care planning.
Continued research in this area may lead to innovative solutions to mitigate the health impacts of climate change. For example, interdisciplinary approaches that integrate climate science, public health, and social determinants of health could reveal new pathways for adaptation and resilience. Future studies may also focus on the development of health infrastructure designed to withstand climate-related stresses, thus improving community health outcomes in an era of global warming.
We are considering manuscripts on, but not limited to the following topics:
-Impact of air pollution on health
-Heat-related illnesses
-Water-, and vector-borne diseases in a warming world
-Social determinants of health and climate vulnerability
-How health systems and infrastructure may be affected by climate change
-Nutrition and health in the context of climate change
-Impacts of climate change on non-communicable diseases
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
This Collection supports and amplifies research related to SDG 3 (Good Health and Well-being) and SDG 13 (Climate Action).
Publishing Model: Open Access
Deadline: Mar 02, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in