MCL1 regulates AML cells metabolism via direct interaction with HK2. Metabolic signature at onset predicts overall survival in AMLs’ patients
Published in Cancer

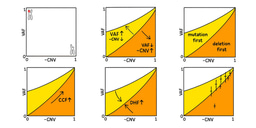
- Acute myeloid leukemic cells feature a lower spare respiratory capacity (SRC) and glycolytic capacity as compared to hematopoietic precursors (day 7, promyelocytes).
- On the base of Proton Leak (PL) values AML blasts can be grouped in two well defined populations, high PL associates with FLT3 mutations. The AML group with blasts presenting high PL or high basal OXPHOS plus high SRC levels had shorter overall survival time and significantly overexpressed myeloid cell leukemia 1 (MCL1) protein
- MCL1 directly binds to Hexokinase 2 (HK2) forming a complex with VDAC (mitochondrial porin) on the outer mitochondrial membrane: the disruption of this complex, by early Mcl-1 inhibition, might rescue those patients
We are particularly interested in the metabolic reprogramming as a basic feature in Acute myeloid leukemia (AML) development and response to therapy. In particular, given the advanced age and the frequent complex comorbidity profile of patients, we search for therapies with a low toxicity profile. Gaining information on the cancer-specific cellular metabolism at onset could lead to the development of new therapies targeted on specific metabolic alterations that would prevent the emergence of therapy resistant clones, minimizing resistance and early disease relapse. Looking for early indicators supporting a tailored metabolic targeted therapy in AML patients we found that it is possible to acquire, at the time of diagnosis, and from the bulk of blast cells, an early information on a subgroup of poor prognosis and no responding AML patients, who need a different therapeutic approach. Overall, phenotypic features reflect distinct metabolic backgrounds among hemopoietic stem cells at different stages of differentiation, leukemia stem cells and proliferating AML blasts. To produce energy, the electrons from substrates oxidation are passed through the respiratory chain on the inner mitochondrial membrane. The flux is maintained by proton pumping against gradient from the inner mitochondrial matrix to the intermembrane space via the respiratory chain complexes I, III, and IV. This generates a proton gradient across the inner mitochondrial membrane, which is necessary for ATP synthase to phosphorylate ADP by proton consumption. However, no living cell converts all the energy of the proton gradient to ATP. Oxidative phosphorylation is incompletely ‘coupled’, since protons can ‘leak’ across the inner membrane without ATP synthesis. Leaked protons link reactive oxygen molecules to produce H2O and thermic dispersion. This evolutionary conserved proton leak pathway regulates physiological processes like thermogenesis and reactive oxygen species (ROS) reduction. Thus the high mitochondrial superoxide production from leukemic high metabolic rate is balanced by PL that minimize oxidative damage. In leukemic cells uncoupled mitochondrial respiration (lesser mitochondrial ATP production due to PL) forces the cells to recur to glycolysis for energy production, in the absence of alterations in the oxidative capacity. This metabolic peculiarity allows for more material for anabolic tumoral growth and enhanced resistance to stress via PL effect. The differential regulatory functions of mitochondria between normal and leukemic precursors play a fundamental role in regulating redox stress response. Given the central role of glycolysis and glucose uptake in association with mitochondrial function in cancer cells’ dynamics, glycolytic limiting enzymes hexokinases (HK) represent essential players in leukemic metabolism, and in particular in mitochondrial function and stability. Mitochondria are basilar in leukemic cell metabolism. Leukemic cells use various metabolic pathways simultaneously in a highly flexible way: glucose derivatives, lipids and amino acids fuel OXPHOS energy production and provide protection against mitochondrial membrane permeabilization, leading to apoptosis, via PL equilibrating effect. The aberrant overexpression of BCL2 and related BH3 antiapoptotic family genes helps to stabilize mitochondria, and is associated with tumorigenesis and drug resistance in various cancers. The AML group with blasts presenting high PL or high basal OXPHOS plus high SRC levels had shorter overall survival time and significantly overexpressed myeloid cell leukemia 1 (MCL1) protein. We demonstrate that MCL1 directly binds to Hexokinase 2 (HK2) on the outer mitochondrial membrane (OMM). Overall, these results suggest that high PL levels and high SRC plus high basal oxphos at disease onset, arguably with the concourse of MCL1/HK2 action, are significantly linked with shorter overall survival time in AML. Our data describe a new function of MCL1 protein in AMLs’ cells: forming a complex with HK2 co-localizes to VDAC on the OMM, thus promoting glycolysis and OXPHOS, ultimately conferring metabolic plasticity and promoting resistance to therapy. The disruption of this complex, by early Mcl-1 inhibition, might rescue those patients.
Follow the Topic
-
Leukemia

This journal publishes high quality, peer reviewed research that covers all aspects of the research and treatment of leukemia and allied diseases. Topics of interest include oncogenes, growth factors, stem cells, leukemia genomics, cell cycle, signal transduction and molecular targets for therapy.


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in