Mucosa exposed to a warming atmosphere share risks faced by planetary vegetation
Published in Bioengineering & Biotechnology, Earth & Environment, and Biomedical Research
In today’s issue of Communications Earth & Environment, researchers report that thinning of mucosa in response to the mouth breathing of dry air delivers inflammatory stresses in human airways, potentially promoting chronic respiratory disease.
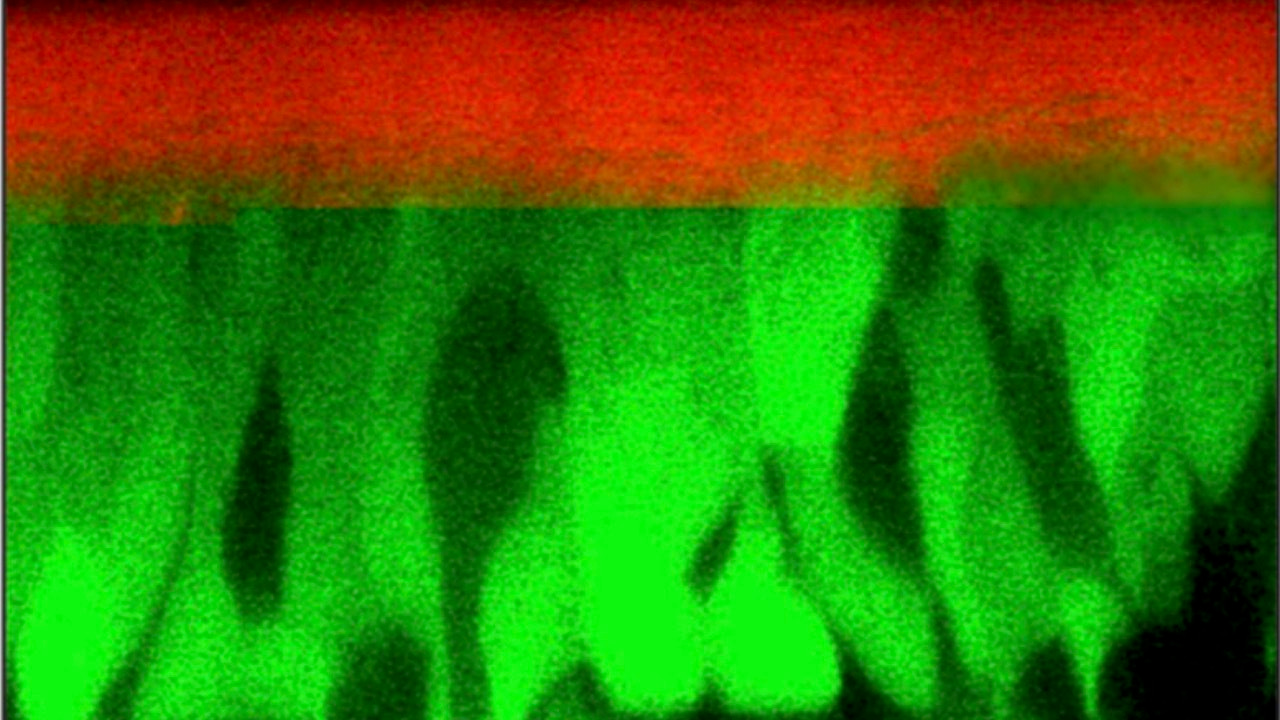
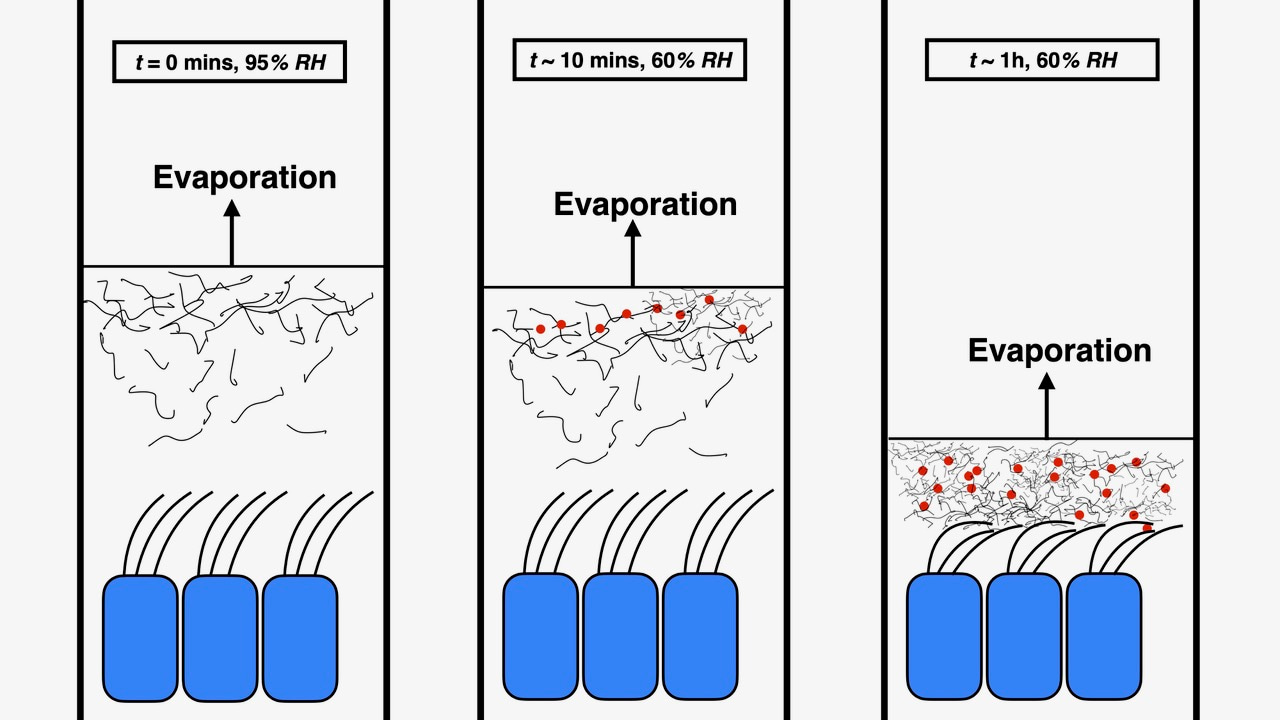
Using continuum mechanical analysis, and a combination of in vitro and in vivo experimental models, the authors find mucus thinning to be the consequence of an evaporative process called transpiration, by which evaporation from the surface of a leaf pulls water from distant roots. A useful hydraulic process that keeps the leaf hydrated in dry air, transpiration delivers damaging cellular compression when the air is too dry, potentially wilting the leaf. In their study, the researchers find that, in a similar fashion, mucus transpiration keeps airway mucus moist through the incessant evaporation required to humidify inhaled air, while inflaming airways above a threshold air dryness.
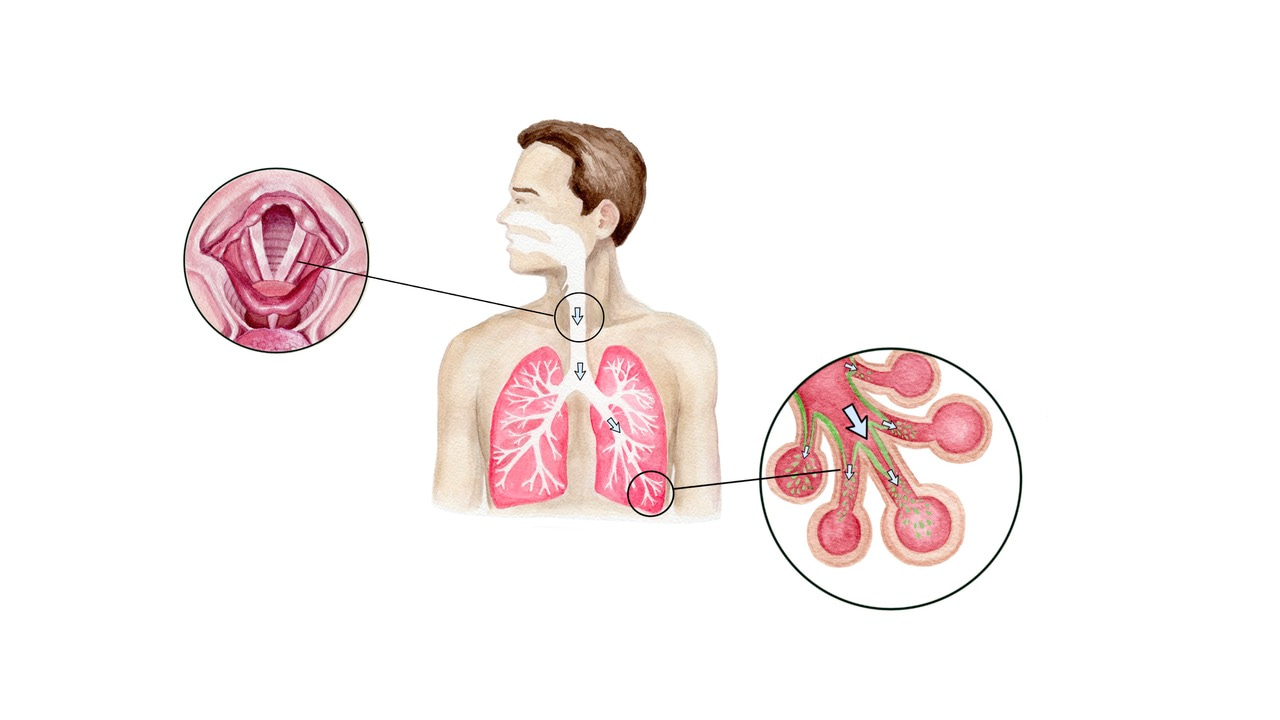
On mouth breathing, inhaled air humidification begins in the larynx. Artist drawing by Heejin Gregory
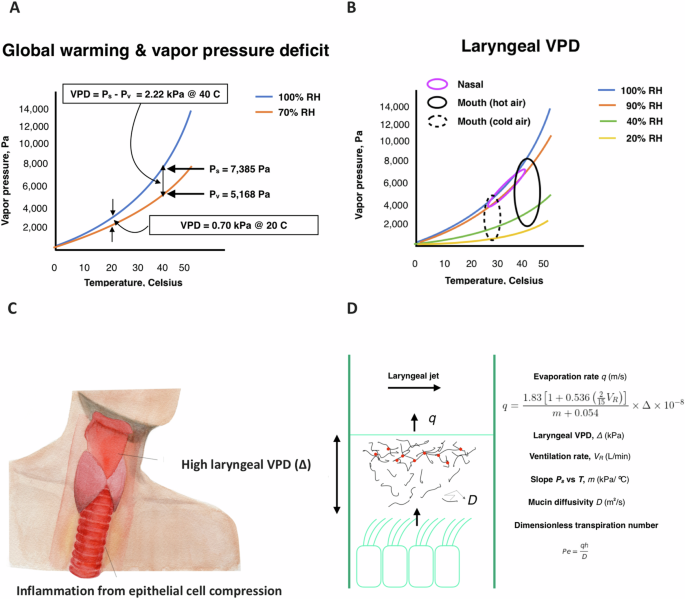
How dry is dry? Air with relative humidity (RH) less than 40% is generally considered to be dry. However, air possessing a temperature of 40oC with relative humidity as high as the earth’s average of 70% — or air at most any temperature and RH near the summit of Mount Everest — is also very dry. All of these conditions share in common high vapor pressure deficit (VPD) — a single thermodynamic variable that qualifies atmospheric dryness or “thirstiness.” VPD grows nearly exponentially in magnitude with increasing temperature at a fixed relative humidity. (It also grows at any temperature and relative humidity as altitude increases or air pressure decreases.) And since the average relative humidity over the surface of the earth has held constant at 70% over a century of global warming, VPD has long been rising at an accelerating rate.
From their theoretical and experimental models, the authors estimate VPD levels above which normal mouth breathing of air is moderately or severely inflammatory to human upper airways. Using climate model simulations, they then deduce that by the latter half of the century most of the Continental United States will be at moderate to severe risk of breathing inflammatory air.
Heightening the threat to human airways is the growing prevalence of chronic mouth breathing. Humans are natural nasal breathers. Among the benefits of nasal breathing is the humidification capacity of the nose. In most atmospheric conditions, air arrives in the human larynx during normal nasal breathing with a relative humidity of 90% or above. However, this is changing. Allergic rhinitis, obesity, and aging of the human population, all contribute to increased chronic mouth breathing. A recent study reports that, by the age of 12, 40% of children are chronic mouth breathers, a percentage that increases with age.
Humans also mouth breathe at high ventilation rate. Sufferers of allergic rhinitis and asthmatics who breathe with high ventilation rate air at 40oC-45oC and 70% RH have an elevated tendency to experience acute cough and bronchospasm, while those exposed to 25oC and 70% RH do not. Asthmatics who breathe cold air with high ventilation rate air also have an elevated tendency to cough and bronchospasm. Why is this? Mouth breathing heats very cold air inhaled air prior to the larynx, while does not appreciably humidify. The mouth breathing of cold air therefore delivers hot dry air into the larynx — similar to the mouth breathing of indoor air that is cooled in the summer, and heated in the winter. In all these cases high VPD air arrives in the larynx, increasing the likelihood of cough and bronchospasm.
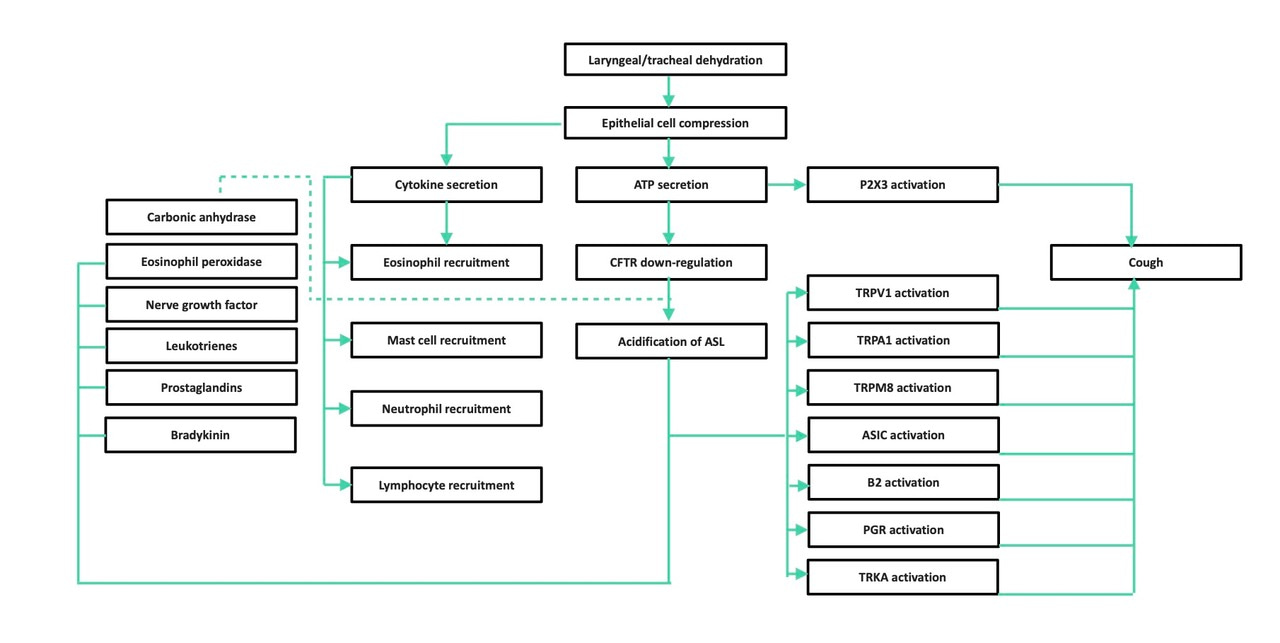
The mucus transpiration inflammatory cascade provokes cough via many pathways.
Cough and bronchospasm are common afflictions of athletes and increase in frequency when athletes exercise in dry air. Thirty percent of hikers who climb Mount Everest have been reported to experience persistent cough, the so-called Khumbu cough.
Mechanical compression of airway epithelial cells has been shown in multiple studies to be implicated in the pathogenesis of asthma and chronic respiratory disease. Compressions of the magnitude delivered by a bronchospasm over a period of a few hours have consistently been shown to promote secretion of inflammatory cytokines and a cascade of inflammatory consequences similar in nature to those shown by the authors of the new report to occur on persistent exposure to dry air.
The report in the current issue of Communications Earth & Environment raises the possibility that the chronic mouth breathing of dry air may play a role in the emergence of chronic airway illnesses such as chronic cough. Chronic cough is a condition first reported in the 1970s. Today, chronic cough is estimated to afflict approximately 10% of the human population. Other mucosa that are chronically exposed to the atmosphere appear also to be at risk, such as ocular mucosa. Dry Eye Disease, also first reported in the 1970s, now afflicts an estimated 11% of the human population.
Hydrating mucosa to avoid the dehydrated state, or rehydrating acutely dehydrated while otherwise healthy mucosa, is a hydration matter with multiple options. Nasal breathing can help avoid airway dehydration. Maintaining indoor air at standard room temperature with relative humidity in the range of 40% to 60%, and avoiding long exposure to very cold and very hot air, are also useful measures to avoid airway dehydration. Approaches to keep airways hydrated independently of breathing condition include the inhalation of hypertonic salt aerosols and the wearing of a face mask.
Rehydration of, and therapeutic relief from, chronically dehydrated airways, as are common to respiratory disease, appears to benefit by inhalation of topically hydrating aerosols, designed to resolve the inflammatory milieu of prolonged airway compression. Such therapeutic aerosols may prove useful future treatments for chronic respiratory diseases.
Our mucosa face increasing risk of inflammation on a dehydrating planet. Without human behavior changes and new hydrating interventions accessible to the entire human population, the burden of respiratory disease is likely to grow. These are not insurmountable challenges. Raising awareness in the medical community along with rapid advance in scientific understanding, can lead to behavioral and therapeutic interventions that help us sustain healthy breathing with climate change.
Follow the Topic
-
Communications Earth & Environment

An open access journal from Nature Portfolio that publishes high-quality research, reviews and commentary in the Earth, environmental and planetary sciences.
Related Collections
With Collections, you can get published faster and increase your visibility.
Holocene hydroclimate
Publishing Model: Hybrid
Deadline: Apr 30, 2026
Archaeology & Environment
Publishing Model: Hybrid
Deadline: Mar 31, 2026

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in