Myocarditis associated with COVID-19 vaccination
Published in Biomedical Research, Pharmacy & Pharmacology, and Immunology
Explore the Research
Myocarditis associated with COVID-19 vaccination - npj Vaccines
npj Vaccines - Myocarditis associated with COVID-19 vaccination
COVID-19 pandemic has challenged and, in some ways, changed many aspects of our society permanently. To promptly and effectively respond to the COVID-19 threat, exceptional efforts had to be put in place, which included the fast development and deployment of COVID-19 vaccines. Different types of COVID-19 vaccines have been authorised in Europe, with the first being the mRNA vaccines. These vaccines have saved millions of lives and have been key in allowing the re-opening of society after a number of lockdowns.
Despite the immense positive impact that the COVID-19 vaccines had in protecting people from severe disease and death, as every vaccine ever produced and authorized for human use, some side effects were identified. Amongst these, the inflammation of the heart muscle and of the lining around the heart, myocarditis and pericarditis, respectively, mostly registered in young males after vaccination with two doses of COVID-19 mRNA vaccines. People affected by myo-pericarditis may experience discomforting events such as chest pain, shortness of breath, and rapid or irregular heart rhythms, which may be due to the reduced heart's ability to pump blood.
Most cases of vaccine associated myocarditis are mild and transient. However, occasionally more severe cases and complications of myocarditis might develop.
Because of the rarity, even the very large clinical trials with thousands of participants are not large enough to detect such rare adverse events; myocarditis and pericarditis could only be detected after the mass vaccination campaigns. Importantly, myocarditis and pericarditis are linked to several viral infections including infection with SARS-CoV-2 and also to other vaccines, like live attenuated virus smallpox vaccines. In particular, myocarditis linked to SARS-COV-2 infection has been recorded much more frequently than after COVID-19 mRNA vaccination. The safety profile of COVID-19 mRNA vaccines remains acceptable and supports a favorable benefit risk balance.
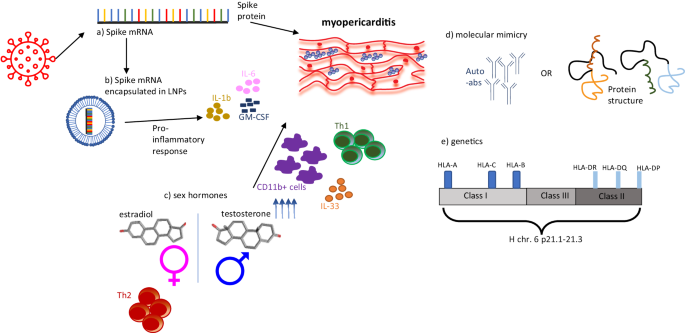
In this article we have concisely reviewed current literature on the epidemiology and possible pathophysiological mechanisms of myo-pericarditis after COVID-19 mRNA vaccination, also schematically summarised in Figure 1. 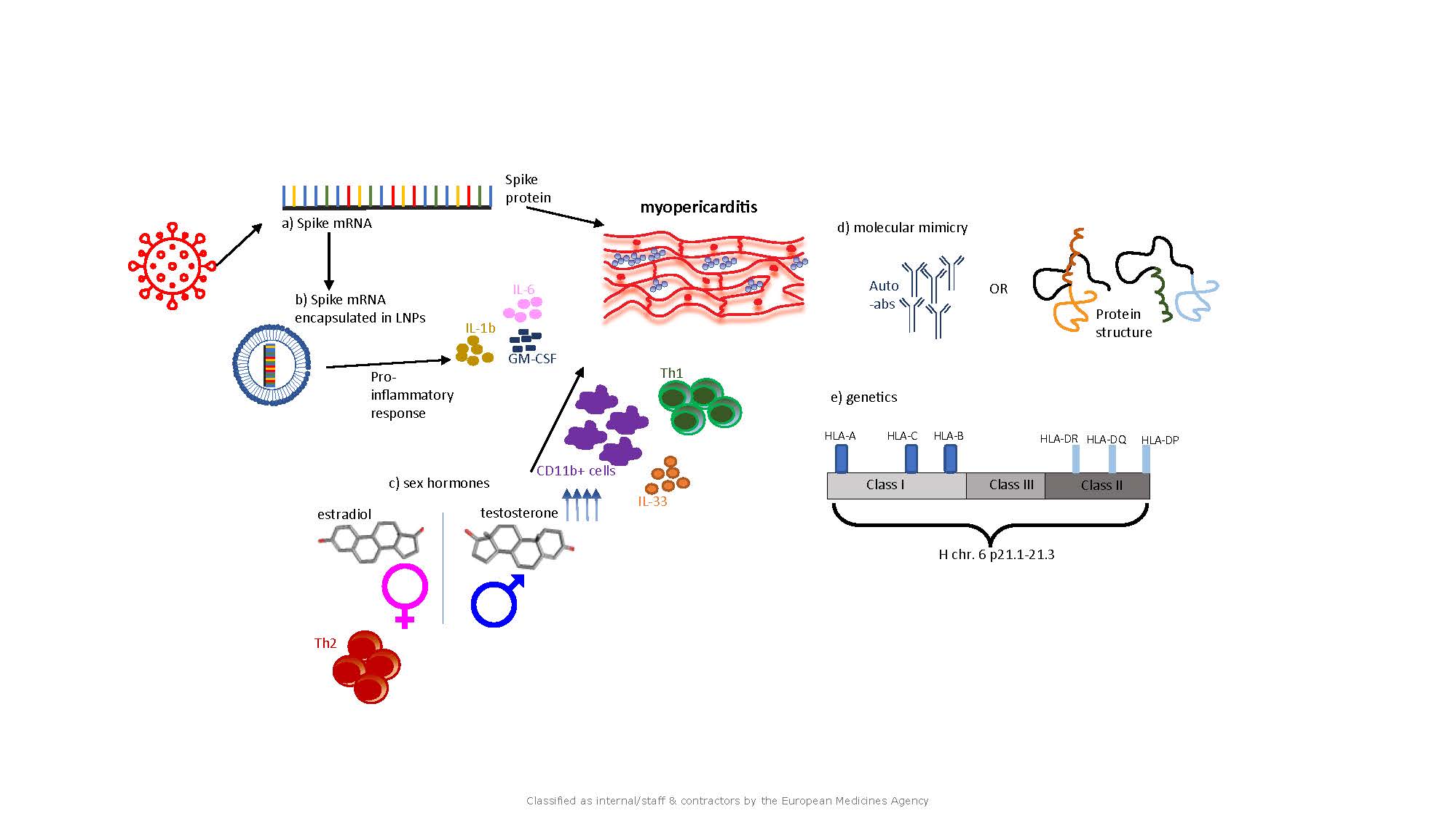
Among the various working hypotheses of vaccine induced myocarditis, the expression of the viral spike protein mediated by the COVID-19 vaccine and recognized by the vaccinees immune system may activate specific immune responses, some of which could contribute to inflammation of the heart. In the mRNA vaccines, the spike encoding mRNA sequence is contained in lipid nanoparticles, which can themselves trigger a proinflammatory response with effect on the heart. Another hypothesis postulates that the intrinsic hormonal differences between men and women are at the basis of the adverse event. Other researchers postulated that myo-pericarditis could be driven by autoimmune responses. Additionally, genetic factors may also contribute to the risk to develop myocarditis upon mRNA vaccination as seen with viral infection associated myocarditis.
In our article, we share an overview of the research activities we think are most important to fill in the current knowledge gaps in the characterization and understanding of this rare disease post vaccination.
As the mRNA platform technology is going to be used not only for vaccine development against infectious diseases but also for application in other medical areas, a better understanding of the disease mechanism leading to these adverse events after COVID-19 vaccination is crucial for the design and use of improved next generation mRNA based vaccines and therapeutics.
More details at: Myocarditis associated with COVID-19 vaccination | npj Vaccines (nature.com)
Follow the Topic
-
npj Vaccines

A multidisciplinary journal that is dedicated to publishing the finest and high-quality research and development on human and veterinary vaccines.
Related Collections
With Collections, you can get published faster and increase your visibility.
Lipid nanoparticle (LNP)-adjuvanted vaccines
Publishing Model: Open Access
Deadline: Feb 19, 2026
Therapeutic HPV vaccines
Publishing Model: Open Access
Deadline: Jun 30, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in