Pre-diagnosis dietary patterns and risk of multiple myeloma in the NIH-AARP diet and health study
Published in Healthcare & Nursing, Cancer, and General & Internal Medicine

Despite patient interest in knowing whether diet is linked to multiple myeloma (MM), there is limited research on dietary patterns and MM risk [1]. Two studies have assessed this risk, albeit with a small number of MM cases. The EPIC-Oxford cohort and Oxford Vegetarian study (65 MM cases) showed that fish eaters, vegetarians and vegans had significantly reduced MM risk compared to meat eaters (RR 0.23, 95% CI, 0.09-0.59) [2]. The Nurses' Health Study and Health Professionals Follow-up Study (478 MM cases) showed a significantly increased MM risk in men with Empirical Dietary Inflammatory Pattern (HR 1.16, 95% CI, 0.96-1.24) [3]. Therefore, we evaluated the association between pre-diagnosis dietary patterns and MM risk in the NIH-AARP Diet and Health Study.
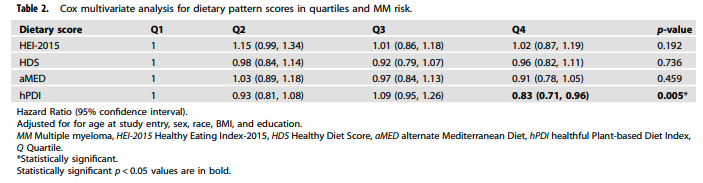
The NIH-AARP Diet and Health study is a prospective cohort of 567,169 persons who completed a food frequency questionnaire in 1995-1996 and were followed until December 2011. Healthy Eating Index-2015 (HEI-2015), Healthy Diet Score (HDS), alternate Mediterranean Diet (aMED) and healthful Plant-based Diet Index (hPDI) scores were calculated using a priori defined methods and grouped into quartiles, with higher scores reflecting healthier eating patterns. Many of these scores have previously been inversely associated with cancer risk and cancer mortality. We prospectively evaluated the association between pre-diagnosis dietary patterns and MM incidence in this cohort. For all dietary variables, we utilized the residual method to adjust for energy intake prior to calculating dietary scores. HR and 95% CI for MM risk in highest versus lowest quartiles of dietary index scores were estimated using multivariate Cox proportional hazards models with person-years as the underlying time metric. The models were adjusted for age at study entry, sex, race, body mass index, and education.
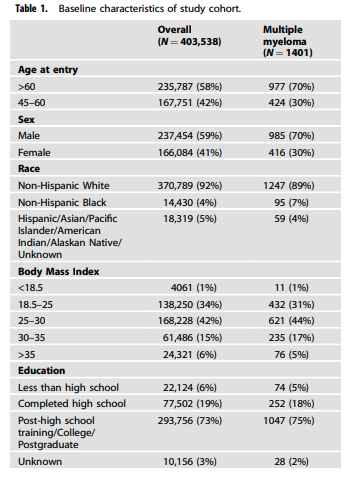
Among 403,583 participants (after exclusions), a total of 1,401 MM cases (58.8% males; 91.8% non-Hispanic whites, 34.3% normal BMI, 5.5% completed less than high school) were identified during the follow-up period (Table 1). Analysis revealed a significant association between hPDI scores and reduced MM risk (highest vs lowest quartile, HR 0.83; 95%CI 0.71-0.96; p=0.005) (Table 2). One of the limitations of a food questionnaire, used in this study and many other dietary studies, is self-reported data. To account for the potential that some respondents’ diets might have changed as a result of preclinical disease or undiagnosed MM at baseline, we conducted sensitivity analyses. In a sensitivity analysis (1331 MM cases), hPDI was similarly associated with a statistically significant reduced MM risk (HR 0.85, 95% CI 0.73–0.99, p = 0.033). HEI-2015, HDS and aMED scores were not associated with MM risk in either analysis.
The hPDI differs from the other dietary scores, in that it is the only fully plant-based score, giving negative points to intake of any animal products. The overall plant-based diet index (PDI) and hPDI were developed by splitting 18 dietary components into three groups: healthful plant foods (vegetables, whole grains, fruits, legumes, nuts, vegetable oils, tea/coffee), unhealthful plant foods (fruit juices, refined grains, potatoes, sugar sweetened beverages, sweets/desserts), and animal foods [4]. We utilized the hPDI, in which the highest score was given to the highest quintile of intake for each healthful food group available, and the lowest score given to the highest quintile of intake for unhealthful plant foods and animal foods available.
A healthful plant-based diet was associated with reduced MM risk in the NIH-AARP cohort. Our findings confirm the observations from the EPIC-Oxford and Oxford-Vegetarian study. These results will help oncologists and patients make informed choices about their diet. To our knowledge, this is the largest epidemiologic study to date assessing pre-diagnosis dietary patterns and MM risk with 1,401 MM cases. Larger randomized clinical trials are needed to better understand this potential association and its underlying mechanisms. Preliminary results of a pilot nutrition-based intervention study (NUTRIVENTION) in individuals with precursor plasma cell disorders and BMI ≥25 (NCT04920084) show that a high-fiber plant-based diet is feasible and leads to improvement in biomarkers associated with progression to MM such as insulin resistance and gut microbiome diversity and composition and reduction in progression trajectory in 2 patients [5]. A larger randomized plant-based dietary study (NUTRIVENTION-3) is currently enrolling (NCT05640843) [6].
References:
- Malik MA, Sweeney NW, Jafri M, Derkach A, Chmielewski C, Adintori PA, et al. Nutrition perceptions, needs and practices among patients with plasma cell disorders. Blood Cancer J. 2022;12:70.
- Key TJ, Appleby PN, Crowe FL, Bradbury KE, Schmidt JA, Travis RC. Cancer in British vegetarians: updated analyses of 4998 incident cancers in a cohort of 32,491 meat eaters, 8612 fish eaters, 18,298 vegetarians, and 2246 vegans. Am J Clin Nutr. 2014;100:378s–85s
- Lee DH, Fung TT, Tabung FK, Colditz GA, Ghobrial IM, Rosner BA, et al. Dietary pattern and risk of multiple myeloma in two large prospective US Cohort Studies. JNCI cancer Spectr. 2019;3:pkz02
- Satija A, Bhupathiraju SN, Rimm EB, Spiegelman D, Chiuve SE, Borgi L, et al. Plantbased dietary patterns and incidence of type 2 diabetes in US men and women: results from three prospective cohort studies. PLoS Med. 2016;13:e1002039.
- Shah UA, Castro F, Derkach A, Fei T, Hosszu KK, McAvoy D, et al. A whole foods plant-based weight loss intervention improves quality of life, metabolic, microbiome and immune profile in MGUS/SMM as well as progression trajectory in a subset - the nutrivention trial. Blood. 2023;142:4771
- Shah UA, Castro F, Anuraj A, Schach E, Derkach A, Joseph NS, et al. A randomized placebo controlled study of a plant-based dietary versus supplement versus placebo intervention in patients with monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM) - the Nutrition Prevention (NUTRIVENTION-3) Study. Blood. 2022;140:5052–5
Follow the Topic
-
Leukemia

This journal publishes high quality, peer reviewed research that covers all aspects of the research and treatment of leukemia and allied diseases. Topics of interest include oncogenes, growth factors, stem cells, leukemia genomics, cell cycle, signal transduction and molecular targets for therapy.





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in