Temporal dynamics in mental health symptoms and loneliness during the COVID-19 pandemic
Published in Healthcare & Nursing
What led to this study
The coronavirus disease 2019 (COVID-19) pandemic and related government-imposed lockdown measures have affected social life and mental health worldwide (1, 2). The existing studies have helped to identify different mental health trajectories and psychological or sociodemographic factors (e.g., being female, young, lonely) related to the deterioration of mental health during the pandemic (e.g., 3). To elucidate the complex and dynamic interactions among symptoms, network analytical approaches have been proposed (4). From the perspective of the network approach to psychopathology (5, 6) co-occurring psychopathological symptoms, referred to as nodes, are connected with each other to a greater or lesser extent (these connections between symptoms are also referred to as edges). Thus, it is assumed that symptoms mutually influence and possibly reinforce each other, with central symptoms characterized by a substantial influence on other symptoms. These symptoms may prove clinically relevant because, in theory, they lead to an activation of the entire network, thus increasing symptom activation (7).
In the context of the COVID-19 research, loneliness has been identified as a central relevant symptom. In addition, worthlessness functioned as bridge symptom in a cross-sectional network, exerting a high influence on the activation of the relationship between of depression and parental stress (8). Loneliness and worthlessness appear to be particularly relevant to be studied in a longitudinal approach, as these cross-sectional studies provide a limited perspective and cannot unravel unfolding dynamic symptom changes, which is particularly relevant for prolonged stressors as pandemics.
What we did
We conducted a secondary data analysis by drawing on data from the Understanding Society UK Household Longitudinal Study, a nationally representative, prospective cohort study in the United Kingdom (UK) with about 40,000 households assessed since 2009 (9, 10). In line with our research questions, we focused on the analysis of the most recent measurement occasion before the onset of the pandemic (2019/2020), the first time-point during the pandemic (April 2020, wave 1, n = 17,761), and the subsequent peaks, i.e., wave 6 (November 2020, n = 12,035) and wave 7 (January 2021, n = 11,968), as defined by COVID-19 incidence and stringency index.
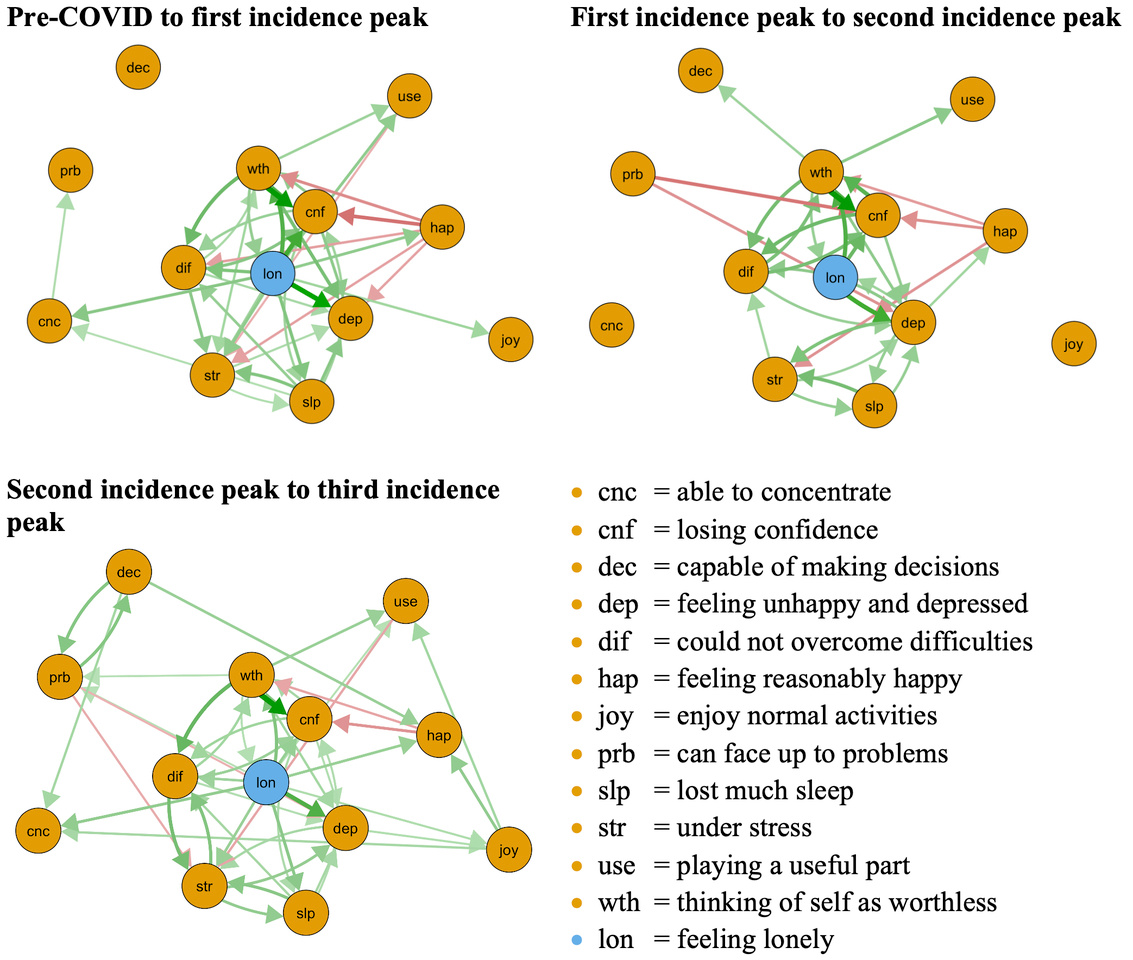
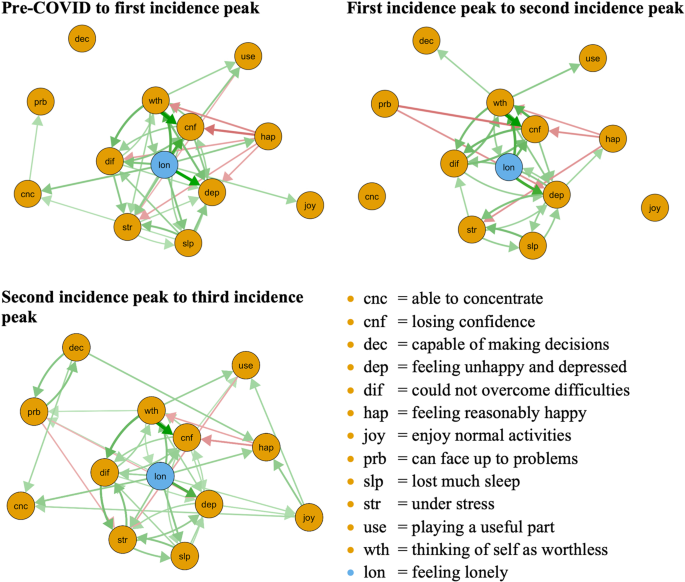
To quantify the centrality of symptoms in our directed CLPNs, we examined two centrality indices: in- and out-expected-influence. These indices are calculated by all outgoing symptom associations one respective item has with all other items in the following wave. This centrality measure is coined out-expected-influence (the degree to which a symptom predicts other symptoms). The other centrality metric is quantified by the ingoing symptom associations one item has with all other items and is labelled in-expected-influence (the degree to which a symptom is predicted by other symptoms).
What we found
We found consistent patterns of symptom associations over time as thinking of self as worthless → losing confidence and loneliness → feeling unhappy and depressed displayed the strongest connections in all networks. Similarly, the standardized centrality parameters indicated that feeling unhappy and depressed and could not overcome difficulties and losing confidence had the strongest in-expected-influence, and loneliness and thinking of self as worthless had the strongest out-expected-influence in all networks.
What it means
The present study provides insights into the dynamics of symptom levels, and sheds light on the activation of symptom cascades that may have been involved in such population level shifts. It appears that the symptom cascades and the findings as a whole have a high relevance in our sample. The present findings suggest that feelings of loneliness and worthlessness increase the risk of mental health deterioration and facilitate later cascades of symptom escalation under chronic stressors such as repeated lockdowns, thus constituting clinically relevant targets for prevention and intervention.
Together with previous findings on loneliness (11-13), our study reemphasizes the importance of loneliness for the escalation of other mental health symptoms, thus constituting a key target for intervention (14). Prevention and intervention programs could be implemented on societal level (e.g., in educational institutions) as regular courses on stress reduction, emotional regulation, empathy, and self-compassion after proving their effectiveness. On an individual level, home visits and daily contact programs were proposed to target loneliness (14). Hence, at any time in the pandemic, especially at the relevant times of onset and incidence peaks, it is advisable and important to address the social connectedness and potential social isolation of individuals and to implement appropriate programs to counteract the impairment of mental health at an early stage. For instance, when implementing contact restrictions, policy makers need to consider how to adequately enable social support groups or small in-person group activities to stop the manifestation of loneliness. For example, single-session growth mindset interventions for adolescent anxiety and depression could be helpful to reduce mental health deterioration (15).
In addition, it is important for prevention and intervention to disentangle how to address the needs for individuals who were already lonely before the pandemic compared to persons who became lonely in light of the restrictions (11). From our findings it can be deduced that loneliness does not have to be addressed only during the pandemic, but already before, so that one is better prepared for such stressors (14). As loneliness was an important variable during all stages of the pandemic, it needs to be investigated whether different groups of individuals felt lonely during the pandemic. Intervention programs that take place online are already available for this purpose (e.g., 19, 20), reducing loneliness and ameliorating feelings of belonging (for an extended review see 21). Single-session interventions are also available, and first studies found evidence of reducing hopelessness and increasing agency, among other outcomes (22). Overall, there are different opportunities to implement appropriate specific interventions to counteract the deterioration of symptom cascades at an early stage. These could be implemented as early interventions or, at the onset of a pandemic, in terms of indicated prevention as a preventive measure for potential at-risk groups.
References
1. Chu IY-H, Alam P, Larson HJ, Lin L. Social consequences of mass quarantine during epidemics: a systematic review with implications for the COVID-19 response. Journal of Travel Medicine. 2020;27(7).
2. Szcześniak D, Gładka A, Misiak B, Cyran A, Rymaszewska J. The SARS-CoV-2 and mental health: From biological mechanisms to social consequences. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2021;104:110046.
3. Pierce M, McManus S, Hope H, Hotopf M, Ford T, Hatch SL, et al. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. The Lancet Psychiatry. 2021;8(7):610-9.
4. Borsboom D, Cramer AOJ. Network Analysis: An Integrative Approach to the Structure of Psychopathology. Annual Review of Clinical Psychology. 2013;9(1):91-121.
5. Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16(1):5-13.
6. McNally RJ. Can network analysis transform psychopathology? Behaviour Research and Therapy. 2016;86:95-104.
7. Borsboom D, Deserno MK, Rhemtulla M, Epskamp S, Fried EI, McNally RJ, et al. Network analysis of multivariate data in psychological science. Nature Reviews Methods Primers. 2021;1(1):58.
8. Skjerdingstad N, Johnson MS, Johnson SU, Hoffart A, Ebrahimi OV. Feelings of worthlessness links depressive symptoms and parental stress: A network analysis during the COVID-19 pandemic. European Psychiatry. 2021;64(1):e50.
9. University of Essex IfSaER. Understanding Society: Waves 1-11, 2009-2020 and Harmonised BHPS: Waves 1-18, 1991-2009. [data collection]. 14th Edition ed: UK Data Service. SN: 6614; 2020.
10. University of Essex IfSaER. Understanding Society: COVID-19 Study, 2020-2021. [data collection]. 11th Edition ed: UK Data Service. SN: 8644; 2021.
11. Bu F, Steptoe A, Fancourt D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health. 2020;186:31-4.
12. Cooper K, Hards E, Moltrecht B, Reynolds S, Shum A, McElroy E, et al. Loneliness, social relationships, and mental health in adolescents during the COVID-19 pandemic. Journal of Affective Disorders. 2021;289:98-104.
13. Groarke JM, Berry E, Graham-Wisener L, McKenna-Plumley PE, McGlinchey E, Armour C. Loneliness in the UK during the COVID-19 pandemic: Cross-sectional results from the COVID-19 Psychological Wellbeing Study. PLOS ONE. 2020;15(9):e0239698.
14. Jeste DV, Lee EE, Cacioppo S. Battling the Modern Behavioral Epidemic of Loneliness: Suggestions for Research and Interventions. JAMA Psychiatry. 2020;77(6):553-4.
15. Schleider J, Weisz J. A single-session growth mindset intervention for adolescent anxiety and depression: 9-month outcomes of a randomized trial. Journal of Child Psychology and Psychiatry. 2018;59(2):160-70.
16. Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychological Medicine. 1997;27(1):191-7.
17. Daly M, Sutin AR, Robinson E. Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study. Psychological Medicine. 2022;52(13):2549-58.
18. Greenberg MT, Abenavoli R. Universal Interventions: Fully Exploring Their Impacts and Potential to Produce Population-Level Impacts. Journal of Research on Educational Effectiveness. 2017;10(1):40-67.
19. Bouwman TE, Aartsen MJ, van Tilburg TG, Stevens NL. Does stimulating various coping strategies alleviate loneliness? Results from an online friendship enrichment program. Journal of Social and Personal Relationships. 2017;34(6):793-811.
20. Walton GM, Cohen GL. A brief social-belonging intervention improves academic and health outcomes of minority students. Science. 2011;331(6023):1447-51.
21. Bessaha ML, Sabbath EL, Morris Z, Malik S, Scheinfeld L, Saragossi J. A Systematic Review of Loneliness Interventions Among Non-elderly Adults. Clinical Social Work Journal. 2020;48(1):110-25.
22. Schleider JL, Mullarkey MC, Fox KR, Dobias ML, Shroff A, Hart EA, et al. A randomized trial of online single-session interventions for adolescent depression during COVID-19. Nature Human Behaviour. 2022;6(2):258-68.
Follow the Topic
-
Translational Psychiatry

This journal focuses on papers that directly study psychiatric disorders and bring new discovery into clinical practice.
Related Collections
With Collections, you can get published faster and increase your visibility.
Moving towards mechanism, causality and novel therapeutic interventions in translational psychiatry: focus on the microbiome-gut-brain axis
Publishing Model: Open Access
Deadline: May 19, 2026
From mechanism to intervention: translational psychiatry of childhood maltreatment
Publishing Model: Open Access
Deadline: Feb 28, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in