The impact of residual disease after surgery on ovarian cancer survival
Published in Biomedical Research and General & Internal Medicine

Background
Most invasive ovarian cancers (including cancers of the ovary, fallopian tube, or primary peritoneal cancer) are treated with surgery. During the surgery, the goal is to remove as much of the tumor as possible so that there is no residual tumor left following the surgery. Depending on the tumor characteristics and spread, this may not be possible, and in those cases the goal has been to remove as much tumor as possible. Our study looked at patients who had surgery for their ovarian cancer and compared patients with no tumor remaining after surgery to those who had at least some tumor remaining; this information was reported by the surgeon. Among the patients with tumor remaining after surgery, we evaluated whether the amount of reported residual tumor was significantly associated with survival. These associations were also evaluated considering the type of ovarian cancer the patient was diagnosed with (“histotype”), and in the context of the chemotherapy that the patient received.
The 2608 patients included in our study were diagnosed with advanced stage (stages III-IV) invasive ovarian cancer and were diagnosed between 2013-2022. These patients were identified using the Cancer Registry of Norway, and detailed data were available from the Norwegian Clinical Registry for Gynecological Cancer. We evaluated whether there was excess mortality comparing those with residual tumor to those with no reported residual tumor. Cancer drug therapy was evaluated in a patients diagnosed from 2019.
What we found
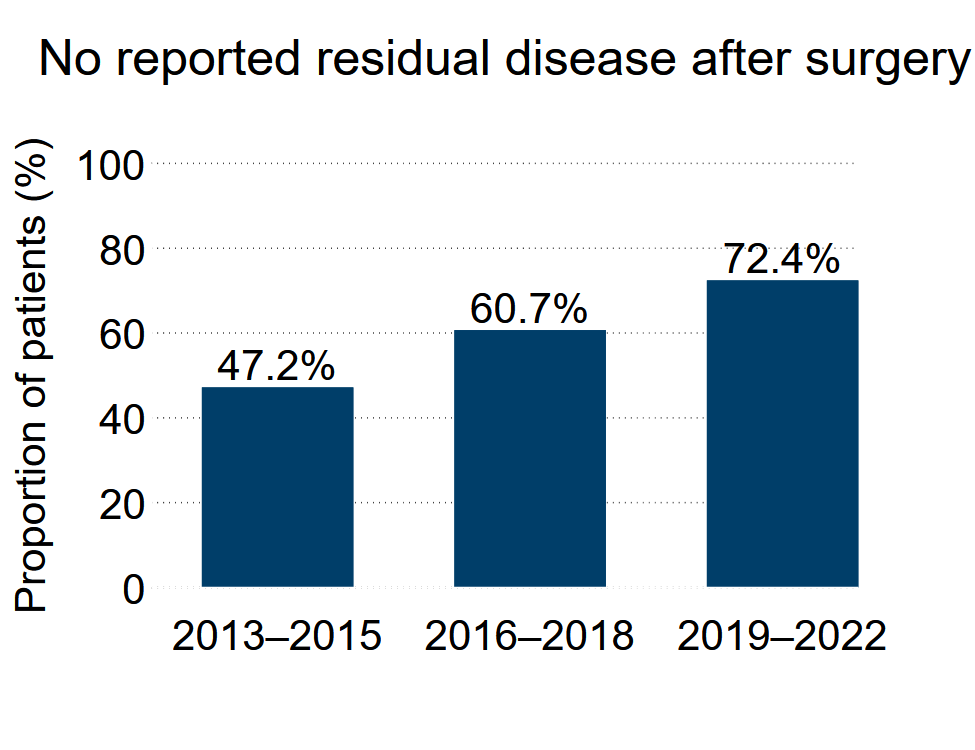
A first observation was that the percentage (and number) of patients with no residual tumor after surgery increased across the years of follow, from 47.2% of patients in the period of 2013-2015 to 72.4% in the most recent period of 2019-2022.
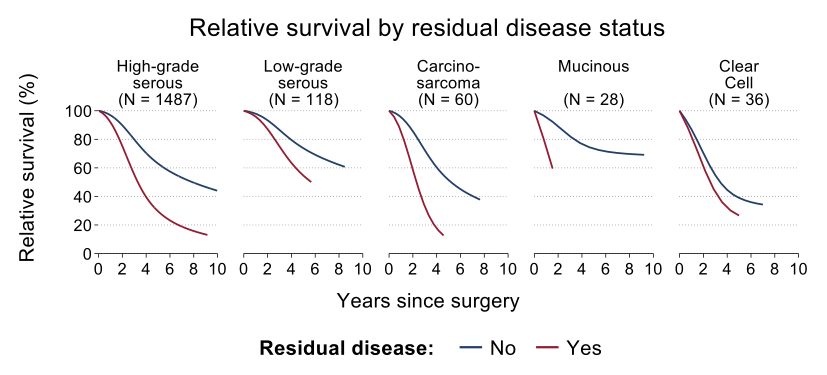
Among the patients who had surgery to remove their tumor, survival was worse for individuals who had residual tumor as compared to no residual tumor following surgery. This finding was consistent regardless of the type of ovarian cancer with which the patient was diagnosed.
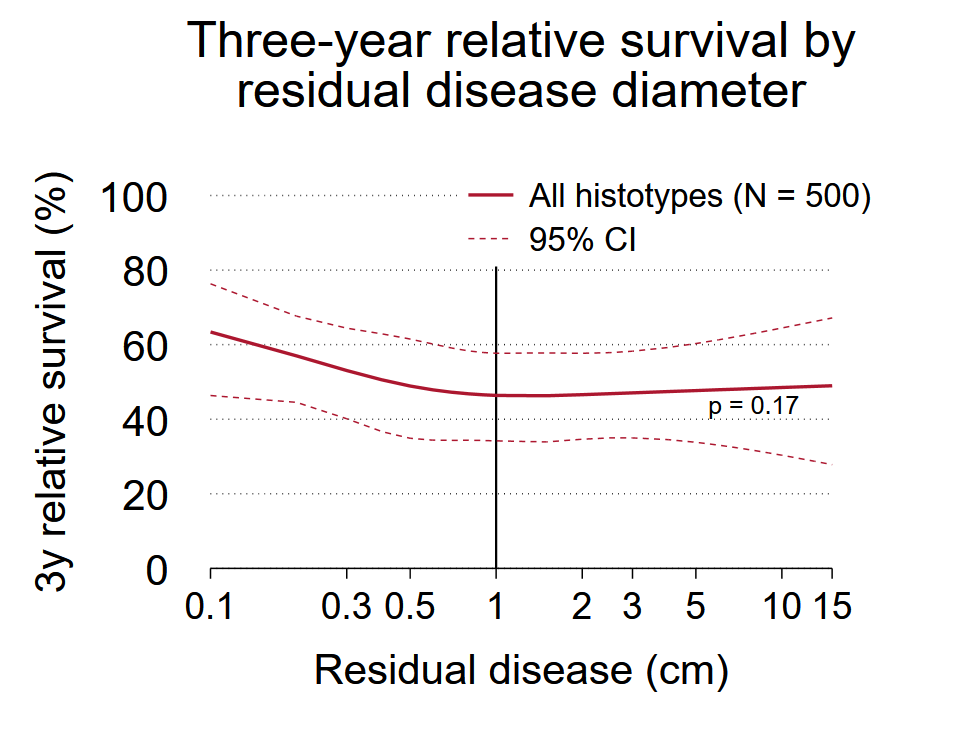
A primary research question was whether the amount of tumor remaining after surgery was associated with survival. Individuals with even very small amounts of reported residual tumor (0.1–0.4 cm in diameter) had approximately 2-fold higher risk of death as compared to women with no evidence of residual tumor. Approximately 3-fold higher risk was observed for all other comparison groups (e.g., 0.5–0.9 cm, exactly 1.0 cm, 1.1–2.9 cm 3.0–20 cm). When evaluating residual tumors across the continuum of reported diameters, no significant association between tumor size and residual disease was observed.
|
Table. Excess hazard ratios (EHR) with 95% confidence intervals (CI) for death due to stage III/IV epithelial ovarian cancer according to amount of residual disease, 2013–2022 (N=1797). |
||
|
Amount of Residual disease |
Patients/ deaths |
EHR (95% CI) |
|
No residual disease |
1154 / 470 |
1 (reference) |
|
0.1–0.4 cm |
138 / 86 |
2.09 (1.63–2.68) |
|
0.5–0.9 cm |
89 / 69 |
2.97 (2.26–3.89) |
|
1.0 cm |
102 / 83 |
2.74 (2.13–3.53) |
|
1.1–2.9 cm |
94 / 61 |
3.10 (2.32–4.13) |
|
3.0–20 cm |
78 / 59 |
2.75 (2.05–3.70) |
|
All estimates were adjusted for age, stage, and Eastern Cooperative Oncology Group (ECOG) performance status. |
||
Why it matters
In current practice “optimal” cytoreduction (tumor removal) is commonly defined as <1 cm residual tumor after surgery. In this study, which evaluated remaining tumor in the context of current chemotherapy treatments, the cut-point of 1 cm did not appear to be a meaningful cut-point for the survival. Achieving no evidence of residual tumor resulted in the best survival outcomes across all evaluated subgroups, as did surgeries resulting in very small amounts of residual tumor (<0.5 cm). This study suggests that the current definition of “optimal” cytoreduction may need to be reconsidered in the context of modern treatment.
What comes next
Further population-based data are needed to confirm these findings, and to further explore the associations when considering specific chemotherapy and targeted therapy treatments.
Follow the Topic
-
British Journal of Cancer

This journal is devoted to publishing cutting edge discovery, translational and clinical cancer research across the broad spectrum of oncology.





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in