The Role of Smartwatch Data in Monitoring Non-Motor Symptoms of Parkinson’s Disease
Published in Healthcare & Nursing, Bioengineering & Biotechnology, and General & Internal Medicine
Parkinson's disease (PD) is widely recognized as a motor disorder, but it encompasses a variety of non-motor symptoms that significantly impact patients' quality of life. These non-motor symptoms, including cognitive impairment, autonomic dysfunction like sleep disturbances and digestive issues, and psychiatric issues, often precede the motor symptoms and continue to affect patients throughout the disease course. Accurate and continuous monitoring of these is needed to improve our understanding of the disease course and ultimately facilitate better care.
The potential of smartwatches
Following a diagnosis of Parkinson's disease, routine care involves a visit to the clinic every 6 months where the main symptoms and their impact on daily life will be assessed via questionnaires and clinical tests. Those visits only provide limited information on the actual status of the patient in real-life and disregard day-to-day variability. Wearables like smartwatches can address these limitations by passively collecting data in real-world settings and have shown promising capabilities in measuring the motor aspects of the disease. The non-motor symptoms remain understudied.
Comparing digital measures to clinical assessments
The study analyzed data from 149 participants from the Parkinson's Progression Markers Initiative (PPMI) diagnosed with Parkinson’s disease, using the Verily Study Watch to collect digital outcome measures such as physical activity, sleep metrics, and vital signs. Weekly averages of the digital outcome measures around the clinic visit (Figure 1) were compared with clinical assessments of non-motor symptoms to evaluate their correlation and potential utility of smartwatch data in clinical settings.
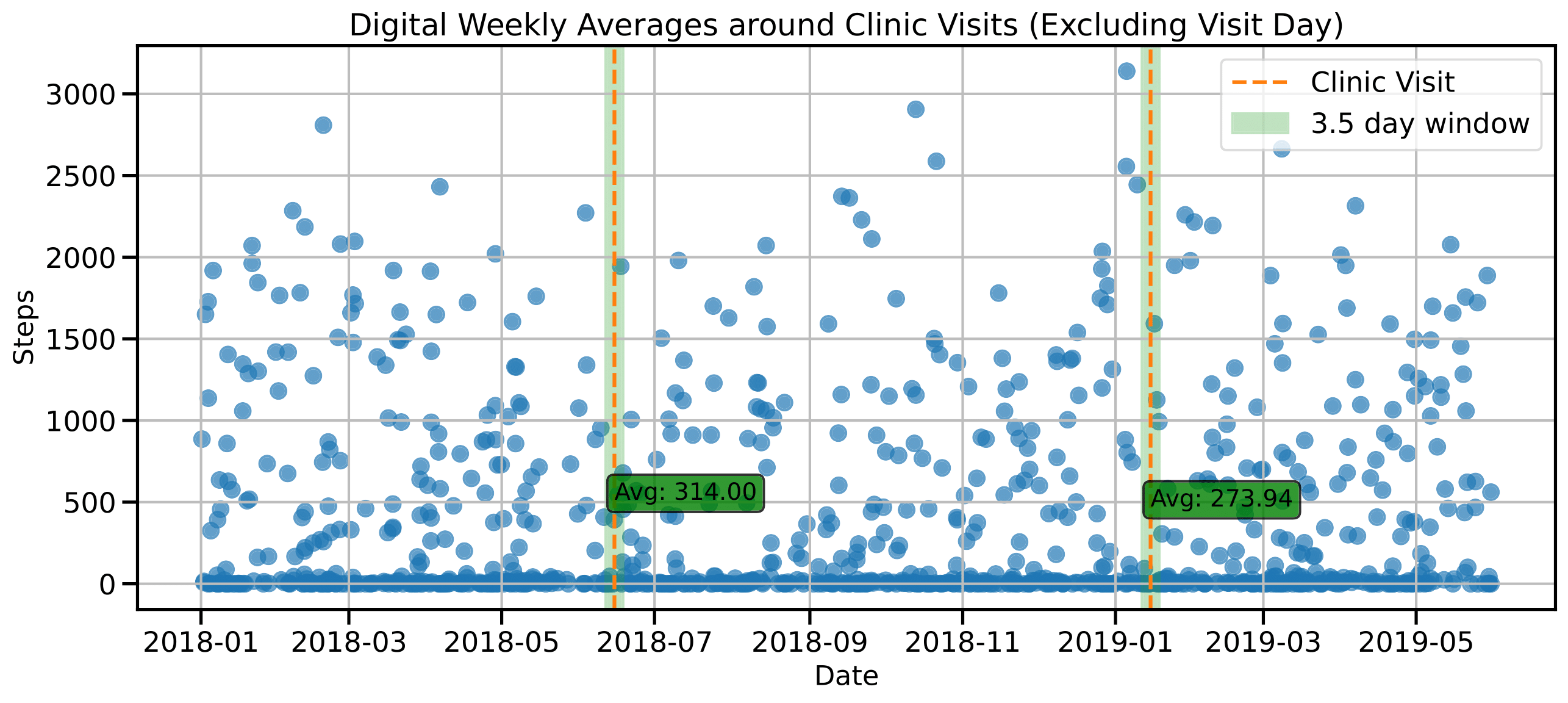
Using the continuously collected digital sensor data, digital weekly averages spanning 3.5 days around the clinic visit were computed excluding the visit day itself.
Key Findings
-
Digitally Measured Physical Activity and Sleep are Associated with Non-Motor Symptoms: Associations were found for clinical assessments of cognition, autonomic functioning, and impairment in daily life. No association were identified for psychiatric symptoms.
- Digital Timeseries Capture Clinical Progression: Long-term digital timeseries data reflects progression of medication, motor symptoms, autonomic functioning, and impairment in daily living.
-
Limited Predictive Performance: Despite found associations, predicting clinical scores based on digital weekly averages on an individual level did not outperform baseline models for most. More tailored sensors and digital measures are required to capture the nuanced aspects of non-motor symptoms more effectively.
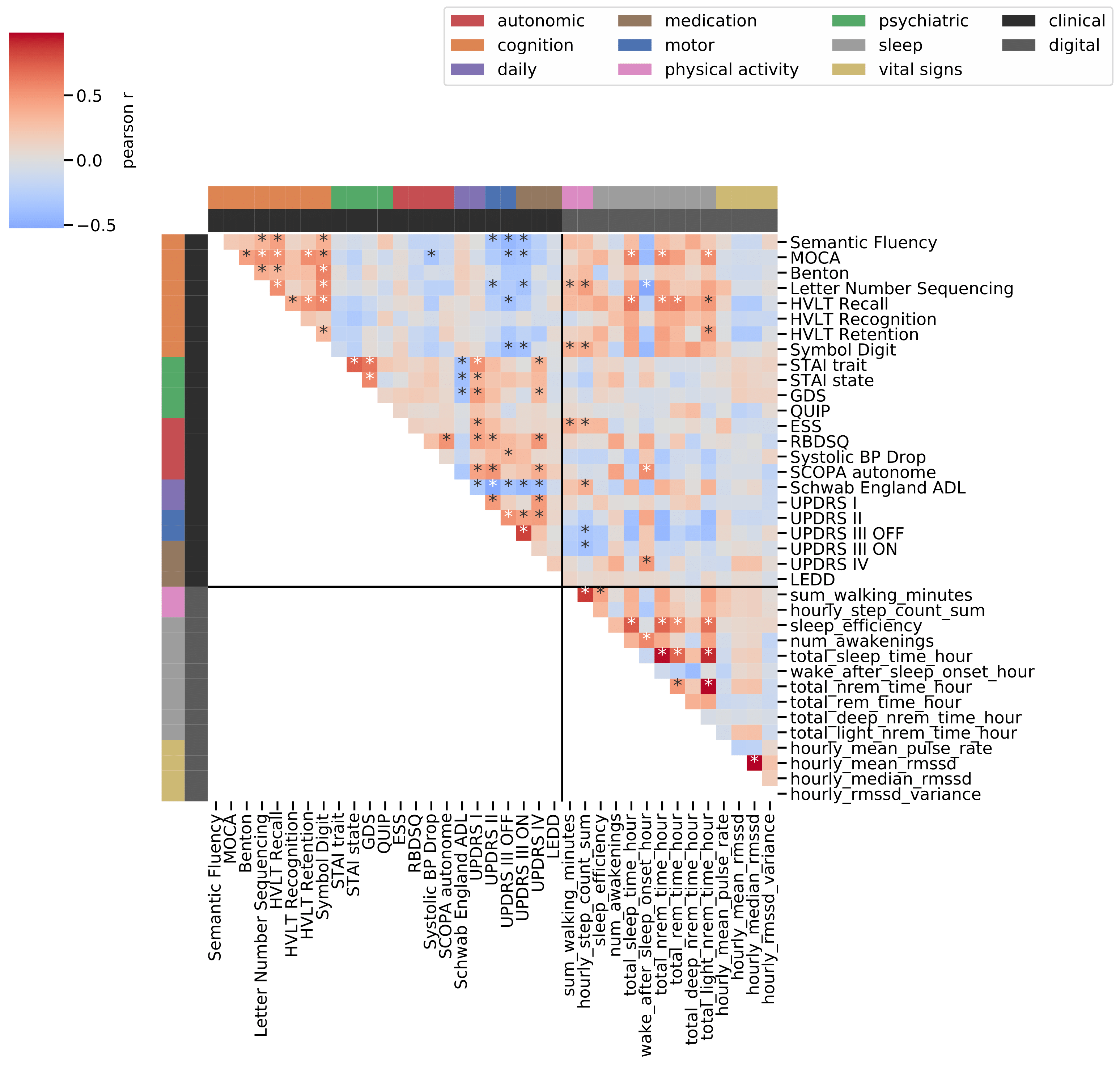
Figure 2: Correlation of digital weekly averages and clinical scores
For each pair of clinical score and digital weekly average, the correlation coefficient is displayed on a divergent color map (red: positive relation, blue: negative relation) with asterisks indicating statistically significant findings.
Challenges and Future Directions
The study highlighted several challenges and areas for improvement in using smartwatch data for monitoring Parkinson's disease:
- Sensor Limitations: The sensors used in the study primarily captured movement-based data, which is limited in assessing non-motor symptoms. Future research should explore the use of more specific sensors, such as those tracking bathroom usage for urinary symptoms or phone usage patterns for depressive symptoms.
- Individual Variability: Non-motor symptoms vary widely among PD patients, necessitating personalized approaches to digital monitoring. Developing algorithms that can adapt to individual patient profiles and provide personalized insights could improve the predictive power of smartwatch data.
Conclusion
Smartwatch data holds significant potential for enhancing the monitoring of non-motor symptoms in Parkinson’s disease. The ability to collect continuous, real-life data offers a valuable complement to traditional clinical assessments, helping to capture the full spectrum of a patient’s condition. Digital health technologies can play a crucial role in improving the management and quality of life for individuals with Parkinson's disease.
Follow the Topic
-
npj Parkinson's Disease

This journal publishes original basic science, translational and clinical research related to Parkinson's disease, including anatomy, etiology, genetics, cellular and molecular physiology, neurophysiology, epidemiology and therapeutic development and treatments.
Related Collections
With Collections, you can get published faster and increase your visibility.
Cognition - preclinical models, and preclinical unmet need
Publishing Model: Open Access
Deadline: Jul 27, 2026
Environmental risk factors for Parkinson’s disease
Publishing Model: Open Access
Deadline: May 13, 2026





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in