Unraveling the Genetic Mysteries of Psychiatric Disorders
Published in Protocols & Methods, Cell & Molecular Biology, and Biomedical Research
Why Do These Disorders Keep Blurring Together?
Psychiatric disorders such as schizophrenia, bipolar disorder and major depressive disorder are known to be complex. While they share overlapping symptoms such as cognitive impairment or mood dysregulation, their underlying biological mechanisms remain unclear. Traditional diagnostic approaches often focus on symptoms, but do not always map clearly onto biology. Therefore, we aimed to delve deeper into the molecular underpinnings of these conditions.
To explore this, we focused on the dorsolateral prefrontal cortex (DLPFC), a brain region critical for decision-making and emotional regulation. This area is often implicated in psychiatric disorders, making it an ideal region to investigate how genetic changes might contribute to disease. But instead of focusing on genes, we took a closer look at exons – the protein-coding parts of genes – because many significant changes are hidden there.
Getting Into the Genetic ‘Weeds’
Genes are often called the "blueprints" of life, but that analogy barely scratches the surface. In reality, each gene can give rise to multiple different transcripts through a process called alternative splicing - where the same gene is chopped up and stitched back together in various ways to create different versions of a protein. These transcripts are essentially alternate instruction manuals, built by including or skipping different segments called exons.
This matters because the exon level is where much of the biological nuance lives. More than 95% of human genes undergo alternative splicing, meaning that focusing only on the overall gene or even transcript level can miss important changes. In our study, this was strikingly clear: While diagnosis had almost no detectable effect on gene-level expression, we found over 2,200 significant hits at the exon level - a difference that would have gone unnoticed in less detailed analyses. To visualize this, take a look at Figure 1, which shows how splicing at the exon level gives us a much sharper resolution of genetic activity.
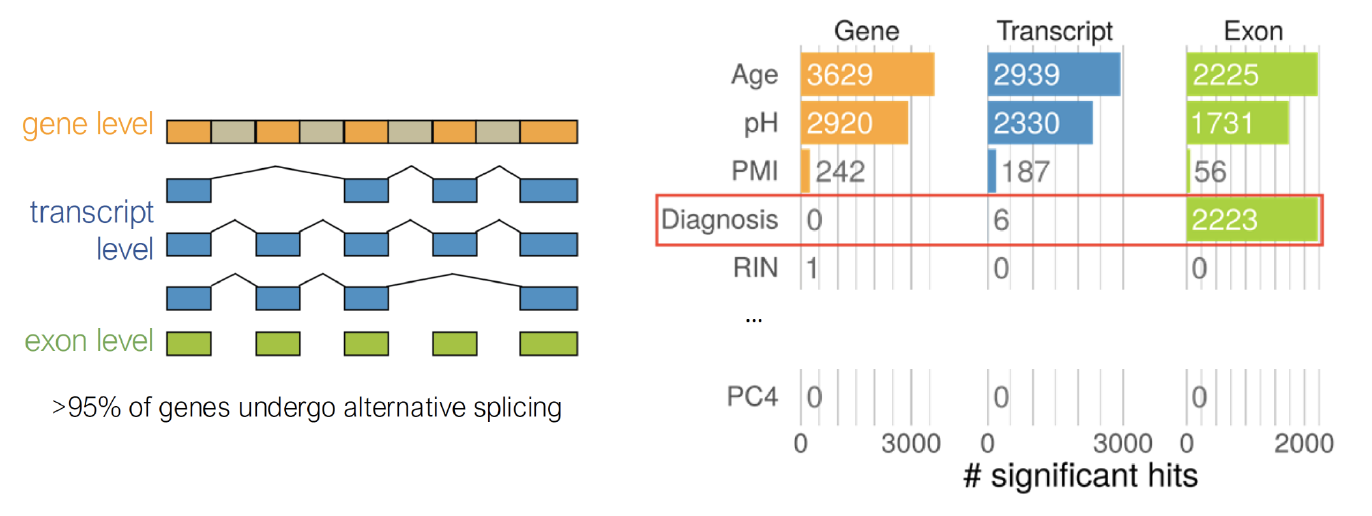
Figure 1: Gene, transcript and exon level explanation.
In other words, it’s not just what gene you have, but how that gene is being spliced and expressed in different brain cells. And when it comes to understanding complex psychiatric disorders, those subtle exon-level shifts can make all the difference.
We used an approach that integrates two types of genetic data:
- Common Variants: These are small genetic differences shared by many people. While each variant has a subtle effect, their combined influence can increase disease risk.
- Rare Variants: These are less common but often have a stronger impact on gene function.
By analyzing how these variants affect exon expression in postmortem brain tissue from individuals with bipolar disorder, major depressive disorder, schizophrenia, and healthy controls, we identified key genes and pathways disrupted across these psychiatric disorders.
The 110 Most Common Suspects and Where They Lead
Our analysis revealed 110 core genes enriched in pathways that link psychiatric disorders to specific biological processes. Among the most significant findings were:
- Circadian Entrainment: Disruptions in the body's internal clock may contribute to mood instability.
- Cortisol Synthesis and Secretion: Cortisol is a key stress hormone, and its dysregulation may contribute to mood instability.
- Dopaminergic Synapses: This pathway is crucial for reward processing and motivation, often impaired in mental health disorders.
These pathways highlight shared molecular mechanisms underlying bipolar disorder, major depressive disorder, and schizophrenia. Interestingly, we found that these core genes were predominantly expressed in excitatory neurons within layers 2–6 of the dorsolateral prefrontal cortex. Excitatory neurons pass signals on to the next neuron.This connection between molecular changes and specific cell types provides new insights into how these disorders affect cognition.
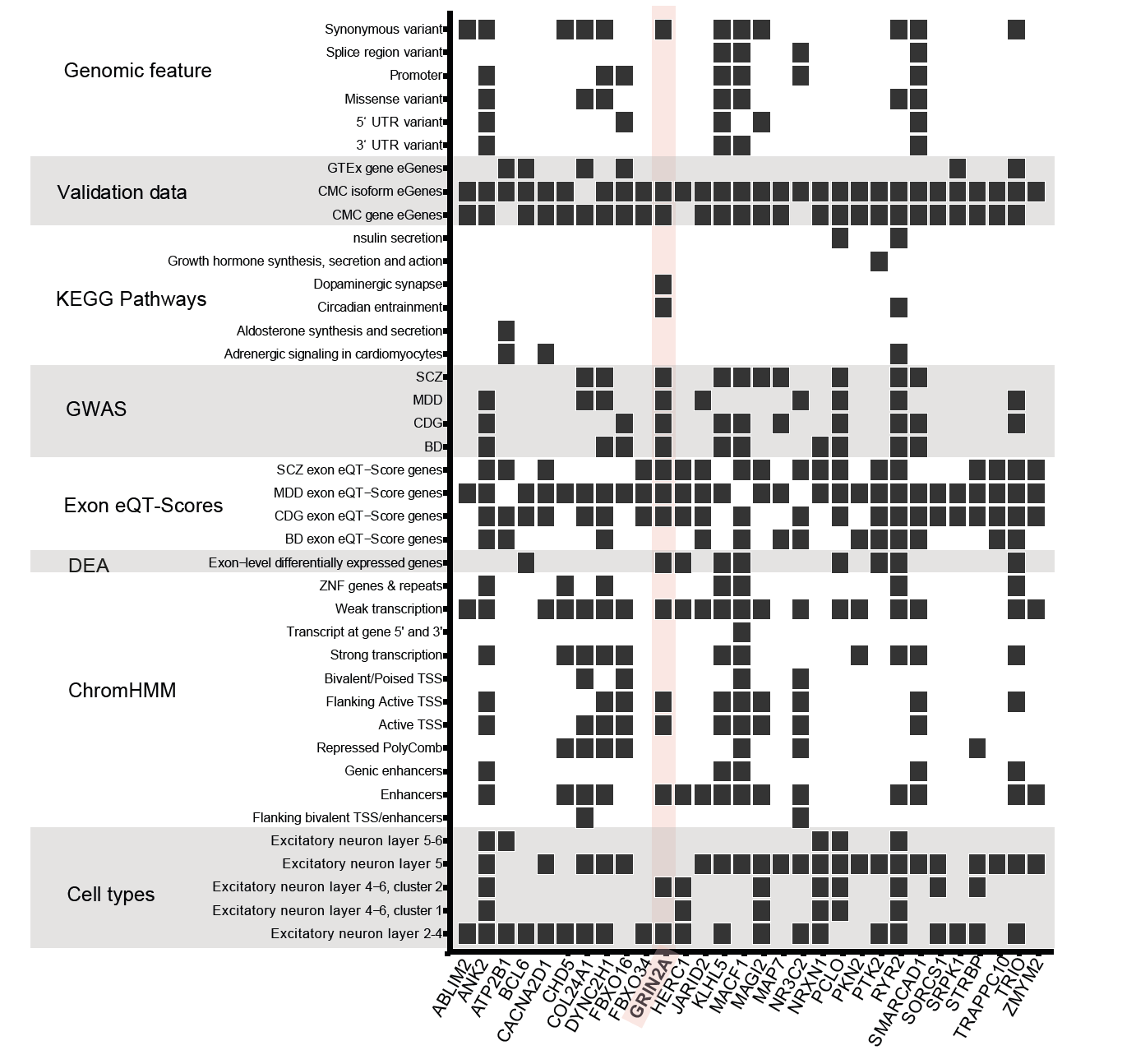
Figure 2 takes it a step further, showing how 30 of our core genes are not only enriched in specific cell types of the dorsolateral prefrontal cortex, but also consistently show up across independent datasets – adding confidence that these signals aren’t just noise, but part of a real, shared molecular signature.
Why It Matters
By identifying shared pathways across psychiatric disorders, our study moves beyond traditional diagnostic categories toward a biology-based framework for understanding mental health. This shift has profound implications for treatment development, for example:
- Drugs targeting disrupted hormone signalling could help stabilise mood and reduce stress-related symptoms.
- Therapies aimed at restoring circadian rhythms might improve sleep and energy levels.
- Interventions targeting dopaminergic synapses could enhance motivation and reward processing.
Mixing It All Together: the Data Cocktail
One of the unique aspects of our study was its use of multimodal data integration.
We combined:
- Exon-level gene expression data from postmortem human brain tissue.
- Single-cell RNA sequencing to pinpoint affected cell types.
- Genetic risk scores to quantify disease susceptibility.
- Rare genetic variants, which often have stronger impacts on protein function.
This comprehensive approach allowed us to identify robust targets for future research and potential therapies interventions.
What’s Next?
This study took us through more revisions, reviewer comments, and rejections than we care to count. But it also brought us across continents, across data types, and – finally – across the finish line.
While our findings represent a significant step forward, they are just one piece of a much larger puzzle. Psychiatric disorders result from a complex interplay of genetic, environmental, and lifestyle factors. Future studies will need to integrate additional data types – such as epigenetic modifications or neuroimaging – to fully understand these conditions.
Nonetheless, our research underscores the importance of moving beyond symptom-based diagnoses toward molecular classifications. By doing so, we can develop more precise treatments that address the root causes of mental health disorders rather than just managing their symptoms.
In the long run, our hope is that insights like these can help shift the field toward more targeted, personalized treatments – offering better outcomes for the many people still waiting for therapies that actually work for them.
Acknowledgments
This work would not have been possible without the collaboration of researchers across multiple institutions and disciplines. We also extend our gratitude to the families who donated postmortem brain tissue for scientific research – your contributions are invaluable.
Follow the Topic
-
Translational Psychiatry

This journal focuses on papers that directly study psychiatric disorders and bring new discovery into clinical practice.
Related Collections
With Collections, you can get published faster and increase your visibility.
Moving towards mechanism, causality and novel therapeutic interventions in translational psychiatry: focus on the microbiome-gut-brain axis
Publishing Model: Open Access
Deadline: May 19, 2026
From mechanism to intervention: translational psychiatry of childhood maltreatment
Publishing Model: Open Access
Deadline: Feb 28, 2026




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in