Valuing Lived Experience: Building the Evidence for Better Care in Pernicious Anaemia
Published in Healthcare & Nursing, Social Sciences, and General & Internal Medicine
The story behind the research
Pernicious anaemia (PA) is a lifelong autoimmune disease leading to severe B12 deficiency. Despite being manageable with regular treatment, it often remains under-recognised and inconsistently managed in clinical practice. This led to the James Lind Alliance Priority Setting Partnership uniting patients, carers, and clinicians to identify the most urgent unanswered questions. At the top of the list were how to improve diagnosis, to understand why symptoms often persist despite treatment, and to explore individual treatment needs.
Working in partnership with the Pernicious Anaemia Society (PAS) and the University of Surrey, and in collaboration with national and international experts, we aimed to turn lived experience into research. Using insights shared by people with PA through PAS, we co-designed a large-scale survey to capture real-world patterns in diagnosis, testing, treatment, and co-existing conditions.
Through PAS, hundreds of people had already described years of unexplained symptoms, repeated misdiagnoses, and ongoing struggles even after diagnosis, as symptoms returned between injections and treatment differed from one practice to the next.
Key findings
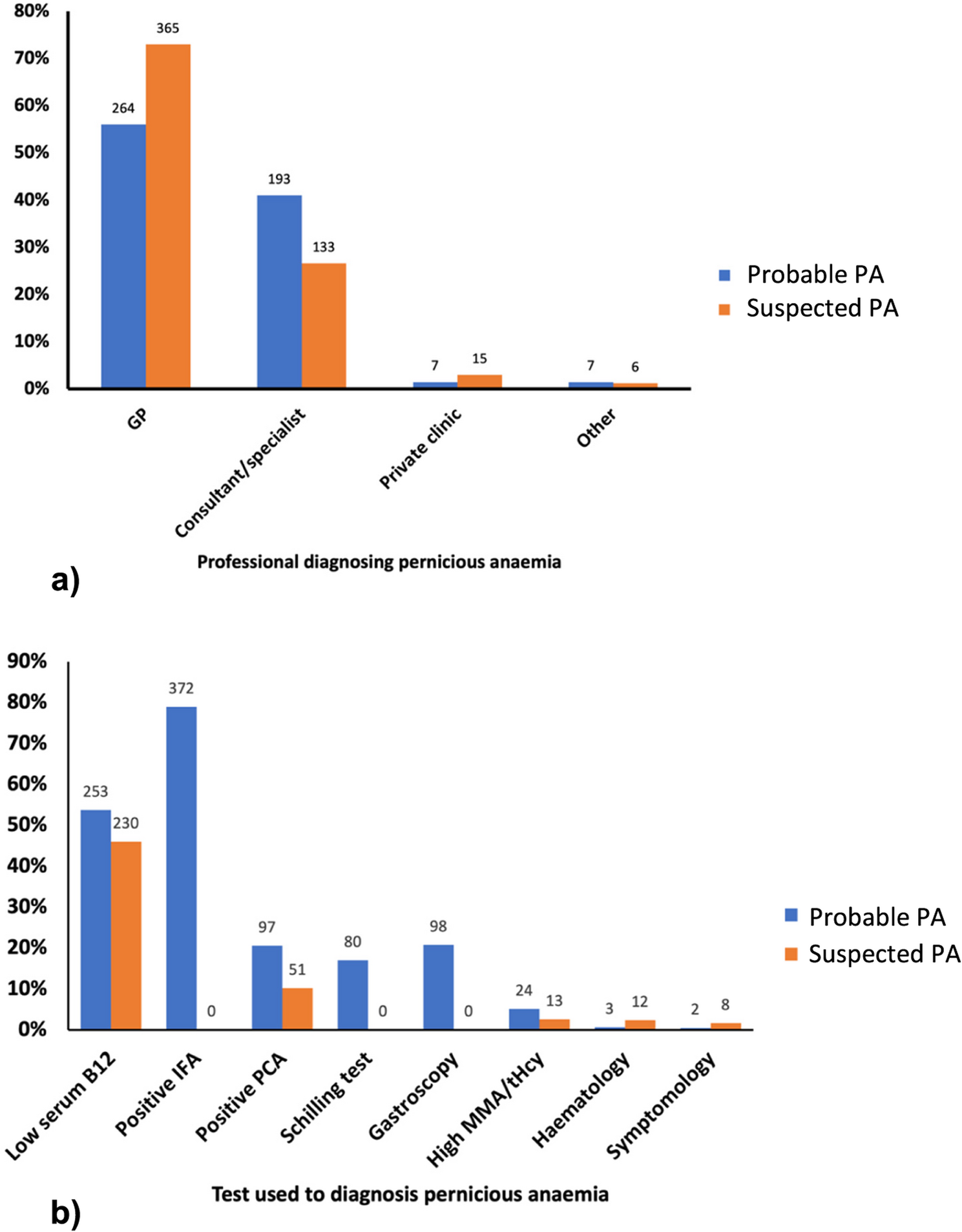
- Diagnosis is delayed. More than one in three people waited at least three years to receive a diagnosis, and one in four waited five years or longer.
- Testing was inconsistent. Only 38% had ever been tested for the key biomarker intrinsic factor antibodies.
- Treatment is variable. Just over half reported a need for more frequent injections than the recommended injections 2-3 monthly schedule (as stated in the British National Formulary), supporting that the “one-size-fits-all” is not appropriate
- Comorbidities were common. About one-third had another autoimmune disease, such as autoimmune thyroid disease or vitiligo. Around 40% also reported iron deficiency.
- Family patterns emerged. Nearly one-third had at least one other family member with PA, and nearly 50% had family members with another autoimmune condition.
These findings highlight that PA presents in diverse ways and cannot be managed through a single diagnostic or treatment pathways.
Why does it matter?
For clinicians, our findings highlight the need to revisit how PA is diagnosed and managed. Early recognition, appropriate testing, and flexible treatment intervals could make a real difference to patient wellbeing.
For people living with PA, the study validates lived experience. It confirms that delayed diagnosis and fluctuating symptoms are not isolated cases, but rather systemic challenges. It also highlights the need for improved life-long therapy and management protocols.
For researchers, the dataset provides a foundation for future research, supporting studies on genetics, multi-morbidity, and studies on symptom trajectories that can help move towards more precision medicine-based care.
This study also shows the power of partnership between researchers and people with lived experience, whose insights shaped every stage of the project, from survey design to interpretation of the results.
What comes next...
This study represents the first step in a wider research programme shaped by the James Lind Alliance priorities. Ongoing projects are now exploring better ways to monitor symptoms using smart-watch technology and developing more precise, holistic and diverse treatment, management and follow-up approaches for people with pernicious anaemia.
Follow the Topic
-
BMC Primary Care

Previously known as BMC Family Practice, this is an open access, peer-reviewed journal that considers articles on all aspects of primary health care research.
Your space to connect: The Primary immunodeficiency disorders Hub
A new Communities’ space to connect, collaborate, and explore research on Clinical Medicine, Immunology, and Diseases!
Continue reading announcementRelated Collections
With Collections, you can get published faster and increase your visibility.
Bridging primary and palliative care
BMC Primary Care is calling for submissions to our Collection, Bridging primary and palliative care. The integration of primary and palliative care is increasingly recognized as essential for improving the quality of life for patients with serious illnesses. This Collection invites research that examines innovative models of care that bridge these two critical domains. The interplay between primary care and palliative care can enhance the patient experience by addressing not only medical needs but also psychosocial and spiritual aspects of care. As healthcare systems evolve, understanding how these two areas can collaborate effectively is crucial for optimizing patient-centered approaches and ensuring comprehensive support for individuals and families.
Advancements in this field highlight the importance of shared decision-making and advanced care planning as mechanisms to enhance communication between healthcare providers and patients. By fostering a collaborative environment, we can empower patients to express their preferences and values concerning their care journey, particularly in the context of end-of-life decisions. Research has shown that integrated approaches lead to better symptom management, reduced hospitalizations, and increased patient and family satisfaction. Ongoing research could transform how we think about and deliver care for patients with serious illnesses.
In this Collection, we welcome submissions that span a wide array of topics, including but not limited to:
- Integrating advanced care planning in primary care
- Shared decision-making in end-of-life care
- Models of palliative care in primary care settings
- Enhancing communication between care teams
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer-review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Jun 08, 2026
Indigenous health and well-being
BMC Primary Care is calling for submissions to our Collection, Indigenous health and well-being. Historically, Indigenous communities have faced significant health disparities driven by systemic inequalities, cultural disconnection, and barriers to accessing healthcare. This Collection seeks to address these issues by gathering research that highlights the unique health challenges faced by Indigenous peoples, including chronic diseases, mental health issues, and the impact of social determinants on health outcomes. By amplifying Indigenous voices and perspectives, we aim to foster a deeper understanding of their health needs and aspirations.
The significance of researching Indigenous health lies in its potential to inform and transform healthcare practices, policies, and systems to achieve health equity. As research grows, we anticipate developments in the field of Indigenous health that may lead to the co-creation of innovative healthcare models. By fostering collaborations between Indigenous communities and healthcare providers, there is potential for enhanced accessibility, culturally appropriate care, and the development of policies that prioritize Indigenous health and well-being. Future studies may also uncover new insights into the role of traditional practices in modern healthcare systems, ultimately bridging the gap between Western medicine and Indigenous healing practices.
In this Collection, we welcome submissions that span a wide array of topics, including but not limited to:
- Barriers to healthcare access for Indigenous populations
- Community health initiatives in Indigenous communities
- Health equity strategies for Indigenous well-being
- Cultural competency in Indigenous healthcare
This Collection supports and amplifies research related to SDG 3: Good Health and Well-being and SDG 10: Reduced Inequalities.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Aug 05, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in