Why obese people are more susceptible to viral infections
Published in General & Internal Medicine, Immunology, and Anatomy & Physiology

The study in brief
The purpose of our study was to investigate and understand why obese people are more likely to be hospitalised and die from viral respiratory infections such as influenza, while non-obese people typically recover after a few days of mild illness.
The immune system’s response to influenza is mainly mediated via the production of specialised chemicals called type I and III interferons (IFN), which leads to activation of interferon-stimulated genes (ISGs). This orchestrates several defence mechanisms that confer protection from a range of viruses1. Although previous research has shown that the type I IFN response is attenuated in obese mice infected with influenza, it remains unclear whether a similar phenomenon occurs in obese humans and whether it might account for the increase in adverse clinical outcomes observed in such individuals2.
To investigate this, we obtained lower airway samples from obese and non-obese people and cultured them in the lab. We examined whether there were any differences in the way cells from non-obese individuals reacted to influenza virus compared to cells from obese individuals, specifically measuring the production of type I and III IFNs.
The findings in a few words
We found that macrophages from the lower airways of obese individuals had a diminished ability to produce interferons. We suspected that this may be due to elevated levels of an obesity-related hormone called leptin within the airways.
To confirm if leptin had a detrimental role on antiviral immunity, we administered leptin directly into the airways of mice before infecting them with influenza. Leptin-treated mice had reduced production of type I IFN in response to influenza infection. We found evidence that this may be due to the ability of leptin to increase expression of a negative regulator of type I IFN, called the suppressor of cytokine signalling (SOCS)-3 (Figure).
Why is this research important?
The incidence of obesity has increased dramatically in recent decades, with global estimates reaching over 650 million people3. At the same time, the 2009 influenza pandemic and the more recent COVID-19 pandemic have highlighted the increased susceptibility of obese patients to viral respiratory infections, as well as the heightened likelihood of hospitalisation and death4,5.
Our research uncovers a previously unrecognised mechanistic role of the obesity-related hormone leptin in mediating the susceptibility of obese individuals to severe influenza infection and suggests that these pathways could be targeted to protect these individuals from severe infections.
What challenges did we face?
Obtaining deep lower airway samples from obese individuals can be especially challenging, as putting them under sedation to perform bronchoscopy carries certain risks. To circumvent this issue we took an opportunistic approach, and obtained samples from obese patients immediately before they underwent bariatric surgery. This allowed us to perform the bronchoscopy while the patients were under general anaesthesia, which was being administered for their surgery.
What are the next steps?
An interesting follow-up question arising from this study would be whether obese patients that undergo gastrectomy or lose weight via other methods, benefit from an improvement in their antiviral immune response.
Furthermore, investigating the therapeutic potential of manipulating leptin hormone levels in obese people as a method of boosting protection against viral infections could be an important future avenue to pursue.
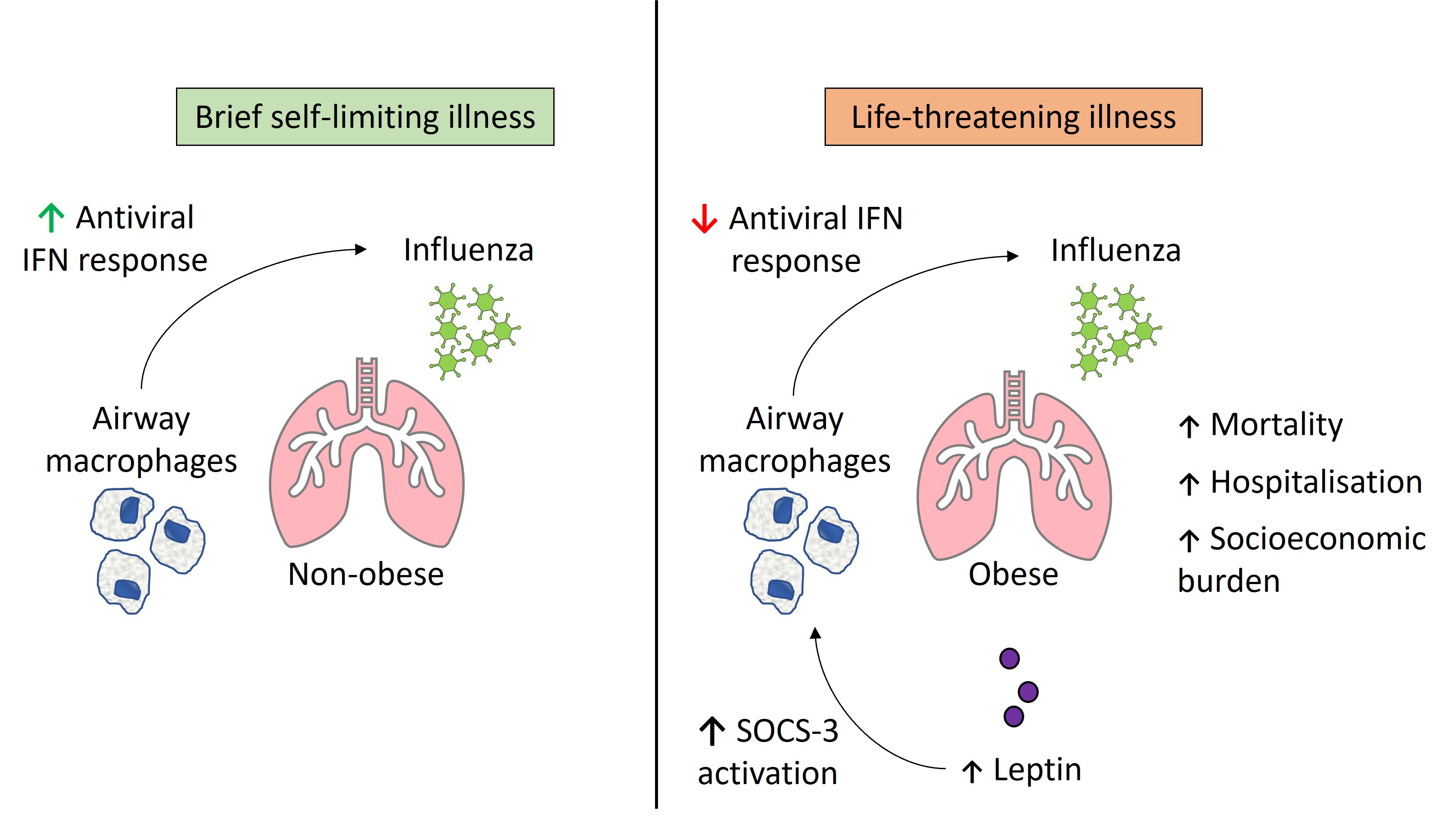
Figure: Proposed mechanism of leptin on antiviral interferon response to influenza infection via the induction of SOCS-3. IFN=interferon.
References
- Gaur, P. et al. Defective interferon amplification and impaired host responses against influenza virus in obese mice. Obesity (Silver Spring) 29, 1272–1278 (2021).
- Namkoong, H. et al. Obesity worsens the outcome of influenza virus infection associated with impaired type I interferon induction in mice. Biophys. Res. Commun. 513, 405–411 (2019).
- World Health Organisation. Obesity And Overweight (2021).
- Morgan, O. W. et al. Morbid obesity as a risk factor for hospitalization and death due to 2009 pandemic influenza A(H1N1) disease. PLoS ONE 5, e9694 (2010).
- Gao, M. et al. Associations between body-mass index and COVID-19 severity in 6.9 million people in England: a prospective, community-based, cohort study. Lancet Diabetes Endocrinol. 9, 350–359 (2021).).
Follow the Topic
-
Nature Communications

An open access, multidisciplinary journal dedicated to publishing high-quality research in all areas of the biological, health, physical, chemical and Earth sciences.
Ask the Editor - Immunology, Pathogenesis, Inflammation and Innate Immunity
Got a question for the editor about the complement system in health and disease? Ask it here!
Continue reading announcementRelated Collections
With Collections, you can get published faster and increase your visibility.
Women's Health
Publishing Model: Hybrid
Deadline: Ongoing
Advances in neurodegenerative diseases
Publishing Model: Hybrid
Deadline: Mar 24, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in