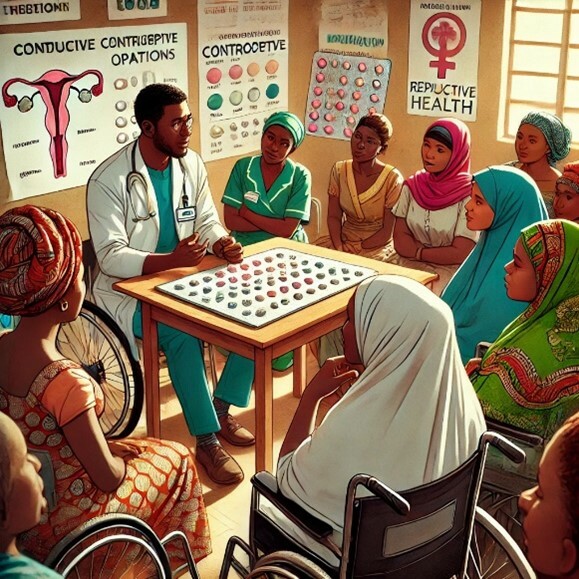
Are modern contraceptives for women with disabilities in Africa?
Published in Healthcare & Nursing, Social Sciences, and Public Health
The rapid growth of the global population includes a significant increase in the number of people living with disabilities. Currently, over 600 million individuals worldwide live with some form of disability, with an estimated 80 million residing in Africa. Notably, statistics show that there are more women with disabilities than men.
Globally, there are significant inequalities in accessing sexual and reproductive health services among women. However, this disparity is particularly alarming for women with disabilities, especially those in Africa. These women face numerous challenges in accessing the healthcare they need, including modern contraceptives, which are crucial for improving sexual and reproductive health.
Modern contraceptives have been one of the most effective tools for enhancing women's reproductive health. Despite the widespread acceptance and availability of these contraceptives since their invention, their use among women with disabilities in Africa remains noticeably low. This is concerning given the proven effectiveness of modern contraceptives, which have the potential to benefit this vulnerable population significantly. This also becomes imperative, considering the fact that these individuals are not asexual.
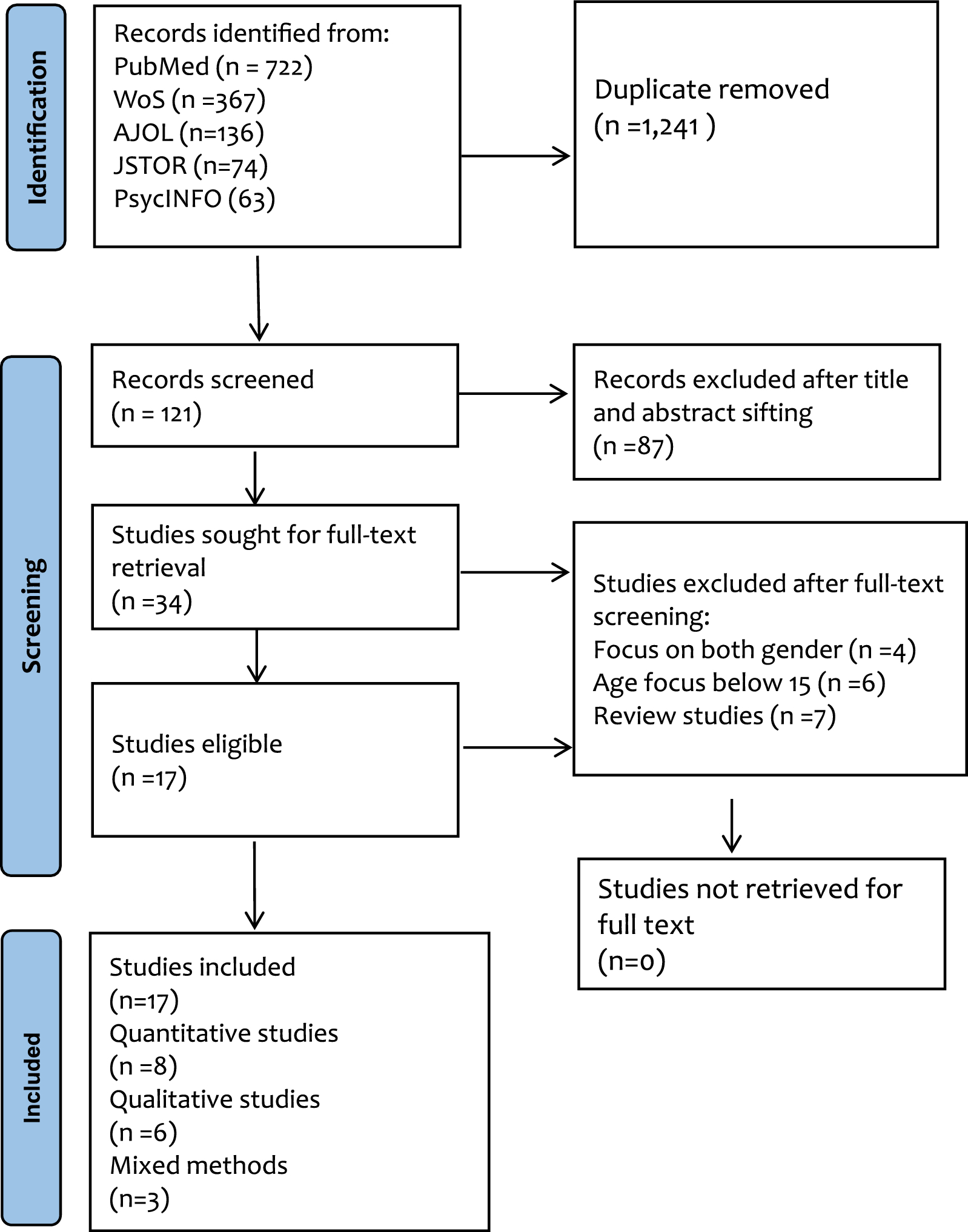
A recent scoping review led by Obasanjo Bolarinwa on improving the sexual health of women with disabilities in sub-Saharan Africa over the past 29 years, following the International Conference on Population and Development (ICPD) in Cairo, Egypt, in 1994. This conference established the concept of sexual and reproductive health and rights (SRHR). The review highlighted that the use of modern contraceptives among women with disabilities in Africa has been minimal, with various barriers preventing access to desired contraceptive methods. These barriers include physical accessibility issues, societal stigma, lack of targeted healthcare services, and insufficient education about contraceptive options.
As we observe World Contraception Day in 2024, it is essential to reflect on the progress made in the field of contraception and consider the inclusivity and gender equality aspects of this progress. It is critical that healthcare systems in Africa actively support and encourage the availability, distribution, and use of modern contraceptives among women with disabilities. To achieve this, all barriers related to access and utilisation disparities must be addressed, ensuring that women with disabilities can choose and use the contraceptives that best meet their needs.
Furthermore, logistics around the distribution of home-based modern contraceptives should be prioritised by policymakers and stakeholders. This approach would address the accessibility challenges faced by women with disabilities, enabling them to access and utilise contraceptives more effectively. By doing so, we can accelerate progress toward achieving the United Nations Sustainable Development Goals, particularly targets 3 (Good Health and Well-being) and 5 (Gender Equality).
In conclusion, ensuring that women with disabilities in Africa have access to modern contraceptives is not just a matter of health but also of equity and human rights. Concerted efforts must be made to eliminate the barriers these women face, allowing them to fully benefit from advancements in reproductive healthcare.
Follow the Topic
-
Reproductive Health

This journal focuses on all aspects of human reproduction, including adolescent health, female fertility, contraception, and maternal health and all articles are open access.
Related Collections
With Collections, you can get published faster and increase your visibility.
Reproductive Health Equity for Migrants, Refugees, and Internally Displaced Populations
This collection aims to assess disparities and barriers in access to maternal care, contraception, and safe delivery services among displaced populations —both within and across countries— compared to host communities in low- and middle-income countries (LMICs) and developed countries. Displaced populations often face significant challenges in accessing essential healthcare services, which can lead to poorer health outcomes for mothers and infants. These challenges include higher rates of maternal and infant mortality, due to inadequate access to quality maternal care and contraception, as well as increased rates of cervical and breast cancer, due to low rates of vaccination and inadequate screening.
The collection welcomes studies that explore various approaches to address these disparities, including:
• Improving cultural competency among healthcare providers. By understanding and respecting the cultural backgrounds of displaced populations, healthcare providers can offer more effective and personalized care.
• Increasing financial access to healthcare services. Many displaced individuals face financial barriers that prevent them from seeking necessary medical care. Strategies to reduce these financial obstacles can significantly improve health outcomes.
• Involving communities in the design and implementation of health programs. Community engagement ensures that health interventions are tailored to the specific needs and preferences of the populations they serve. This participatory approach can lead to more sustainable and impactful health programs.
• Encouraging innovative approaches and the implementation of relevant technologies among migrants and refugees.
• Raising awareness of prevention, screening, and access to care for cervical and breast cancers.
Overall, this collection aims to highlight innovative solutions and best practices to reduce health disparities and improve maternal and infant health among international and internally displaced populations.
This Collection supports and amplifies research related to SDG 1, No Poverty, SDG 3, Good Health and Well-Being, and SDG 10, Reduced Inequalities.
We are committed to supporting participation in this issue wherever resources are a barrier. For more information about what support may be available, please visit OA funding and support, or email OAfundingpolicy@springernature.com or contact the Editor-in-Chief.
Publishing Model: Open Access
Deadline: Mar 20, 2026

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in