Behind the scenes: researching long COVID and menstruation
Published in Social Sciences and Biomedical Research
What started as anecdotal whispers about irregular periods, heavier menstrual bleeding and skipped cycles, soon formed a pattern too consistent to ignore. It appeared that long COVID was affecting more than lungs and energy levels, it was perhaps rewriting hormonal rhythms. Women were understandably concerned and we listened.
Amplifying women’s voices
But finding reliable data was not easy. Many clinicians dismissed the connection, attributing menstrual changes to stress or natural variations in menstrual parameters. None of the clinical trials on COVID asked about menstruation, no health agency was logging these data. This meant we could not get answers quickly.
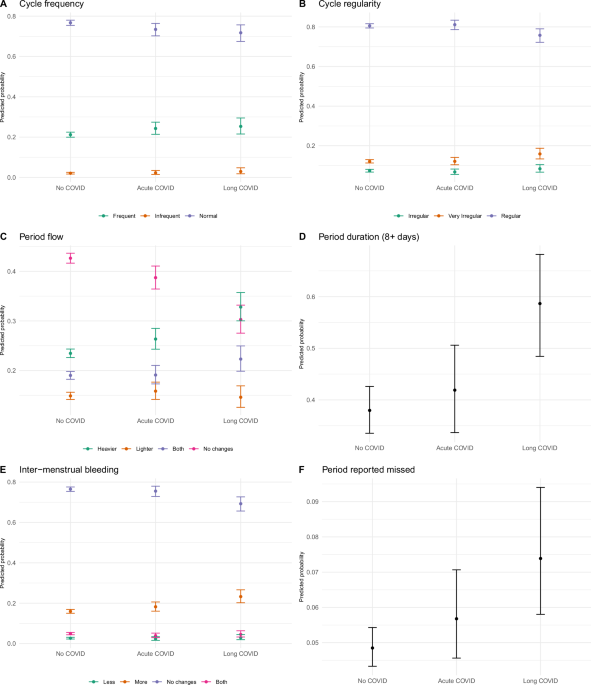
Undeterred, we brought together a multidisciplinary team of experts in gynaecology, anthropology, epidemiology and reproductive biology and developed an online survey on COVID-19 Pandemic and Women’s Reproductive Health. This went live in March 2021, and like so many events in science, serendipity prevailed. At this particular point in time, there were women who had never had COVID-19, those who had acute COVID and recovered well, and a group of women who had acute COVID and had persistent symptoms lasting >8 weeks. There were similar rates of vaccination across all three groups. This gave us a unique opportunity to compare menstrual symptoms in those who had and had never had COVID 19 - something that would be virtually impossible to do now. What we found was that those who developed long COVID reported increased menstrual volume, duration and intermenstrual bleeding, when compared to those who had never had COVID. While women who had recovered from acute COVID reported minimal menstrual disruption.
Reversing the direction
Alongside the understudied impact of COVID on menstruation, women in long COVID support groups were reporting exacerbations of their symptoms at different points in their menstrual cycle. There were also reports that long COVID was disproportionally affecting women, particularly those of reproductive age. This begged the question ‘How is the menstrual cycle affecting long COVID symptoms?’ To answer this, we set up an app-based long COVID symptom tracker for those who were menstruating regularly, where women could record the number and type of long COVID symptoms they experienced daily and rate the severity of each. We revealed that there was no difference in the number of symptoms that women experienced across the menstrual cycle but that the severity of long COVID symptoms was highest around the time of menstruation and into the first half of the cycle.

Not just what, but why?
More than finding associations, we wanted to delve deeper and examine potential mechanisms causing menstrual disturbance with Long COVID and the increased severity of long COVID symptoms around menstruation. To do this, we invited women with long COVID to attend for three research visits during a menstrual cycle. We collected blood samples and endometrial samples (the inner lining of the uterus that is shed during menstruation) in the first half of their cycle, in the second half of their cycle and during menstruation. For comparison, we examined blood and endometrium from a group of women who had provided samples prior to the COVID pandemic.
As researchers, we were very conscious that this was a significant ask from women who were already suffering with extremely debilitating symptoms. We worked closely with people with lived experience to design and refine our study and were overwhelmed by their desire for answers and willingness to participate in research.
A major limitation of our study is the lack of diversity in this group, despite significant efforts to reach underrepresented women. Given hospital restrictions at the time and the significant symptoms these women were experiencing, alongside the normal pressures of work and caring responsibilities for reproductive aged women, our numbers were understandably low. There are also cultural barriers to studying menstruation. Some people just don’t feel comfortable talking about their periods.
The altruism of those who did come forward to participate will always stay with us, we were blown away by their commitment, turning up repeatedly for biopsies and blood samples to advance knowledge about menstruation and long COVID. So, the pressure was on to deliver in the lab.
Doing a lot with a little
First, these precious endometrium and blood samples were carefully categorised for stage of the menstrual cycle using ovarian hormone blood levels and examination of the tissue by an expert pathologist. Next, we performed Liquid Chromatography-Tandem Mass Spectrometry (or LC-MS/MS for short) on the samples. This is technique allowed us to identify and quantify many hormones. We also checked hormone receptor levels in the endometrial tissue.
This revealed higher blood levels of 5α-dihydrotestosterone, one of the most active androgens, and lower endometrial androgen receptors in those with long COVID versus no COVID. This indicated that androgen levels (typically thought of as a male hormone but also present in women) may be altered in those with long COVID. Whether this is a cause or consequence of long COVID remains undetermined, but high androgen levels have previously been linked with menstrual disturbance.
Other ovarian hormones were reassuringly unchanged between the groups. Furthermore, AMH, a marker of ovarian function, was also similar in those with long COVID versus no COVID.
Next, we examined markers of inflammation in the blood using a multiplex ELISA. This technique allowed us to measure many factors in the samples. We showed increased inflammation at menstruation in those with long COVID versus controls. We also observed clumps of immune cell in the menstrual endometrial tissue from those with long COVID that were not present in women who had never had COVID.
Moving forward
Overall, we showed that long COVID was associated with menstrual disturbance but not impaired ovarian function. Higher levels of androgens or inflammation may contribute to menstrual disturbances in those with long COVID and may also influence long COVID symptom severity during menstruation.
This increased understanding of the impact of long COVID on menstruation is the first step towards the development of evidence-based treatments for those suffering with menstrual disturbance. We also hope it will instigate exploration of sex specific treatments for women with long COVID. One of the lessons from the COVID pandemic is that menstrual health isn’t a niche issue. It’s a vital part of the long COVID story and we’re listening.
Banner image: Lesia Lerionova via Getty Images. Symptomatic woman image in main blog: Mary Long via Getty Images.
Follow the Topic
-
Nature Communications

An open access, multidisciplinary journal dedicated to publishing high-quality research in all areas of the biological, health, physical, chemical and Earth sciences.
Related Collections
With Collections, you can get published faster and increase your visibility.
Women's Health
Publishing Model: Hybrid
Deadline: Ongoing
Advances in neurodegenerative diseases
Publishing Model: Hybrid
Deadline: Mar 24, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in