Developing Diagnostics for Global Health
Published in Microbiology

When the McGill Summer Institute for Global Health Diagnostics started in 2015, the aim of its founders and co-directors, Professor Madhukar Pai, Dr Cédric Yansouni and Dr Nitika Pant Pai, was to mobilise research and resources for a much neglected area of global health. Today, diagnostics still fall behind drugs and vaccines in terms of global health funding, for example receiving only 9% of total funding for TB R&D throughout 2009-2016, making diagnostics R&D 86% underfunded compared with Global Plan Funding Targets. Commercial companies have a relatively poor record of developing diagnostics aimed at low and middle-income countries (LMICs), largely due to the perceived limited market and lack of profitability.

The course programme and panels reflected the broad range of participants represented at this year's Summer Institute, from industry partners and programme directors, to patients and community advocacy groups. The atmosphere was engaging and collaborative, with course co-director Dr Nitika Pant Pai opening the meeting with a positive tone to a week of sharing experiences and frustrations alike, assuring participants "there are no mistakes, only lessons".

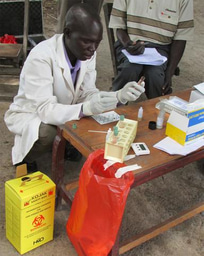
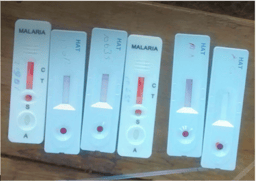
Despite diagnostics' relative neglect on the global health agenda, huge strides have also been made and the challenges that the presenters and participants at the Summer Institute are grappling with are very different to those of a decade ago. The development and scale up of GeneXpert machines is enabling more rapid and accurate detection of TB cases, including rifampicin resistance in a single test, allowing for early and appropriate initiation of treatment. However, questions remain over how well machines are rolled out, integrated, and supported in weak health infrastructures. The mass roll-out of malaria RDTs has transformed the diagnostic algorithm for febrile illnesses, setting the stage for the proliferation of rapid point of care tests from HIV to sleeping sickness, each with their own disruptions to local diagnostic ecosystems. The volatile market of diagnostic devices and evolving attitudes regarding the role of diagnostics among the global health community recently culminated in the WHO’s launching of the Essential Diagnostics List (EDL), which arose out of discussions at the Summer Institute in 2017. At this year’s Global Health Diagnostics course, approximately 100 participants from over 30 countries, representing public health, policy, industry, donors, lab professionals, and community based organisations were now in a position to reflect with hindsight on the diagnostic innovations that have taken place in recent years, and look forward to new challenges on the horizon.

Throughout the week we talked a lot about landscapes, from epidemiological landscapes, regulatory and funding landscapes, to patient landscapes of care. The course and discussion panels allowed for a cross pollination of intersecting issues, from ruthless market forces faced by industry, to the marginalisation of central lab capacity by the global health community. As Prof Peter Dailey of University of California Berkeley surmised at the beginning of his presentation on optimizing multi-disease testing platforms, “this is when landscapes collide”. What does the current diagnostic landscape look like and where do we go from here?
These are some of the questions being explored by the DiaDev project, a new partnership between the University of Edinburgh, Kings College London, Kings Health Partners, and Public Health Foundation India. Through the mapping of diagnostic infrastructures and collaborations with stakeholders, DiaDev traces some of the unpredictable biographical trajectories of diagnostic devices as they travel through research laboratories, manufacturing plants, regulatory bodies, clinics, and ministries of health.
ACKNOWLEDGMENTS
This project has received funding from the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation programme under grant
agreement No 715450.


The author would like to thank Professor Madhukar Pai and Dr Alice Street for their helpful comments and input on this series. The author acknowledges the lands of the Abenaki/Abénaquis, Haudenosauneega, Huron-Wendat, Kanien'kehá:ka, and Mohawk on which the Summer Institute takes place.



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in