Does glandular fever increase the risk of inflammatory bowel disease?
Published in Public Health
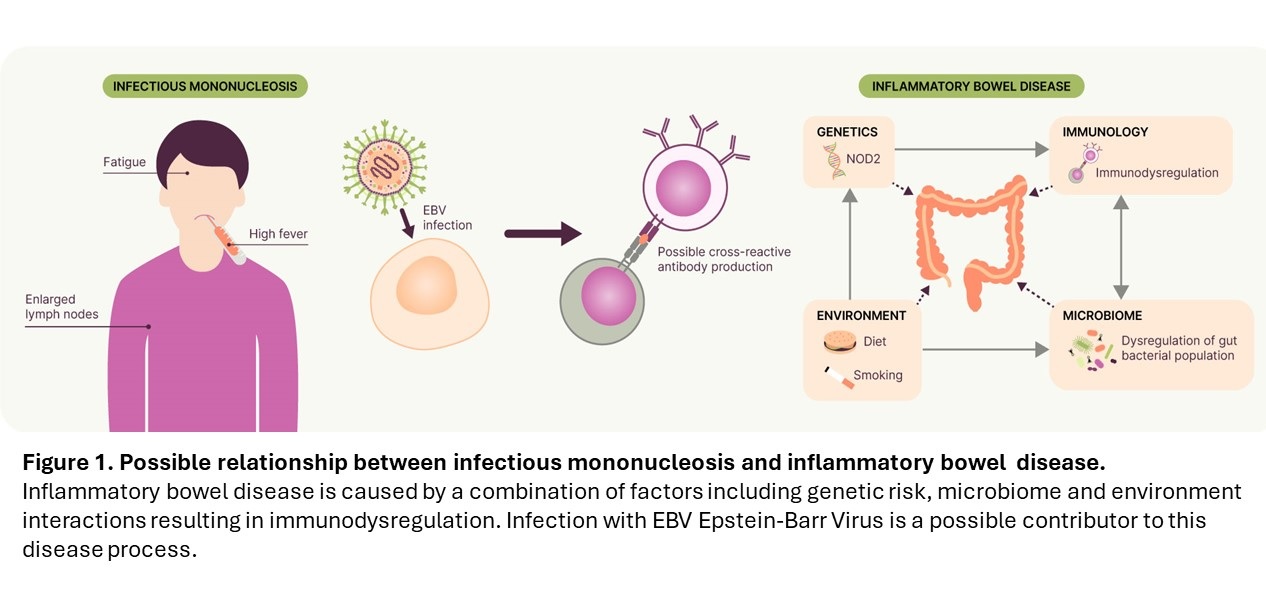
Infectious mononucleosis (IM), also known as glandular fever, ‘mono’ or ‘kissing disease’, is a common syndrome which is characterised by symptoms of fever, tiredness, and enlarged lymph nodes. In the vast majority of cases, the disease is caused by infection with the herpesvirus, Epstein-Barr Virus (EBV). Primary infection with EBV usually occurs in childhood or early adulthood with a silent seroconversion or symptomless infection and development of antibodies to the virus. However, in approximately 5% of acute infections, IM is associated with severe disease presenting with high fever, generalised lymphadenopathy and extreme fatigue, due to an aggressive over production of mononuclear leukocytes that gives the disease its name. Associations between IM and several autoimmune diseases, including rheumatoid arthritis, systemic lupus erythematosus, and multiple sclerosis have previously been identified however the risk of developing the inflammatory immune-mediated diseases inflammatory bowel disease (IBD) following IM is unclear.
Our study and what we found
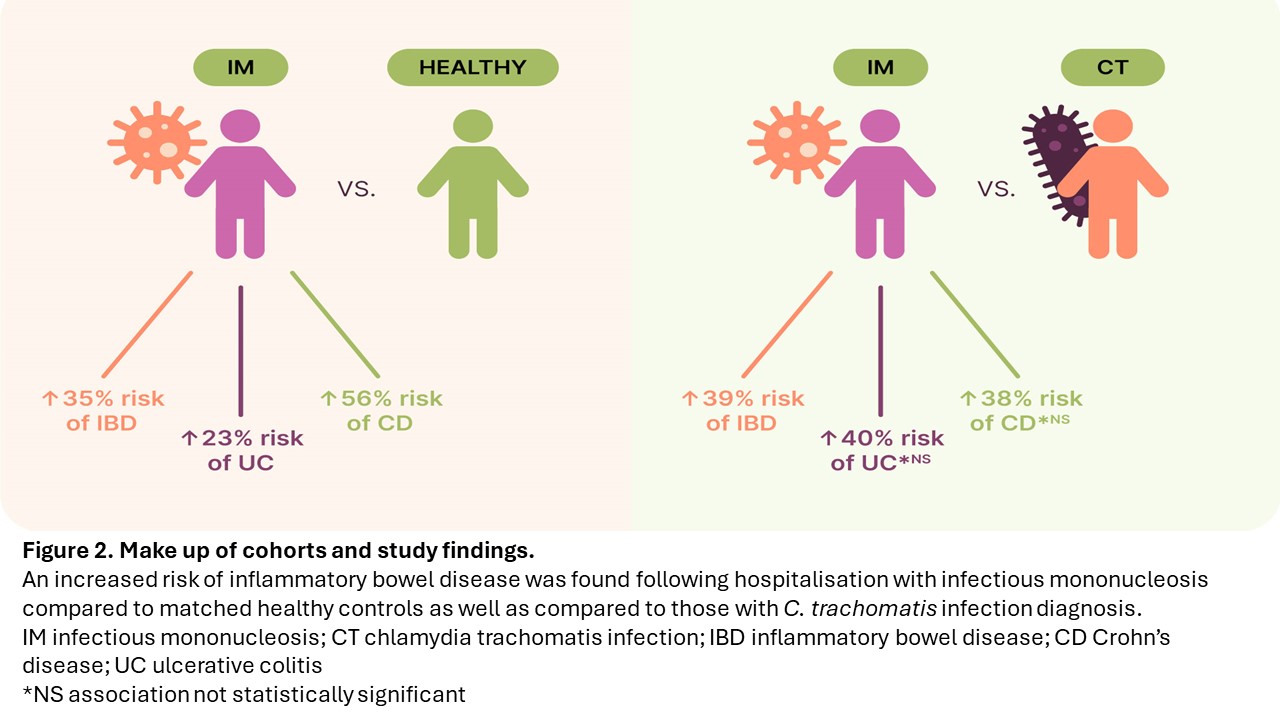
We used data from almost 40,000 patients with IM and almost 400,000 patients without a recorded IM diagnosis, sampled at random and matched on the basis of age, socio-economic area of residence, and sex, between January 1977 and December 2021 in Denmark to assess the risk of developing IBD following hospitalisation with IM. When compared to those patients who were not hospitalised with IM, those with IM disease had a 35% (22-49%) increased risk of IBD later in life. This risk was seen particularly for the development of the IBD subtype, Crohn’s disease, for which there was a 56% (34-83%) increased risk, following IM.
Findings were consistent across age groups with a 20-60% increased risk of IBD following IM in those diagnosed with IM before the age of 30 years. Interestingly, there was a particularly strong association with the development of Crohn’s disease in those hospitalised with IM before the age of 10 years, indicating a particular vulnerability to Crohn’s in those developing severe infection with EBV and IM disease very early in life.
In order to test whether findings were due to a systemic ascertainment bias, i.e., whether patients diagnosed with IM were more likely to be diagnosed with IBD due to a difference in health seeking behaviour, we undertook the same analysis using a negative control group. For this we matched patients diagnosed with IM, to patients diagnosed with Chlamydia trachomatis (CT) infection, another disease commonly associated with adolescence and young adults, which is similarly primarily diagnosed via primary healthcare providers in Denmark. We used propensity score matching to weight the cohort of patients with CT infection to those with IM diagnosis on the basis of age, socio-economic area of residence and sex. Following this rigorous sensitivity analysis, we continue to find a significant association between IM and IBD, with a 39% increased risk of IBD development following IM diagnosis compared with CT diagnosis.
Interestingly, there was a particularly strong association with the development of Crohn’s disease in those hospitalised with IM before the age of 10 years, indicating a particular vulnerability to Crohn’s in those developing... IM disease very early in life.
Conclusion
This work indicates that hospitalisation with infectious mononucleosis is significantly associated with an increased risk of developing inflammatory bowel disease later in life. Our data shows that this association is seen in those developing IM across all ages under 30 years old, in both men and women, and that IM is particularly associated with the Crohn’s disease IBD subtype when hospitalisation occurs very early in life (below 10 years old). The causes of IBD are complex and not fully understood, this work contributes to our understanding of the potential environmental risk factors associated with disease onset.
Follow the Topic
-
Nature Communications

An open access, multidisciplinary journal dedicated to publishing high-quality research in all areas of the biological, health, physical, chemical and Earth sciences.
Related Collections
With Collections, you can get published faster and increase your visibility.
Women's Health
Publishing Model: Hybrid
Deadline: Ongoing
Advances in neurodegenerative diseases
Publishing Model: Hybrid
Deadline: Mar 24, 2026





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in