Exploring the Connection Between the Oral Microbiome and Mental Health
Published in Sustainability and Biomedical Research
The Oral-Brain Axis: What Is It?
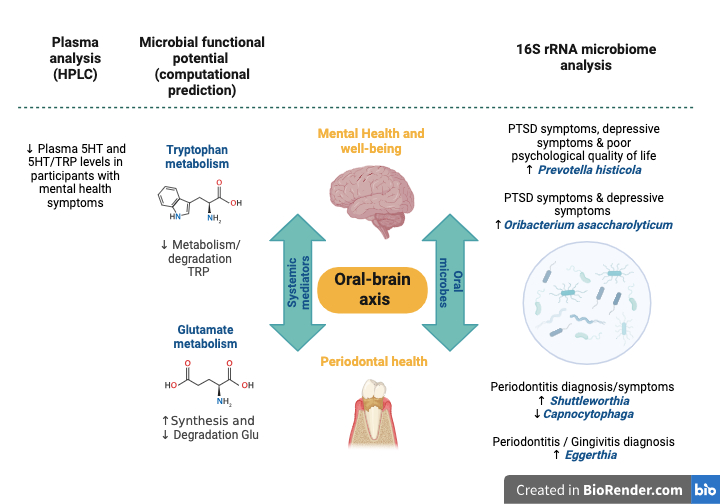
You may have heard of the gut-brain axis, describing the connection between our gut microbiota and mental health. Similarly, we are now beginning to understand the oral-brain axis—a concept that suggests the microbiome could also play a critical role in mental well-being. The oral cavity houses an extensive collection of microbes, the oral microbiome, which comprises diverse bacterial species that can influence inflammation, immune response, and even brain chemistry. Periodontitis is a common, long-lasting gum infection caused by bacteria, affecting nearly half of the world’s population. It leads to inflammation in the body by triggering the release of immune signalling molecules that promote inflammation. In addition to being linked to other health problems like heart disease, diabetes, and atherosclerosis, research suggests that periodontitis may also be connected to mental health problems, highlighting a possible link between oral health and brain function.
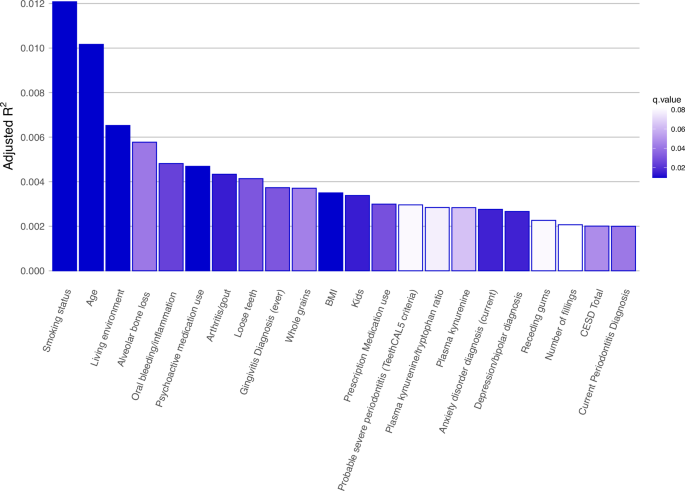
In our study, we focused on a large cohort of 470 participants, 306 of whom reported mental health symptoms and current diagnoses of depression, anxiety, and post-traumatic stress disorder (PTSD). We also collected periodontal data from participants (including diagnoses and symptoms of periodontitis or gingivitis). By utilizing 16S rRNA sequencing, we characterized the microbiome composition of their saliva and compared it to that of 164 mentally healthy controls. We also investigated associations between the oral microbiome and periodontal symptoms and diagnoses. Lastly, we also predicted the functions of the oral microbes and verified it in plasma samples to identify possible connections between periodontal and mental health.
Key Findings:
Our research revealed intriguing correlations between specific microbial populations and mental health symptoms.
- Mental and periodontal health significantly affect the makeup of the oral microbiome: Symptoms of depression, as well as a diagnosis of depression or an anxiety disorder, self-reported diagnoses of gingivitis or periodontitis, and signs of severe gum disease influenced the overall makeup of the oral microbiome.
- Depression and Anxiety Links: The levels of Prevotella histicola (P. histicola) were higher in participants with depressive symptoms and those with poor psychological quality of life. Higher levels of Oribacterium asaccharolyticum were detected in individuals diagnosed with anxiety disorders and in those with depressive symptoms, whilst individuals diagnosed with anxiety disorders also had lower levels of Neisseria elongate.
- Trauma and the oral microbiome: Participants who experienced emotional neglect during childhood exhibited higher levels of Streptococcus mutans. Individuals with PTSD symptoms had lower levels of Haemophilus sputorum and higher levels of P. histicola, similar to those with depressive symptoms and lower psychological well-being (Fig.1).
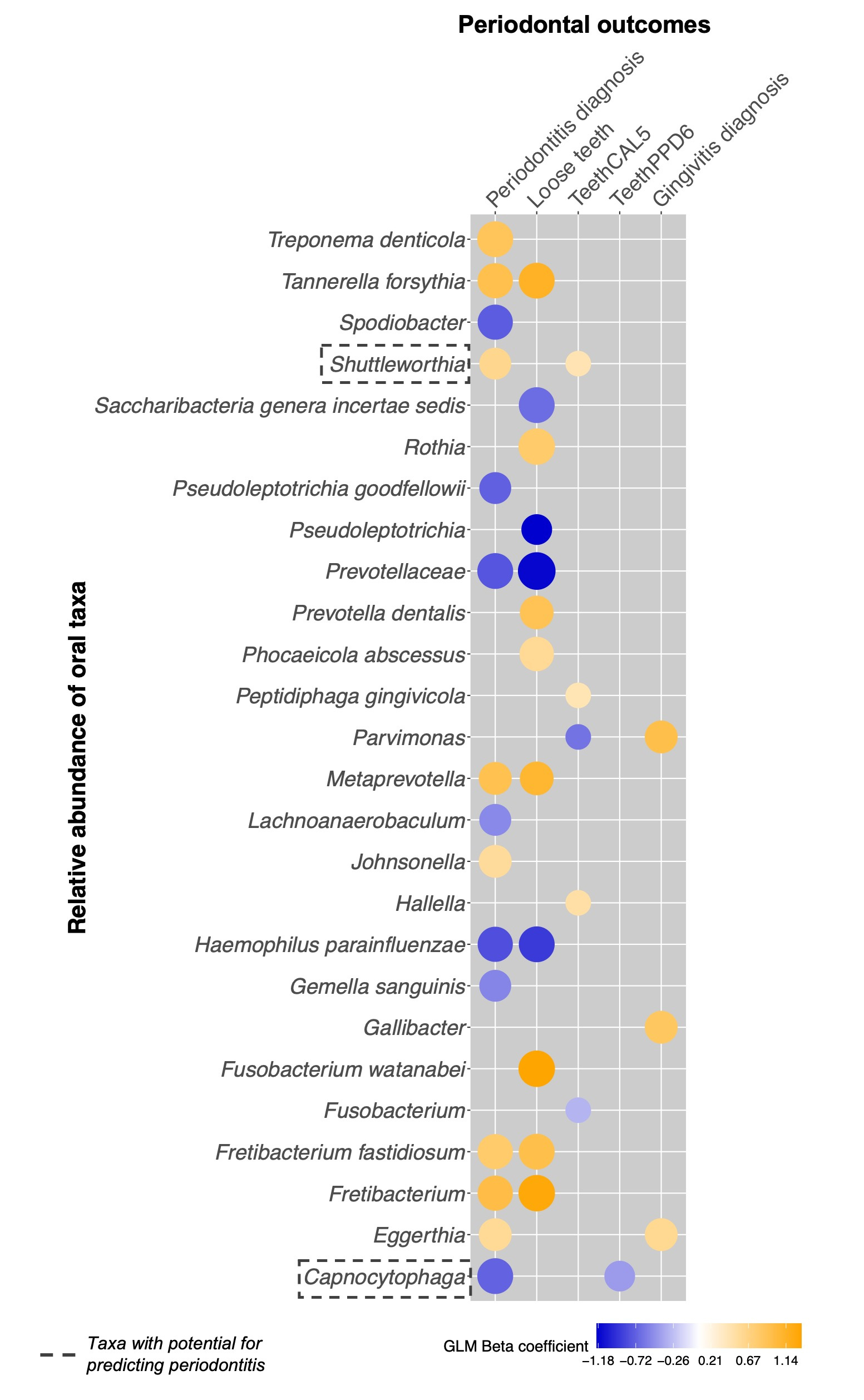
- Periodontal Health Matters: We also noted several significant links between periodontal health and the abundance of salivary microbes. Higher levels of Shuttleworthia and lower levels of Capnocytophaga were found in individuals with clinical periodontitis and those with predicted severe periodontitis. One feature that was common between participants with a diagnosis of gingivitis and periodontitis was higher levels of Eggerthia compared to periodontal controls (Fig.2).
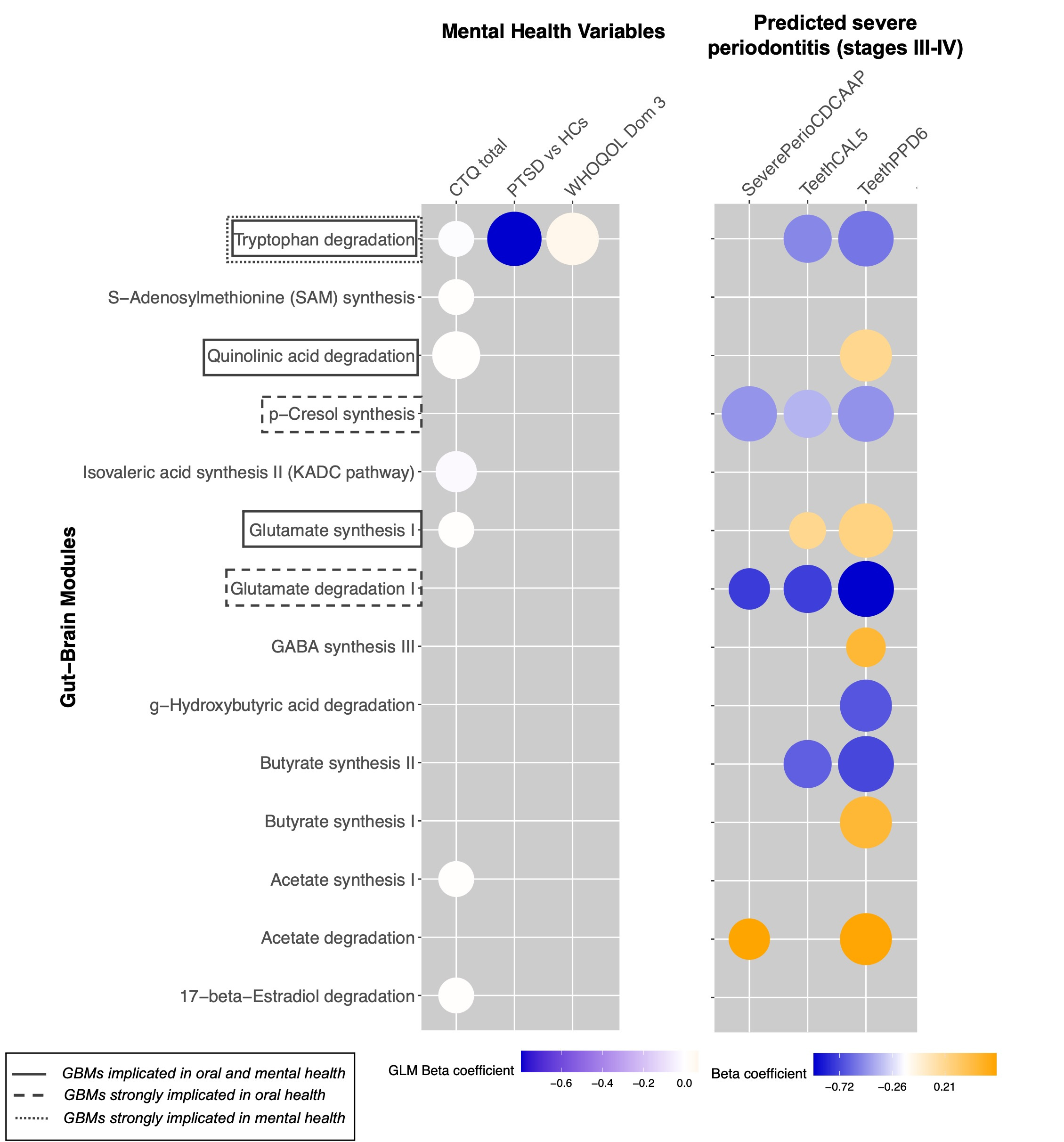
- Tryptophan Metabolism - A Potential Link: Although we didn't find any specific bacteria linked to both mental and periodontal health, we did discover a potential common biological process linked to the oral microbiome, mental and periodontal health: the breakdown of tryptophan (TRP). This process was reduced in people with PTSD, childhood trauma, poor social relationships, and those with possible periodontal disease. Lower tryptophan breakdown could lead to lower serotonin levels, which may affect mood. We found lower plasma serotonin levels among participants with mental health symptoms, indicating a possible metabolic link between oral microbiota and mental health (Fig.3).
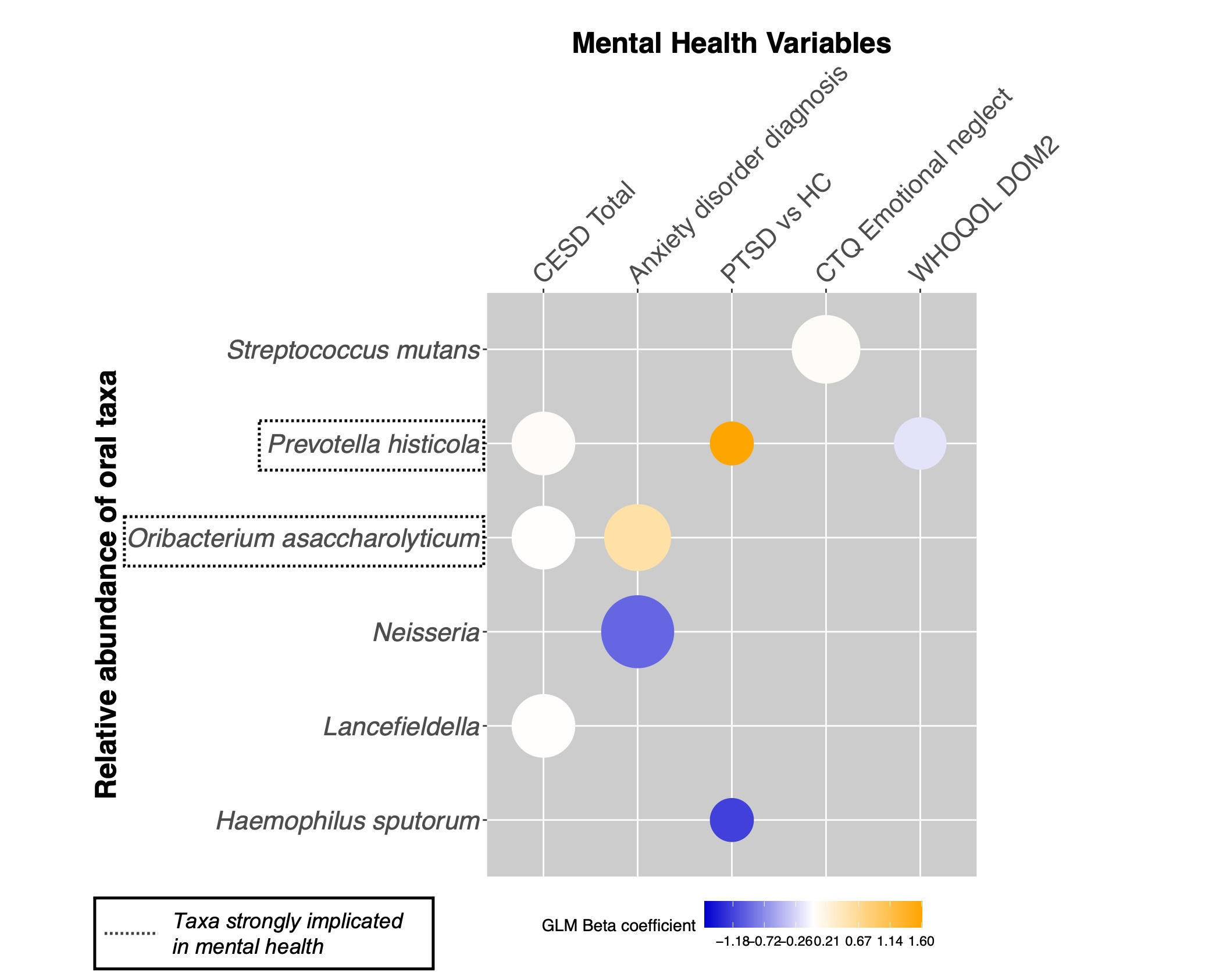
Fig.1: Summary graphic highlighting common taxa associated with mental health outcomes, trauma, and wellbeing (positive associations are indicated in yellow tones, negative associations in blue tones, color intensity is proportional to standardized GLM β coefficients, and point size is proportional to the q-values (FDR corrected p-values)).
Implications for Future Research and Treatment
Our study highlights the links between oral microbes and periodontal and mental health.
While these findings are promising, they also raise several important questions:
- Do the oral bacteria cause/contribute to mental health symptoms? Our study only shows a link between the types of bacteria in the mouth and mental health symptoms at a single point in time. To understand if the bacteria actually cause these symptoms, future studies that track changes over time are needed.
- Can oral health interventions improve mental health? Given our results, exploring the potential of dental care and oral hygiene as therapeutic tools in mental health treatment could be a promising area for future research.
- What mechanisms underlie these microbiome changes? Understanding the biological pathways connecting the oral microbiome to mental health is crucial. We need to explore how specific bacterial populations influence brain function and emotional regulation.
Conclusion
The relationship between the oral microbiome and mental health is a burgeoning field of study with immense potential for novel therapeutic interventions. Our research sheds light on the intricate connections between these domains, emphasizing the need for further exploration.
As we unravel the mysteries of the oral-brain axis, we invite you to consider the importance of maintaining good oral health—not just for a bright smile but also for mental well-being.
Follow the Topic
-
Translational Psychiatry

This journal focuses on papers that directly study psychiatric disorders and bring new discovery into clinical practice.
Related Collections
With Collections, you can get published faster and increase your visibility.
Moving towards mechanism, causality and novel therapeutic interventions in translational psychiatry: focus on the microbiome-gut-brain axis
Publishing Model: Open Access
Deadline: May 19, 2026
From mechanism to intervention: translational psychiatry of childhood maltreatment
Publishing Model: Open Access
Deadline: Jun 30, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in