From Status Symbol to Silent Epidemic: The Complex Relationship Between Obesity, Food Insecurity, and Liver Health
Published in General & Internal Medicine, Public Health, and Agricultural & Food Science

For centuries, in many cultures, larger body size has been seen as a marker of prosperity, fertility, and social status. But in today’s world, this perception is colliding with a stark reality: obesity is increasingly linked to food insecurity, poor nutrition, and preventable chronic diseases such as metabolic dysfunction-associated steatotic liver disease (MASLD) and diabetes type 2.
On World Obesity Day 2025, we explore the paradox of modern malnutrition: Why are food-insecure communities disproportionately affected by MASLD? How do socioeconomic disparities, aggressive marketing, and low food literacy contribute to an unhealthy cycle of liver disease? And, most importantly, what can be done to break the link between food inequity and metabolic disease?
To help answer these critical questions, we will answer three key questions that contributed to our recent review “Food inequity and insecurity and MASLD: burden, challenges, and interventions” (Nature Reviews Gastroenterology & Hepatology).
Key Questions for the Researcher:
If obesity was historically seen as a sign of wealth and prosperity, why is it now linked to poor health outcomes like MASLD?
In June 2013, the American Medical Association (AMA) recognised obesity as a chronic disease with multifactorial aetiology, including genetics, metabolism, environment, lifestyle, and behavioural components. This, in turn, has substantially shifted how obesity is viewed, underpinning complex risk factors rather than just lifestyle choices.
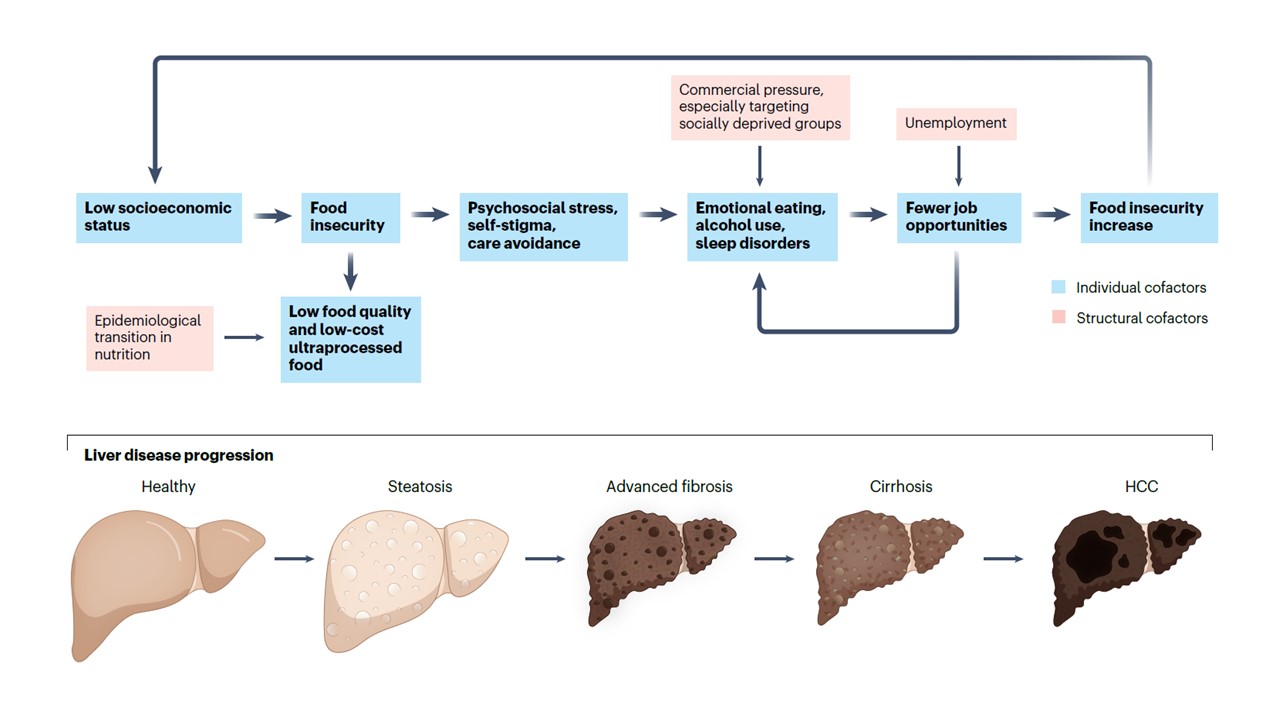
Obesity is closely related to additional metabolic diseases such as type 2 diabetes and MASLD. People living with obesity face a 3.5 times higher risk of developing MASLD, compared to those living with a normal weight. MASLD is characterised by fat accumulation within the liver (hepatic steatosis) without secondary causes (e.g., significant alcohol or drug intake). Without adequate care, MASLD can progress to an inflammatory phase known as metabolic dysfunction-associated steatohepatitis (MASH), fibrosis and cirrhosis.
MASLD is the most common liver disease globally, and on 19 April 2025, World Liver Day will have the theme 'Food is Medicine'.
How does food insecurity contribute to liver disease, and what role do unhealthy diets play in MASLD?
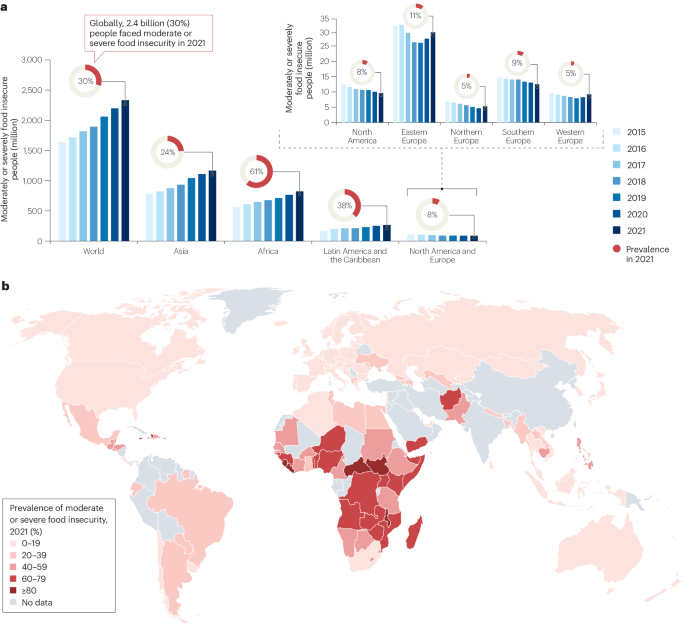
Food insecurity refers to inconsistent access to enough food for a healthy, active life; it is a major structural determinant of health. Beyond food quantity, food insecurity is also related to food quality; in other words, it can represent the limited availability of affordable nutritious food and even water. This could mean that a person is overweight, yet experiencing food insecurity because of the low-quality food being consumed.
Food insecurity is prevalent in socially deprived communities and negatively affects their nutritional choices and health. Take, for example, when healthy foods like vegetables, fruits, nuts, legumes, olive oil, and fish are expensive or scarce, but fast food is easily obtainable. Western diets have become characterised by high consumption of ultra-processed food, fast food, soft drinks and alcohol, which are associated with worse metabolic health including MASLD as well. When the built and social environments promote the adoption of a Western diet over the recommended Mediterranean diet (or similar plant-based dietary pattern), it increases the risk of MASLD at the individual level.
People experiencing food insecurity often face psychological stress and self-stigma, which can lead to emotional eating, increased alcohol consumption, and even fewer job opportunities. These factors may further worsen food insecurity and negatively impact metabolic health.
What can we do to address the link between food insecurity and MASLD?
There are only a few studies investigating the association between food insecurity and MASLD, most of them were conducted in the United States. Thus, the first priority should be strengthening research efforts to underscore the social and environmental determinants of MASLD, as was previously indicated in a global research agenda. In our review, we outlined essential actions and evidence-based initiatives to address MASLD, liver disease as a whole and food insecurity.
Here are some examples of required actions:
Policy and environmental changes
- Increase taxes for unhealthy food and reduce taxes for healthy food
- Restrict advertising and marketing of unhealthy food and beverages
- Reformulate unhealthy foods
- Safe outdoor green spaces for physical activity
- Front-off-pack food labeling including the number of added sugar teaspoon
- Prioritise public health interests concerning food
- Walkable access to affordable healthy foods
Healthcare and community strategies
- Routinely screen for food insecurity
- Incorporate socioeconomic inequities and food insecurity into clinical practice guidelines
- Offer economic incentives for healthy foods
- Offer healthy school and workplace lunches
- Promote healthy lifestyle community initiatives
- Provide patients and those at risk with reliable and clear information on healthy lifestyle choices
- Provide or refer for mental health screening and care
We must undertake a multi-level approach that engages clinicians, public health and community experts, patient organisations, and policy-makers as emphasised in the global action priorities agenda. By implementing the recommended actions and strengthening the evidence base, we can improve patient care and better address the high MASLD burden globally.
Follow the Topic
-
Nature Reviews Gastroenterology & Hepatology

The basic, translational and clinical content in this journal is written by internationally renowned basic and clinical academics and researchers and targeted towards readers in the biological and medical sciences, from postgraduate level upwards.

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in
This blog entry strikes me as exemplary. However, I have a couple of remarks that I believe to be of paramount importance, both concerning education.
Firstly, the education of the medical and health collective as a whole. Undoubtedly, many of us have failed, and continue to fail, to appropriately appreciate individuals living with obesity and its consequences. Despite being recognized as a disease, this diagnosis is often omitted in most patient clinical records; we frequently fail to advise any lifestyle modification (and when we do, it is done in an utterly generic manner), and ultimately, our approach is not always empathetic and only serves to increase stigmatization. As if this scenario were not of extreme significance, medical schools do not teach us to prescribe either a healthy diet or appropriate exercise. In truth, we are taught nothing—or very little—of what could be termed medicine of healthy lifestyle. Thus, it is imperative to educate healthcare personnel on this true pandemic.
Secondly, as we know, excess adiposity largely originates in our early years, placing the role of early childhood educators and teachers at the forefront. Likely, their training is also inadequate, facing considerable limitations to advise their students on the best possible lifestyle, informing them of the consequences both short-term and, especially, long-term. Such education is something educators can expand upon once they receive it. In this respect, neither doctors nor other health personnel have made a sufficient effort.
Food insecurity refers to inconsistent access to sufficient food for a healthy and active life but is also linked to the quality of the food available. Undoubtedly, it may signify the limited availability of nutritious, affordable food, and even water, due to economic hardships. However, it can also result from poor choices by individuals due to inadequate or non-existent information on the subject. In other words, within an obesogenic environment such as ours, the absence of even basic formal education in nutrition can become a pivotal factor in the onset and perpetuation of obesity.
In conclusion, education in all its dimensions, affecting all stakeholders involved (health professionals, educators, teachers, and society at large), will be crucial in halting the continuous rise in the prevalence of this disease and, gradually, reversing the obesity curve in our Western societie. Such education, which should include the concept of "social nutrition" (https://www.nature.com/articles/s43856-023-00398-3, a concept that educators can expand upon once they receive it.
Javier Crespo. Clinical and Traslational Research in Digestive Diseases, Valdecilla Research Institute (IDIVAL), Marqués de Valdecilla University Hospital, Santander, Spain
Thank you, Javier, for your insightful comment! I completely agree with all the points you raised. Preventing metabolic disease should begin as early as the embryonic stage and include education on healthy eating and behavior during the first 1,000 days and throughout the entire lifespan. We definitely have a lot of work to do to accomplish this aim.