Impact of nutrition counseling on dietary improvements, glycemic control, and neonatal outcomes in pregnant women with pregestational diabetes mellitus
Published in Healthcare & Nursing, General & Internal Medicine, and Public Health
Background
Pregestational diabetes mellitus (PGDM) poses significant risks for both mothers and their infants, including macrosomia and neonatal hypoglycemia. Nutrition management is a key component of prenatal diabetes care, yet its real-world effectiveness in Asian clinical settings remains underexplored.
Study Overview
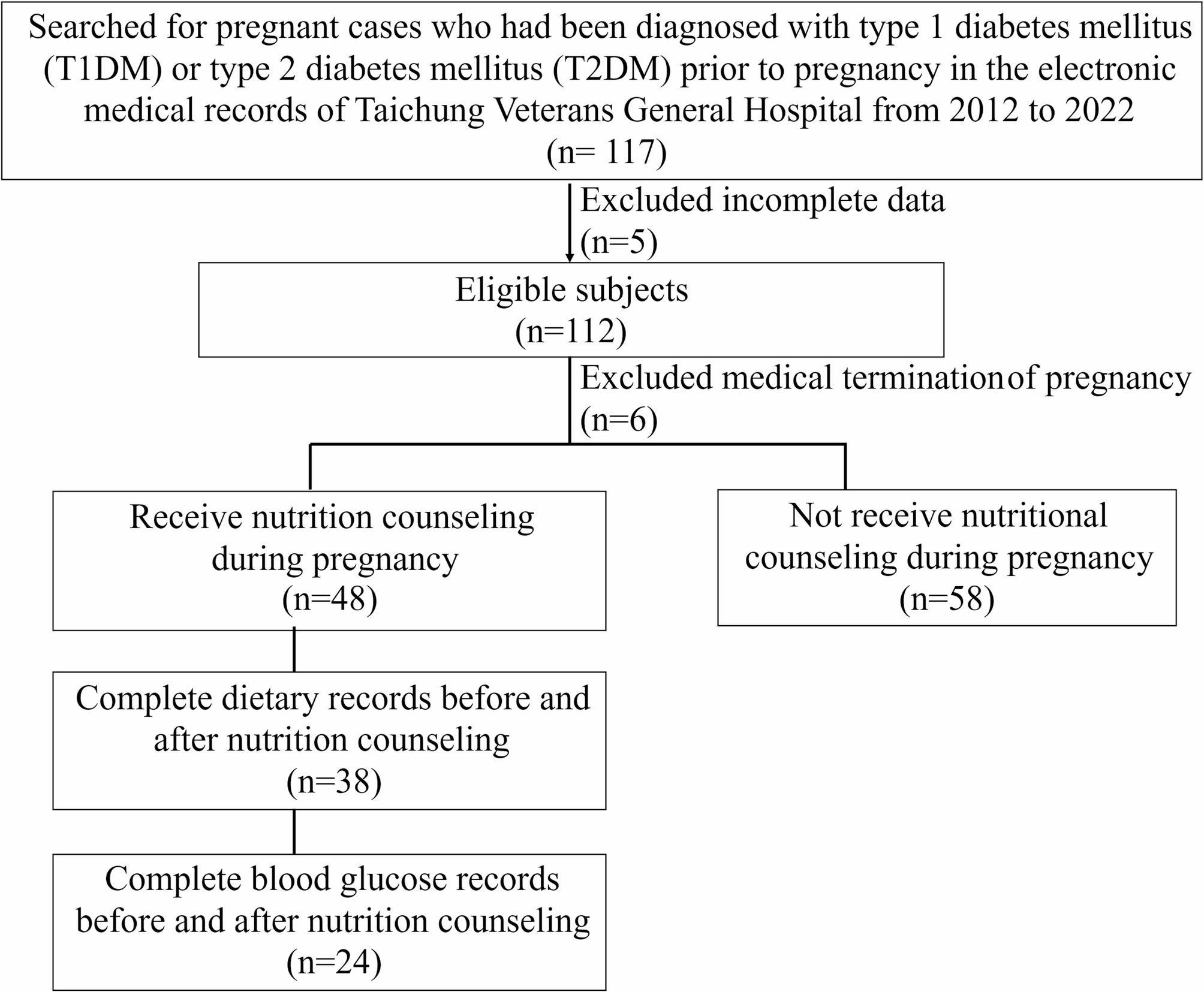
This retrospective study analyzed electronic medical charts from a tertiary medical center to assess how individualized nutrition counseling influenced dietary behavior, glycemic control, and neonatal outcomes in women with PGDM. Participants received structured dietary guidance provided by registered dietitians as part of multidisciplinary prenatal care.
Main Findings
After counseling, participants demonstrated marked improvements in dietary balance and nutrient intake. Consumption of vegetables, dairy products, and whole grains increased significantly, aligning more closely with national dietary guidelines.
Glycemic control also improved: both fasting and postprandial glucose levels decreased following dietary intervention, suggesting enhanced adherence to meal planning and carbohydrate distribution.
Importantly, positive changes in maternal nutrition were associated with better neonatal outcomes. The incidence of large-for-gestational-age infants and neonatal hypoglycemia declined among women who followed nutrition recommendations consistently. These findings highlight the clinical value of personalized nutrition counseling as a non-pharmacological approach to optimize pregnancy management in women with preexisting diabetes.
Implications for Practice
This study emphasizes that nutrition counseling should be an integral part of routine prenatal care for women with PGDM. Early referral to dietitians allows timely dietary modification and supports multidisciplinary coordination among obstetricians, endocrinologists, and nutrition professionals.
Beyond glycemic control, improving maternal diet quality contributes to healthier birth outcomes and long-term metabolic benefits for both mother and child. Our findings provide evidence-based support for the implementation of structured nutrition services in tertiary hospitals and diabetes-in-pregnancy clinics across Asia.
Reference
Follow the Topic
-
BMC Pregnancy and Childbirth

This is an open access, peer-reviewed journal that considers articles on all aspects of pregnancy and childbirth. It welcomes submissions on the biomedical aspects of pregnancy, breastfeeding, labor, maternal health, maternity care, trends and sociological aspects of pregnancy and childbirth.
Related Collections
With Collections, you can get published faster and increase your visibility.
Fetal and placental surgery
BMC Pregnancy and Childbirth is calling for submissions to our Collection on Fetal and placental surgery.
Fetal and placental surgery represents a rapidly evolving field that aims to address congenital anomalies and complications during pregnancy through in-utero interventions. These surgical techniques, which can include procedures such as fetoscopy and placental surgery, enable clinicians to treat conditions that may adversely affect fetal development, health, and survival. Placental surgery encompasses a variety of interventions, including but not limited to, the treatment of placental insufficiency, the management of placenta previa, and the correction of placental vascular anomalies. As technology and surgical techniques advance, this area of medicine continues to expand, offering promising new avenues for intervention that can significantly enhance neonatal outcomes.
The Collection invites researchers and clinicians in fields including maternal-fetal medicine, obstetrics and obstetrical surgery, and neonatology, to contribute research that explores topics including, but not limited to, in-utero surgical techniques, emergency obstetric practices, recent advancements in minimally invasive techniques, and outcomes associated with these interventions.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Jun 10, 2026
Respectful maternity care - Part II
BMC Pregnancy and Childbirth is calling for submissions to our Collection on Respectful maternity care - Part II.
The World Health Organization defines respectful maternity care (RMC) as care that maintains dignity, privacy, and confidentiality of pregnant and birthing women, ensures freedom from harm and mistreatment, and enables informed choice and continuous support during labor and birth. RMC is considered a fundamental human right. Despite the acknowledged importance of providing RMC to all women, many women still experience disrespect and abuse during labor and birth across global contexts.
BMC Pregnancy and Childbirth is calling for submissions on ‘Respectful maternity care’ to bring together research on the benefits of respectful maternity care and the challenges in its implementation, both at the provider level and the system level. Both qualitative and quantitative research are welcome. Topics of interest include, but are not limited to, prevalence of disrespect and abuse in maternity care, implementation of respectful maternity care, RMC and maternal and neonatal outcomes, interventions to enhance and promote RMC, RMC in postnatal care, and effective communication and informed choice.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Aug 12, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in