Integrating Oral Pathology into Diagnostic Practice: A Clinical Imperative for Head and Neck Pathology
Published in General & Internal Medicine
In today’s era of precision diagnostics, the value of interdisciplinary collaboration has become increasingly evident, particularly in the field of diagnostic pathology. While general pathologists play a pivotal role in identifying and interpreting a wide spectrum of diseases, there exists a specialised domain that requires a more nuanced understanding: oral and maxillofacial pathology. This branch of pathology is dedicated to the diagnosis of diseases affecting the oral cavity, jaws, salivary glands, and associated head and neck structures. Oral and maxillofacial pathologists are specifically trained to handle the histological complexities of these regions, bridging crucial knowledge gaps that may otherwise be overlooked.
Across diagnostic settings, many general pathologists have come to recognise oral and maxillofacial pathology as a distinct and important speciality. There is growing acknowledgement that oral lesions whether odontogenic tumours, salivary gland neoplasms, or epithelial dysplasias require the focused attention of someone with domain-specific training. Yet, despite this recognition, complex head and neck biopsies are not routinely referred to oral pathologists. In many cases, this is not due to disregard but rather a lack of structural integration, dedicated hiring, and systemic awareness of oral pathology's critical diagnostic value.
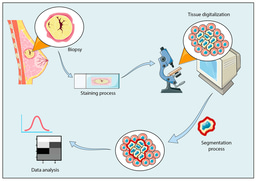
The head and neck region presents a wide array of challenging pathological entities. These include odontogenic cysts and tumours, jawbone lesions, mucosal premalignant changes, and a diverse group of salivary gland neoplasms. These lesions are not only histologically diverse but also clinically complex, requiring in-depth contextual understanding such as radiographic correlation, knowledge of dental and craniofacial development, and insight into site-specific behaviour. In such settings, oral and maxillofacial pathologists are uniquely qualified to make precise diagnoses that significantly impact surgical planning, cancer management, and long-term patient outcomes.
Despite these advantages, oral and maxillofacial pathology is still often regarded as a purely academic or dental sub-discipline in many institutions. It is commonly housed within basic medical sciences and is rarely integrated into frontline clinical or diagnostic services. Many histopathology laboratories process biopsies from the head and neck region on a regular basis without input from a trained oral and maxillofacial pathologist. This disconnect is concerning, especially given the rising burden of oral cancer, increasing recognition of premalignant and reactive lesions, and the growing importance of morphomolecular diagnostic approaches. Relying solely on general pathologists for complex oral lesions without access to subspecialty consultation risks misdiagnosis, delays, and potential compromises in patient care.
To address these challenges, institutional protocols should be developed to guide the referral of complex or ambiguous head and neck cases to oral pathologists. This approach would mirror existing best practices, such as referring soft tissue tumours or lymphomas to their respective subspecialists. Such collaboration not only promotes diagnostic accuracy but also enriches interdisciplinary education and strengthens patient outcomes. Furthermore, oral pathologists should be actively involved in multidisciplinary tumour boards, clinical case discussions, and continuing medical education (CME) activities to ensure their expertise informs patient-centred decision-making.
Unfortunately, in Pakistan, oral and maxillofacial pathology is still often regarded as a purely academic or dental sub-discipline. To bridge this gap, urgent reforms are needed. First, regulatory authorities such as the Pakistan Medical and Dental Council (PMDC), College of Physicians and Surgeons Pakistan (CPSP), and Higher Education Commission (HEC) must officially recognise oral pathology as a clinical diagnostic speciality. This step will validate its importance and ensure its rightful place within healthcare delivery. Second, every tertiary-care hospital and diagnostic centre dealing with head and neck cases should be required to either hire a qualified oral pathologist or engage one in a consultative role. In institutions with a significant head and neck caseload, dedicated oral and maxillofacial pathology units should be established, ideally equipped with morphomolecular tools such as immunohistochemistry and PCR-based diagnostics.
In conclusion, the integration of oral and maxillofacial pathologists into mainstream pathology is not merely an academic aspiration; it is a clinical imperative. With the increasing complexity of head and neck lesions and the demand for precise diagnosis, Pakistan can no longer afford to marginalise this speciality. Oral and maxillofacial pathology must be redefined as a clinical, diagnostic discipline with a tangible impact on patient care. Establishing oral pathology services in laboratories and formally hiring oral pathologists nationwide will not only elevate diagnostic standards but also align our healthcare system with global best practices.

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in