Mapping the brain's highways and byways to explore the potential of intranasal oxytocin in psychosis prevention
Published in Neuroscience, Protocols & Methods, and General & Internal Medicine

Psychosis is a complex condition which casts a shadow over the mental and physical health of many lives, and researchers and clinicians are continuously exploring new avenues for prevention and support. In our latest Molecular Psychiatry study entitled “Connectome dysfunction in patients at clinical high risk for psychosis and modulation by oxytocin”, we explore the merits of intranasal oxytocin as a potential candidate in psychosis prevention. We do this by testing whether, a “sniff” of this peptide administered to people at risk can modulate an important mechanism thought to contribute to the genesis of psychosis and result in alterations in the organisation of brain connections.
Understanding psychosis risk and Psychiatry’s shift towards prevention
Traditionally, psychiatry has primarily focused on symptom management and treatment post-onset. However, there is a growing recognition of the importance of early intervention and prevention in mental health. Before the onset of psychosis, individuals may experience a phase known as Clinical High Risk for Psychosis (CHR-P), marked by subtle changes in perception and cognition. Strategies for early intervention during this phase would be crucial for mitigating the risk of psychosis onset. From cognitive-behavioral therapy to novel pharmacological agents, researchers are actively investigating diverse approaches but identifying a highly effective one remains a distant target to achieve. In this context, understanding the underlying brain mechanisms of psychosis risk is critical for developing tailored interventions that might promote resilience at the time when the disorder first starts.
The role of the brain's highways and byways in psychosis
At the core of psychosis risk lies the intricate network of connections within the brain. These connections, or neural pathways, facilitate communication between different brain regions and underpin various cognitive and emotional processes, which if disrupted might can contribute to the development of psychosis and other mental health disorders. Connectomics, the study of brain connectivity patterns, has emerged as a powerful tool for identifying and understanding how irregular patterns of brain connections might predispose individuals to psychosis and other psychiatric conditions. An intervention that modulates these irregular patterns of brain connections might therefore stand out as an interesting candidate for psychosis prevention.
Intranasal Oxytocin… A Promising Avenue
Intranasal oxytocin, recognized for its role in social bonding and emotional regulation, has garnered attention as a potential intervention in preventive psychiatry mostly for its capacity to modulate multiple processes contributing to mental distress, i.e. by decreasing stress and anxiety or facilitating our understanding of others actions and thoughts. Recent research suggests that one of the mechanisms oxytocin uses to do so is by influencing brain connections. Could boosting the levels of oxytocin in the brain through a nasal spray offer a promising avenue for early intervention strategies in psychosis?
Our Study
In our study, we investigated the effects of a single acute dose of intranasal oxytocin on the functional connectome in 30 clinical high-risk individuals using advanced statistical methods applied to data acquired with a neuroimaging technique called magnetic resonance imaging, MRI. We found significant differences in network organisation between individuals prone to psychosis and healthy controls, particularly within key brain networks implicated in psychosis such as the thalamus or the nucleus accumbens. Moreover, we observed that oxytocin modulated network topology in a manner specific to clinical status, making the brain connections of individuals at risk for psychosis change in a direction so they were more like those observed in healthy individuals.
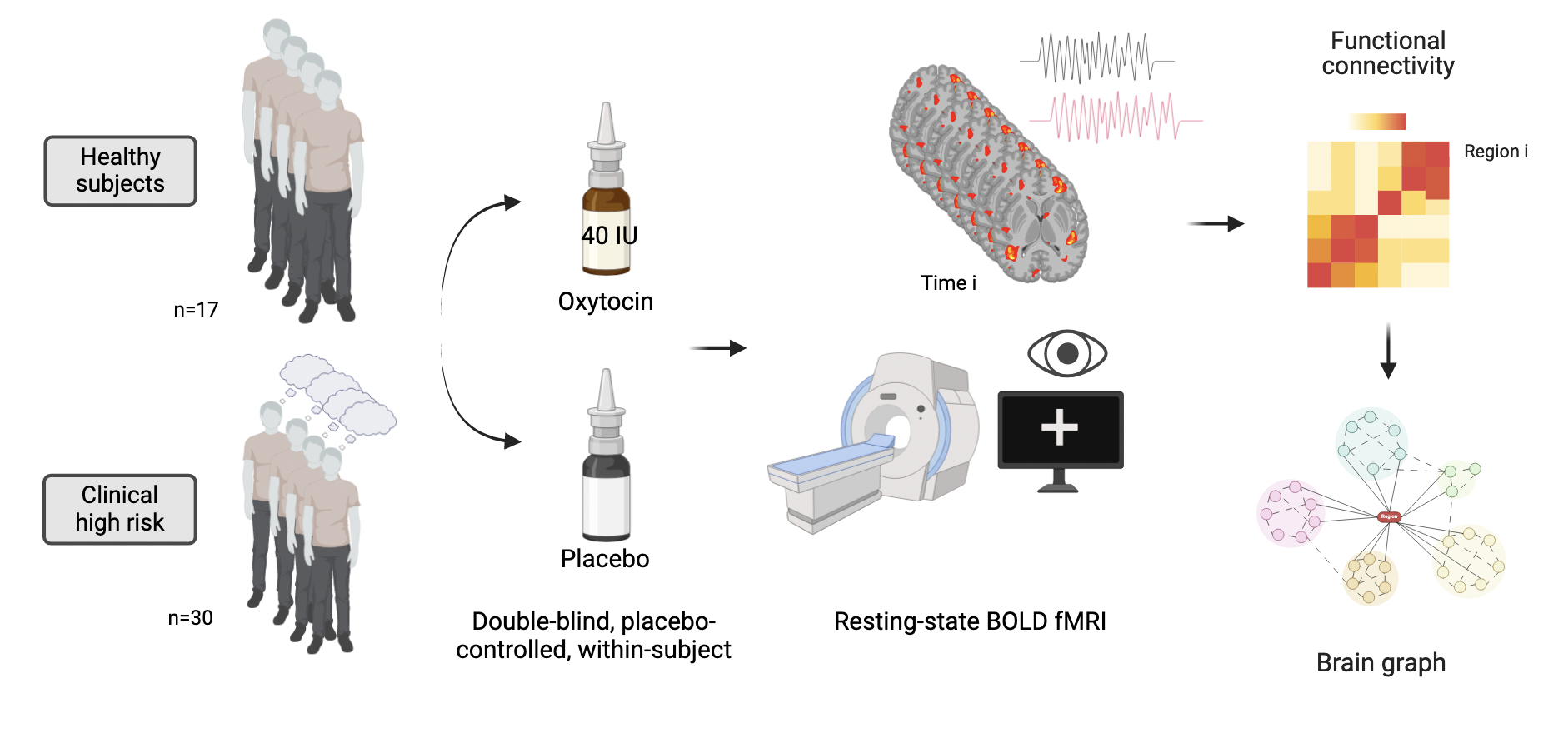
Figure 1: Summary of our study's design and analytical approach
Insights and limitations
While our findings are preliminary, they contribute important pieces of information about the potential utility of intranasal oxytocin in psychosis risk and identify a plausible mechanism underlying such effects and an imaging technique that can be used to study it further. However, our findings will need to be replicated in larger samples and further work identifying optimal doses and methods of administration in this population should be conducted.
As preventive psychiatry continues to gain momentum, intranasal oxytocin emerges as a promising tool in our selection of early intervention strategies for psychosis. One small beacon of hope illuminating the path towards prevention and support for all individuals.
Follow the Topic
-
Molecular Psychiatry

This journal publishes work aimed at elucidating biological mechanisms underlying psychiatric disorders and their treatment, with emphasis on studies at the interface of pre-clinical and clinical research.



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in