Mapping the Neurodevelopmental Predictors of Psychopathology
Published in Neuroscience, General & Internal Medicine, and Behavioural Sciences & Psychology
Explore the Research
Mapping the neurodevelopmental predictors of psychopathology - Molecular Psychiatry
Molecular Psychiatry - Mapping the neurodevelopmental predictors of psychopathology
The neurodevelopmental origins of mental illness have become increasingly acknowledged, such that most forms of psychopathology are becoming recognized as brain disorders rather than mental issues stemming from maladaptive thoughts and feelings. This conceptualization has garnered widespread adoption and permeated the way we describe mental health challenges in our everyday vocabulary. For instance, symptoms of depression tend to be attributed to deficiencies in mood-regulating neurotransmitters, such as serotonin and dopamine. This way of thinking has been rightfully supported by advancements in psychotropic medications and decades of research that have uncovered a multitude of neuroimaging differences associated with psychopathology. It is increasingly clear that individuals suffering from mental illness tend to exhibit atypical neurobiological characteristics related to brain structure, functional organization, and white matter connections. Although many facets of the brain are impacted by mental illness, an overwhelming amount of evidence suggests that there is not a single mechanism that can be used to deterministically predict the onset of symptoms or track how mental disorders progress throughout the lifespan. The most clinically relevant neuroimaging markers tend to be only weakly correlated with mental health outcomes.
Machine learning algorithms are useful tools for summarizing heterogeneous neuroimaging data into single mental health estimates, which are generated on person-by-person basis (Figure 1). In theory, combining the predictive power of all clinically relevant neuroimaging features should result in highly accurate brain-based models of psychopathology. However, capturing all the intricate brain-behavior relationships in a single predictive algorithm remains a critical challenge. This is an important objective as developing accurate predictive algorithms could help uncover key biomarkers and be clinically useful in the early identification of high-risk individuals. Towards this end, we leveraged a machine learning framework to understand which neuroimaging metrics and brain networks were the most important in the prediction of internalizing symptoms, externalizing symptoms, and general psychopathology.
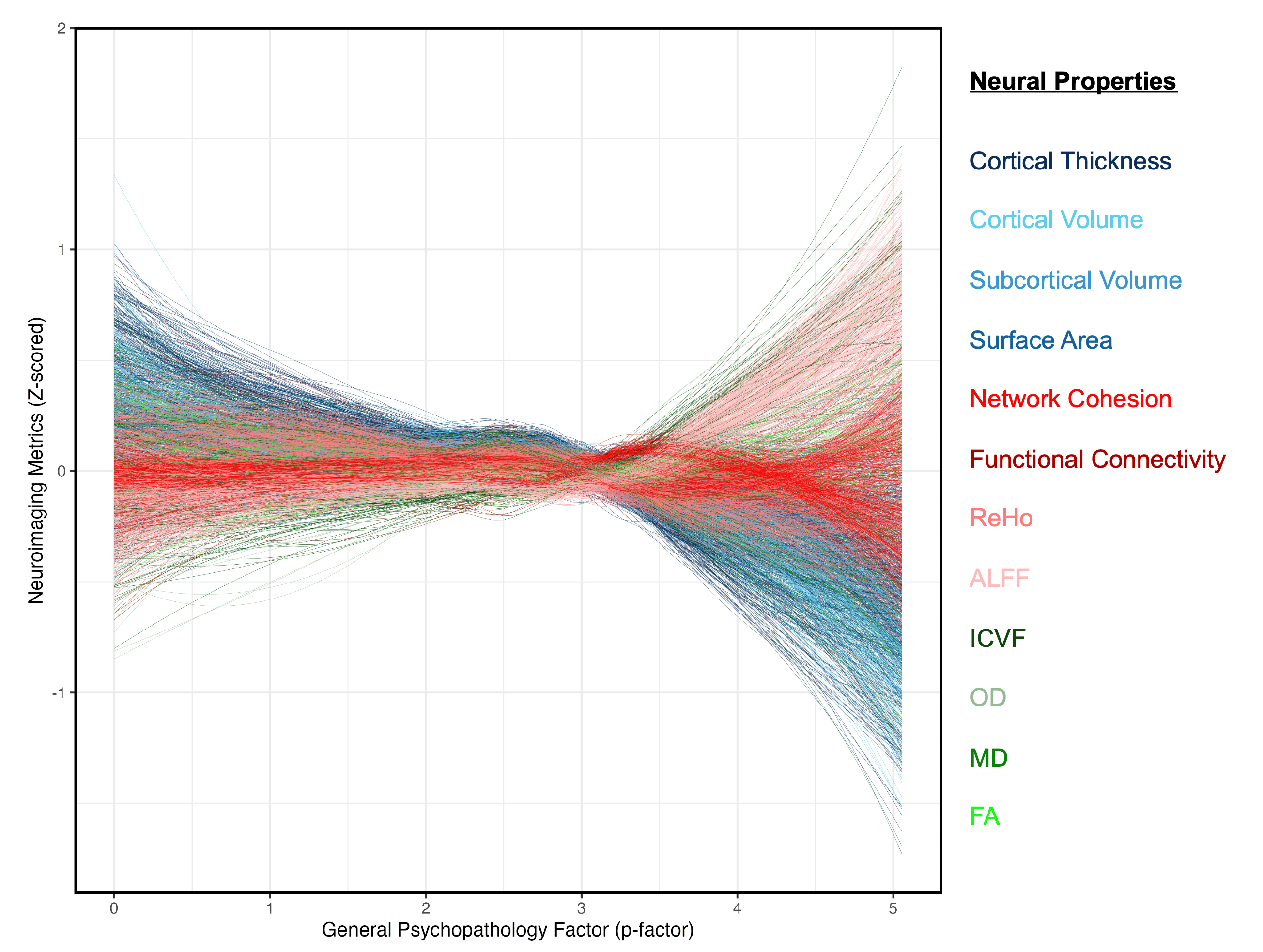
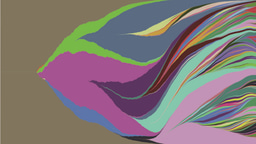
Figure 1. Multimodal neuroimaging features exhibit unique and diverse associations with psychopathology. Each set of neuroimaging metrics displayed similar non-linear patterns with general psychopathology, but greater differences were apparent between MRI modalities. Each colored line represents a single neuroimaging feature, which is color coded based on its given neuroimaging modality. Blue colored lines represent metrics of anatomical brain structure, red lines denote metrics of brain activation and functional connectivity, and green lines contain information about the microstructure of white matter tracts. All features were plotted using a locally weighted scatterplot smoother (loess), which is a nonlinear parametric technique used to fit a smooth curve to a given set of data points.
Most Predictive Neurobiological Properties
We found that metrics of white matter microstructure were consistently the best predictors of psychopathology (Figure 2), particularly those calculated using neurite orientation dispersion and density imaging (NODDI). Prior research has delineated that these microstructural characteristics were the most sensitive to neurodevelopmental differences and generalized cognition. Considering that these white matter properties made up only a small proportion of our feature space, it is even more likely that these features contained unique and pertinent neurobiological information about psychopathology. In particular, the most important white matter connections were found along the anterior thalamic radiation, which serves an important role in the corticostriatal circuit, as these nerve fibers connect the prefrontal cortex with deep brain structures, such as the striatum and thalamus. Disruptions to the anterior thalamic radiation have been associated with reductions in goal-directed behaviors and psychosis-related symptoms, providing further evidence that this white matter tract may be a key mechanism underlying generalized psychopathology.
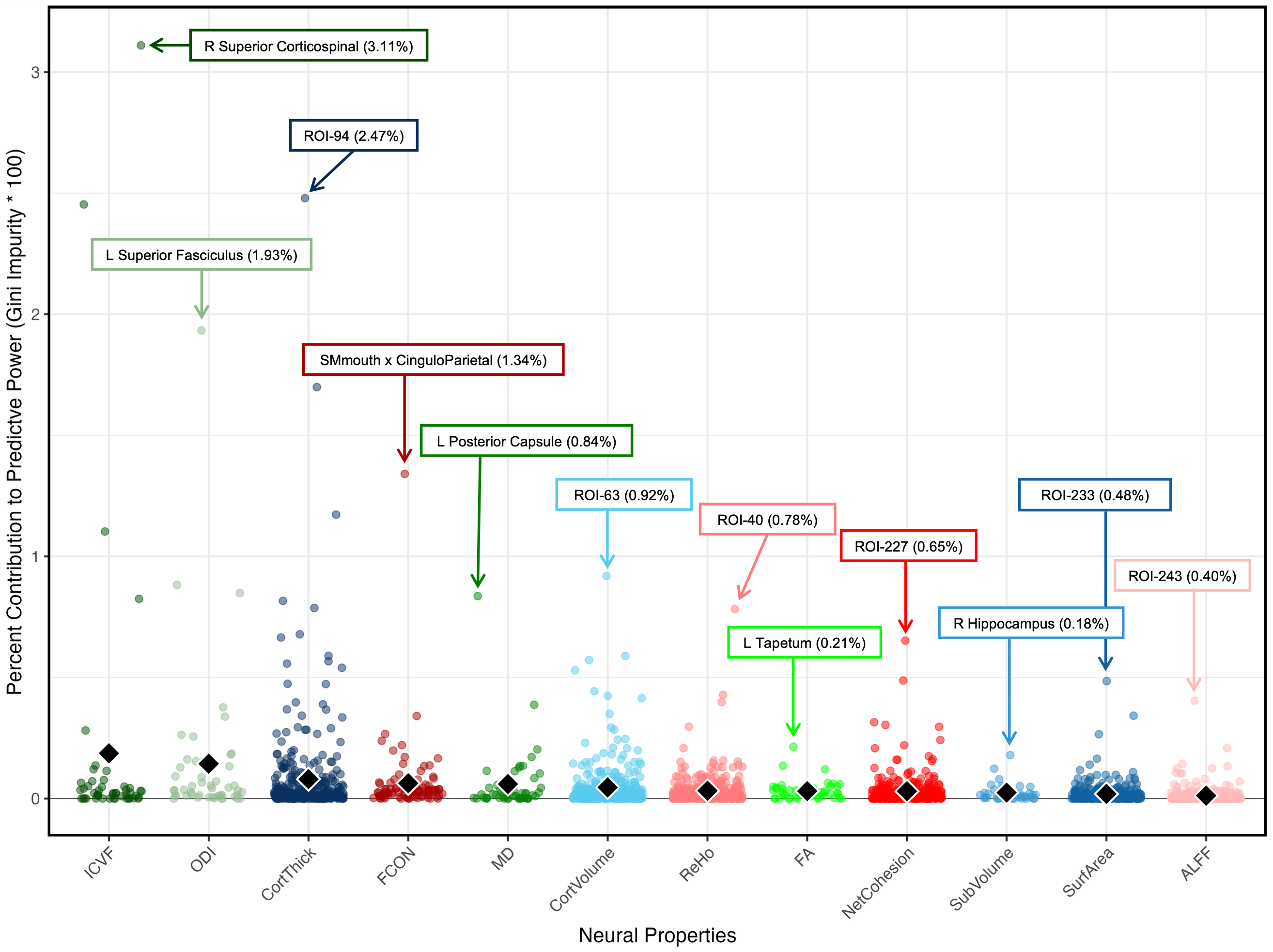
Figure 2. NODDI microstructural metrics and cortical thickness were the most heavily weighted among our models that were trained across all multimodal metrics. Gini impurities were evaluated to determine which neuroimaging metrics provided the largest predictive power to our multimodal models. Intra-cellular volume fraction (ICVF), orientation dispersion index (ODI), and cortical thickness demonstrated the largest importance, as these properties contained the five most important features and the highest impurity values when averaging across all brain regions. Each colored dot in the scatter plot reflects the mean impurity value of a single feature that was used to optimize our multimodal models. Text boxes were used to identify the most important feature among each neural property. The black diamonds denote the mean impurity values across all features for a given set of neural properties, which are sorted from the greatest to the least important along the X-axis.
Most Predictive Brain Networks
Our results also demonstrated that models trained exclusively on features from the default mode and dorsal attention networks were the most accurate, even when compared to the models that were trained across all brain networks (Figure 3). These findings further demonstrate that it may be essential to optimize machine learning algorithms using a subset of clinically relevant biomarkers rather than using a large quantity of non-informative metrics. These results build upon prior literature suggesting that abnormal connectivity between these networks might be the neurological basis for depressive rumination, as affected individuals are unable to disengage from obsessive thoughts and feelings during the pursuit of goal-directed tasks or cognitively strenuous activities. As such, these findings are consistent with the idea that disruptions to introspection, self-reflection, and executive functioning may be principal components of general psychopathology. Nevertheless, affective brain networks that help to facilitate socioemotional regulation also emerged as playing a key role in predicting certain dimensions of psychopathology. In particular, internalizing symptoms were best predicted by features from the cingulo-opercular network, whereas the salience and cingulo-parietal networks were among the most important for externalizing symptoms. Overall, brain-based models appear to incorporate multiple complex brain-behavior dynamics in their predictions of psychopathology
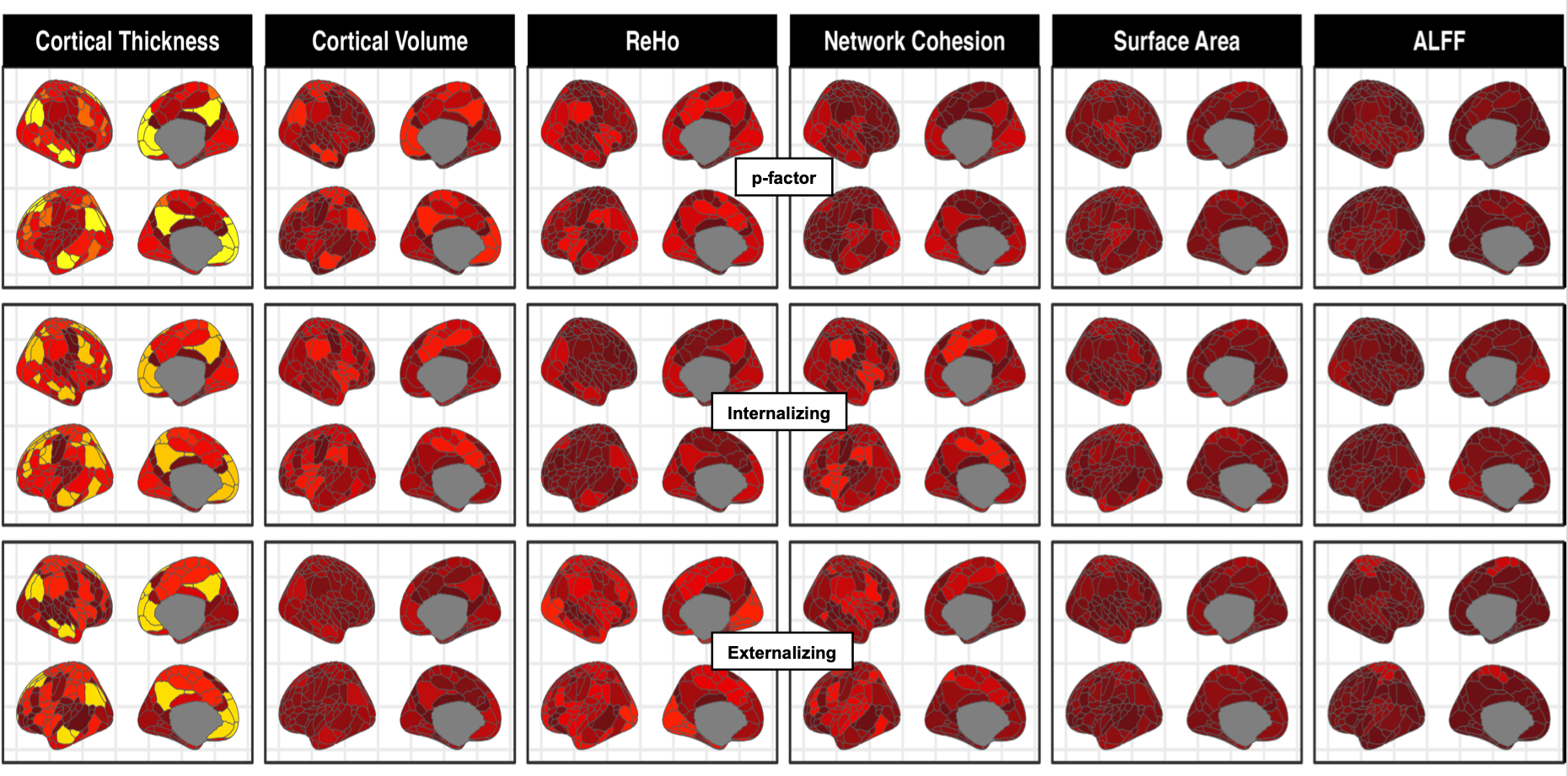
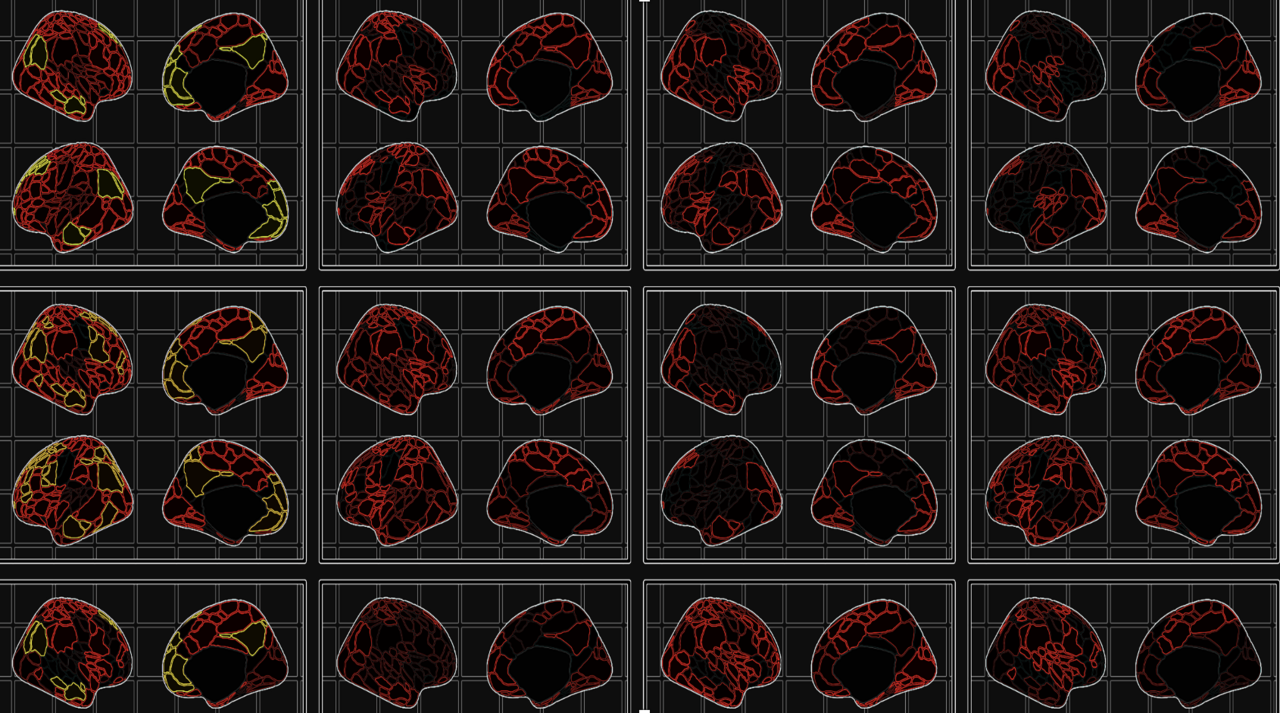
Figure 3. Neuroimaging metrics extracted from the default-model network were among the most predictive of internalizing, externalizing, and the general psychopathology. Spatial maps were used to visualize where the most important features were extracted from for each dimension of psychopathology. Lighter colors are assigned to features with higher Gini impurities on average (more predictive power), whereas darker shares of red denote features with lower Gini impurities on average (less predictive power). The default mode network and dorsal attention were consistently among the most important brain networks across all three dimensions of psychopathology. Externalizing symptoms appeared to have the most unique neural signature, as its’ models weighed features from the cingulo-parietal and salience network most heavily, as opposed to the default mode and dorsal attention network.
Prediction Accuracy of Brain-Based Models
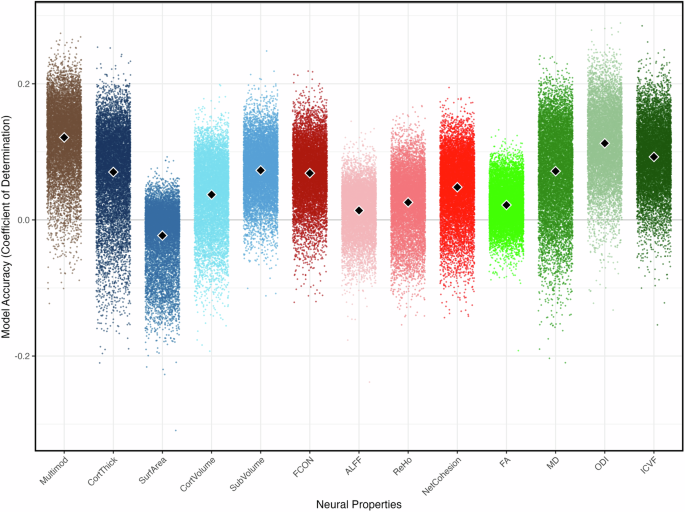
All of our brain-based models of psychopathology performed significantly better than chance but displayed relative low prediction accuracy (r2 < 0.12; Figure 4). However, our algorithms achieved greater predictive accuracy than those from prior prediction-based studies conducted on adolescent samples (r2 < 0.03). While our study is a step in the right direction, many improvements are necessary. Studies conducted on adult populations have been relatively more successful in using neuroimaging data to derive accurate machine learning algorithms, especially when detecting differences in schizophrenia, bipolar disorder, and major depression. Given the progressive nature of these disorders and their widespread impact on the brain, it is not surprising that these studies reported better predictive accuracy at later stages of life when neural differences associated with psychopathology are most apparent. Yet, it is not as clear when, in development, the neurobiological differences related to psychopathology are prominent enough, such that we can begin deriving more accurate brain-based models of psychopathology. Further, it is less certain whether such models derived in later stages of development would have clinical utility as a way of identifying high-risk individuals. Thus, there remains a strong need to establish accurate predictive models during adolescence when symptoms of psychopathology are most likely to emerge, and the implications for data-driven diagnostic tools would be the most valuable.
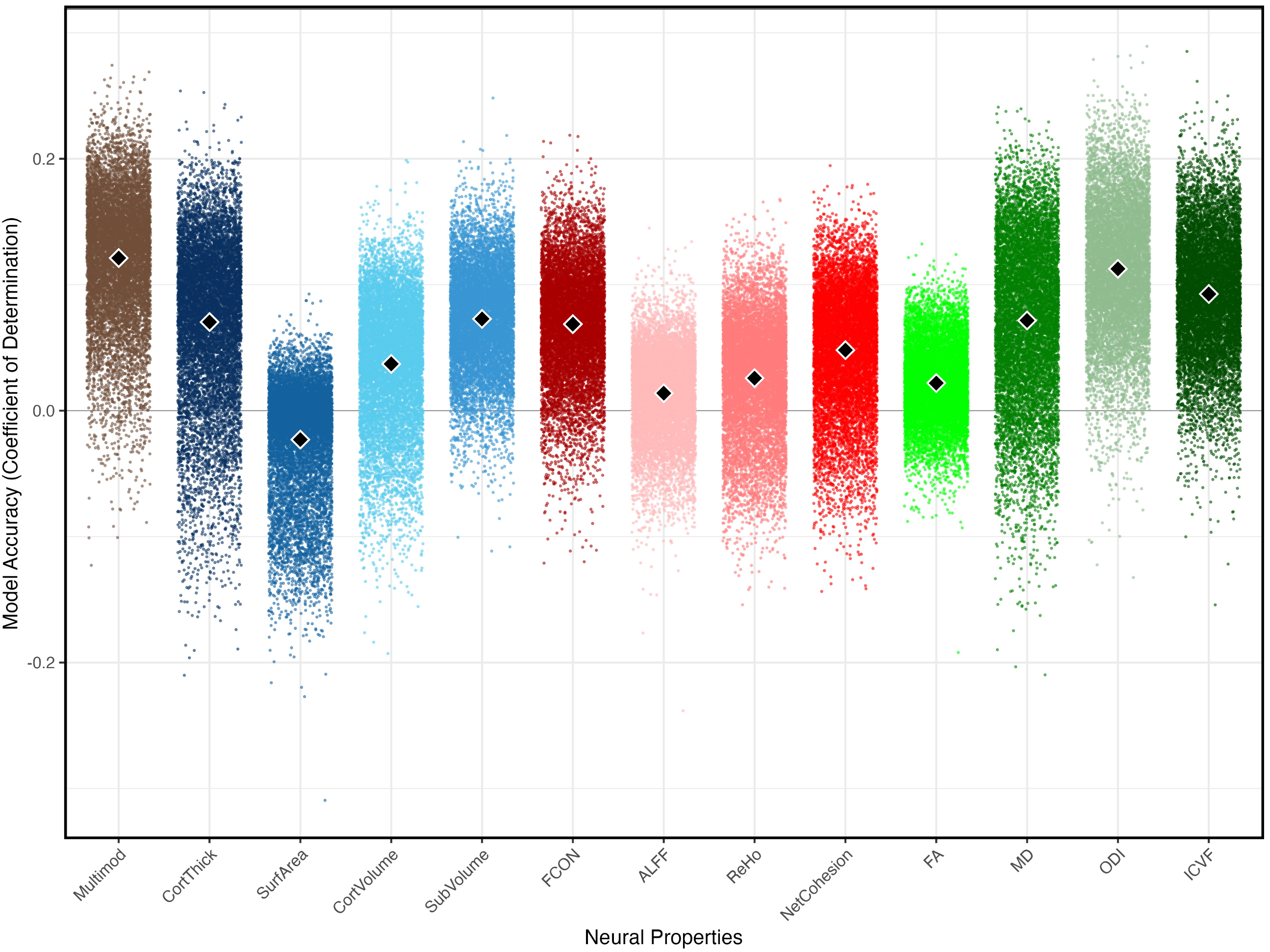
Figure 4. Brain-based models of psychopathology were the most accurate when optimized across all neuroimaging features, but many improvements are necessary for such predictive models to be clinically relevant. Among the models that were trained exclusively on a single set of neuroimaging metrics, the greatest accuracy was achieved when using ODI, ICVF, or cortical thickness. Each colored dot in the scatter plot represents the coefficient of determination from one of our bootstrapping iterations, and the black diamonds denote the mean coefficient of determination across all 10,000 bootstrapped samples. Abbreviations on the X-axis: functional connectivity (FCON); amplitude of low frequency fluctuations (ALFF); regional homogeneity (ReHo); fractional anisotropy (FA); mean diffusivity (MD); orientation dispersion indices (ODI); intracellular volume fractions (ICVF).
Conclusion and Future Directions
Multimodal neuroimaging has provided us valuable insights into the neurobiological markers underlying various forms of psychopathology, but additional work is needed to derive accurate prediction-based algorithms that would be applicable in a clinical setting. Taken with findings from prior studies, neurobiological features appear to be an important part of the equation for predicting psychopathology, but relying exclusively on neural markers is clearly not sufficient. This is especially true among adolescent samples with subclinical symptoms. Consequently, risk factor models of psychopathology may benefit from incorporating additional sources of information that have also been shown to be clinically relevant, such as demographic factors, psychosocial vulnerabilities, environmental stressors, and genetic predispositions.
Follow the Topic
-
Molecular Psychiatry

This journal publishes work aimed at elucidating biological mechanisms underlying psychiatric disorders and their treatment, with emphasis on studies at the interface of pre-clinical and clinical research.
Your space to connect: The Psychedelics Hub
A new Communities’ space to connect, collaborate, and explore research on Psychotherapy, Clinical Psychology, and Neuroscience!
Continue reading announcement


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in