Persistent and long-term COVID-19 symptoms – a nationwide study in Denmark
Published in Healthcare & Nursing
One year after the beginning of the SARS-CoV-2 pandemic, repeated reports of COVID-19 patients, who had not even been hospitalized, but still continued to experience a diverse range of symptoms1 made us worried.
In order to uncover the range and magnitude of these health problems in the general population, including among those who had not yet sought medical attention, we decided to attempt to collect self-reported symptom data from the Danish population. The Danish Ministry of Health supported the idea of launching a nationwide surveillance project and stepped in to fund the project.
Mass testing of the population was a central part of the control strategy in Denmark during the first part of the pandemic. PCR (polymerase chain reaction) tests were available free of charge for anybody, who wanted to be tested independent of whether they e.g. had symptoms, were contacts to infected individuals, needed to be tested for work or wanted to get tested before a social gathering. Tests could be booked online at test centres across the country and all results were registered centrally. This approach resulted in one of the highest test incidences in Europe during the period were our study was conducted2.
Together with the existence of an electronic postal system in Denmark, “e-boks”, which offers two-way communication between public authorities and among citizens aged 15-years or above3, access to nationwide PCR results enabled us to distribute electronic questionnaires to everybody, who had received a positive PCR test result for the first time within the study period. In order to measure symptoms specific for the SARS-CoV-2 infections, we also invited persons not testing positive to answer the questionnaire. For this we used date-matched control persons, who had also been PCR tested but had received a negative test result and never been tested positive.
Participation in the project was voluntary and no rewards were given for participation, and since many other smaller questionnaire-based covid-related studies had already been launched, we were curious to see whether “questionnaire fatigue” might be an issue among the invited participants. Luckily approximately 1/3 of the invited decided to participate, which is comparable to what have been observed in other studies.
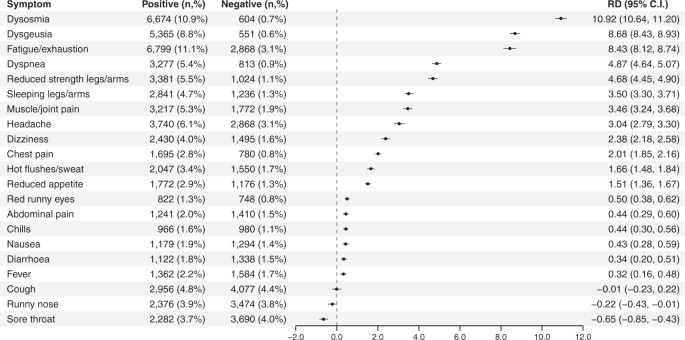
We observed that six to twelve months after the test, the risks of 18 out of 21 physical symptoms were elevated among test-positives and one third (29.6%) of the test-positives experienced at least one physical post-acute symptom compared to 13.0% among the test negative control-persons. The largest risk differences (RD), were observed for reduced/altered smell (dysosmia) (RD = 10.92%, 95%CI 10.68-11.21%) and reduced/altered taste (dysgeusia) (RD=8.68%, 95%CI 8.43-8.93%), which were the only reported symptoms that were not more prevalent among hospitalized cases compared to among non-hopsitalized cases.
Ranged after risk differences, altered sense of smell and taste were followed by fatigue/exhaustion (RD=8.43%, 95%CI 8.14-8.74%), difficulty breathing (dyspnea) (RD=4.87%, 95%CI 4.65-5.09%) and reduced strength in arms/legs (RD=4.68%, 95%CI 4.45-4.89%).
During the period from the test and until completing the questionnaire, new diagnoses of anxiety or depression were also more common among test-positives, along with general health problems, such as cognitive problems and exhaustion. Due to a possible general pandemic effects on mental health this is especially where the control group really showed its worth by allowing us to subtract the background level in the population.
We also observed influence of age and sex, where females and particularly 30-59 year olds were more likely to report most symptoms.
Based on these results, we could conclude that even in the general population in Denmark, where the majority of test-positives (96.0%) were not hospitalized during acute infection, a considerable proportion experienced post-acute symptoms and sequelae up to 12 months after infection. This was also clear, when comparing the amount of sick leave amount cases and controls.
These results are in line with the results of other studies4–7, however still much remains to be elucidated regarding both mental health, duration of symptoms, as well as influence of variants and vaccination and the full socioeconomic consequences of post COVID-19 condition. Additionally, there seem to be a lack of knowledge regarding possible ways of preventing or reducing the risk of developing post COVID-19 condition, once an individual has already been infected by SARS-CoV-2, probably due to the fact that the biological mechanisms behind the symptoms are not yet fully understood.
In an ongoing longitudinal study, we are collecting more specific information regarding mental health aspects, neurocognitive problems as well as fatigue and post-exertional malaise to supplement the results presented in the present study.
For the years to come we will still continue to benefit from these data and thereby hopefully aid in creating more evidence of the full health consequences of the pandemic. Thus were are very grateful for all the people, who have taken the time to participate in the survey, and who continues to fill-out follow-up questionnaires, which contributes more information on duration and development of different symptoms of post COVID-19 condition.
Read the full story here: https://rdcu.be/cR8zm
References
- Nalbandian, A. et al. Post-acute COVID-19 syndrome. Nat. Med. (2021) doi:10.1038/s41591-021-01283-z.
- European Centre for Disease Prevention and Control. Data on testing for COVID-19 by week and country. https://www.ecdc.europa.eu/en/publications-data/covid-19-testing (2022).
- Digitaliseringsstyrelsen. Statistik om Digital Post. https://digst.dk/it-loesninger/digital-post/om-loesningen/tal-og-statistik-om-digital-post/ (2022).
- Bliddal, S. et al. Acute and persistent symptoms in non-hospitalized PCR-confirmed COVID-19 patients. Sci. Rep. 11, 1–11 (2021).
- Augustin, M. et al. Post-COVID syndrome in non-hospitalised patients with COVID-19: a longitudinal prospective cohort study. Lancet Reg. Heal. - Eur. 6, 1–8 (2021).
- Stavem, K., Ghanima, W., Olsen, M. K., Gilboe, H. M. & Einvik, G. Persistent symptoms 1.5-6 months after COVID-19 in non-hospitalised subjects: A population-based cohort study. Thorax 76, 405–407 (2021).
- Rauch, B. et al. COVID-19-related symptoms 6 months after the infection - Update on a prospective cohort study in Germany. Preprint at medRxiv https://doi.org/10.1101/2021.02.12.21251619 (2021).
Follow the Topic
-
Nature Communications

An open access, multidisciplinary journal dedicated to publishing high-quality research in all areas of the biological, health, physical, chemical and Earth sciences.
Related Collections
With Collections, you can get published faster and increase your visibility.
Women's Health
Publishing Model: Hybrid
Deadline: Ongoing
Advances in neurodegenerative diseases
Publishing Model: Hybrid
Deadline: Mar 24, 2026





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in