Re-examining SARS-CoV-2 vaccine targeting and dose separation in England
Published in Healthcare & Nursing
Background
Novel infectious disease can inflict vast morbidity and mortality worldwide. In response to the COVID-19 pandemic, there was a surge in research and development of pharmaceutical products to aid intervention efforts, including vaccine development. Upon a candidate vaccine proving effective in trials and receiving approval from appropriate regulatory authorities for healthcare use, emergency vaccination programmes can begin. However, there will not be enough supply or personnel to vaccinate everyone immediately. This means programme planning almost always has the following crucial question: Who should we prioritise to receive the vaccine? Effective prioritisation could save many lives.
Public health decisions often have to be made on the basis of limited data and therefore need to be as robust as possible to potential changes in scientific understanding. The UK was the first country to begin their vaccine deployment campaign in December 2020. Following recommendations from the JCVI (the Joint Committee on Vaccination and Immunisation) [1], one of the earliest decisions was to target vaccination at healthcare workers, who have high exposure to infection, and the most vulnerable groups to generate the maximal impact on severe disease.
Another question of considerable importance was whether to prioritise first or second doses. In other words, would it be preferred to provide maximal two-dose protection to a smaller number of the most vulnerable first, or to prioritise lower one-dose protection to a greater number of individuals? A decision was made in the UK to adopt a 12-week dose interval for all UK vaccines [2], allowing the first three months of the programme to be dedicated to giving as many people as possible the protection offered by one dose of the vaccine.
Now some time has passed, retrospective thoughts naturally arise. Of interest to us was what may have been the epidemiological outcomes for different vaccine dose targeting and/or dose separation choices?
How can we study the potential epidemiological implications of alternative vaccine prioritisation programmes?
To investigate the epidemiological implications of having differing vaccine prioritisation and dose separation programmes whilst rolling out the vaccine, you could conduct a clinical trial. This clinical trial would have multiple (non-mixing) groups, with each group having a different combination of vaccine prioritisation scheme and time between the first and second vaccine dose. Yet, in the face of a rapidly spreading pathogen causing substantial harm amongst the population, such actions would be highly unethical and a non-starter in terms of public health policy.
There is only one “past” for how the vaccine programme was conducted for the initial rollout of the COVID-19 vaccines. How can we explore what may have occurred if another vaccine prioritisation ordering had been used? In our research, we use mathematical models to analyse infectious disease dynamics. Models can give an estimated range of predicted possibilities, given the currently available evidence, and can be used to consider scenarios for what could have happened under a given set of alternative circumstances (termed counterfactual scenarios).
To retrospectively assess the implications of the vaccine dose separation and prioritisation decisions, in this work we used mathematical models developed and matched to epidemic data from England throughout the COVID-19 pandemic to perform simulations of counterfactual scenarios.
Model summary and our choice of scenarios
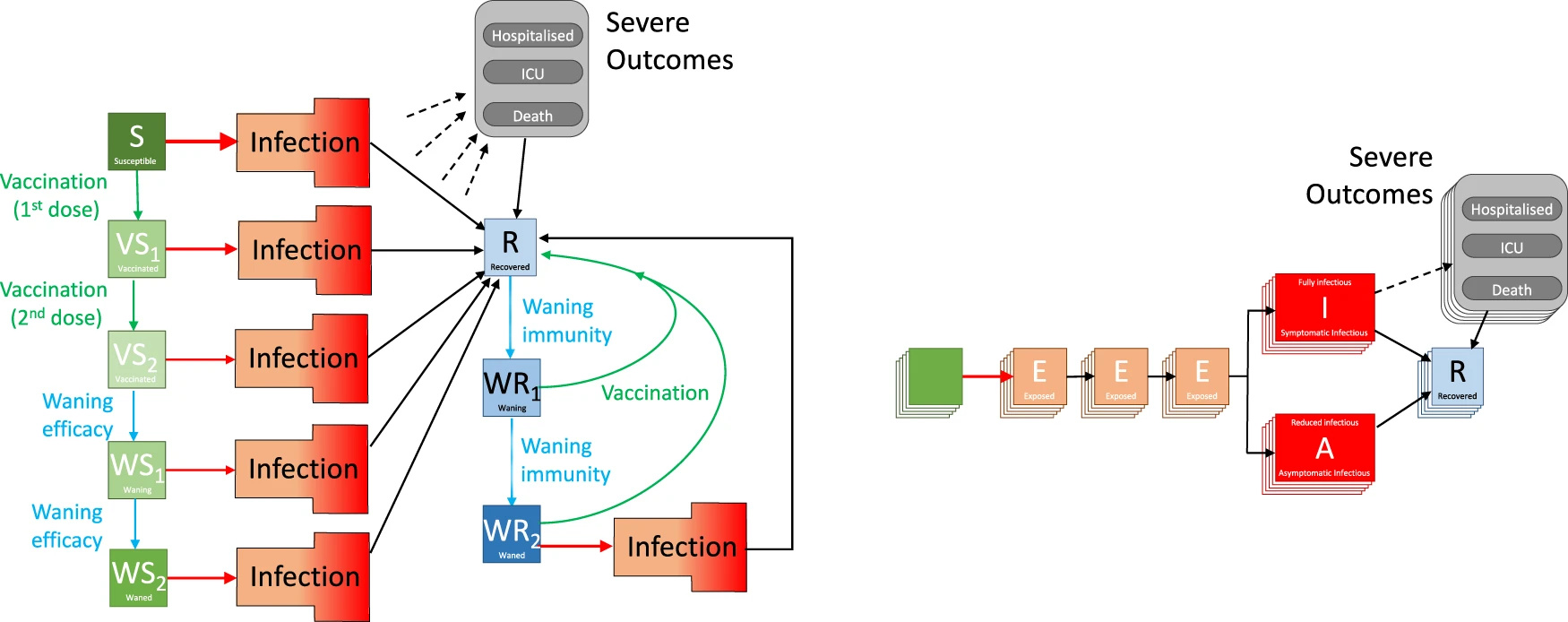
Our model is based on a traditional deterministic SEIR (Susceptible, Exposed, Infectious, Recovered) framework, with three exposed classes to capture the distribution of times from infection to becoming infectious and splitting the infectious group into symptomatic and asymptomatic infection. To this base model we added additional structure to capture the effects of restricted social interaction whilst maintaining household transmission. We stratified the population into five-year age-groups (0 − 4, 5 − 9, ... , 100+) and `replicated’ this model seven times to capture the different dynamics in the seven National Health Service (NHS) regions in England. Collectively, the model is written as a large system of ordinary differential equations [3] and is visualised in Figure 1.
Using this model, we considered four different scenarios to study a range of dose targeting and dose separation choices.
Scenario 1: Default - Model fitted to the epidemiological data (community cases, hospital admissions, hospital occupancy and deaths, from the start of the pandemic until June 2022), replaying the recorded vaccination times (corresponding to 12-week and then switching to 8-week intervals due to concerns over the Delta variant).
Scenario 2: Prioritise youngest - Vaccination order is reversed, such that the youngest adults, most responsible for transmission, are vaccinated first. The interval between the first and second vaccine dose is unchanged.
Scenario 3: Three-week interval, default efficacy - Vaccination order preserved. Second doses are given after a three-week interval, with all vaccine efficacy parameters the same as with the 12-week interval between doses.
Scenario 4: Three-week interval,lower efficacy - Vaccination order preserved. Second doses are given after a three-week interval, with a lower vaccine efficacy due to the shorter time interval between the two doses. We informed this change in vaccine efficacy from an analysis linking the level of neutralising antibodies to the degree of vaccine protection [4] and experimental work that measured the level of neutralising antibodies in individuals receiving two doses of vaccine at either a four or 12 week interval [5].
In all four scenarios, we matched the number of doses administered each day and the final attained uptake within each age-group to the observed data. Another notable assumption was it being assumed that population behaviour and all other policy decisions, such as the steps taken as part of the Roadmap out of lockdown [6], were unaffected by the scenario chosen. In reality, policy decisions were influenced by the epidemic dynamics - but prediction of this complex feedback is beyond the scope of our approach.
What did we find?
We found that the policy of vaccinating the oldest (and most vulnerable) first led to a faster decline in deaths and hospital admissions (shown in Figure 2) than targeting the younger age groups who are more responsible for transmission (comparing the default black line with the green dotted line for the alternative targeting).
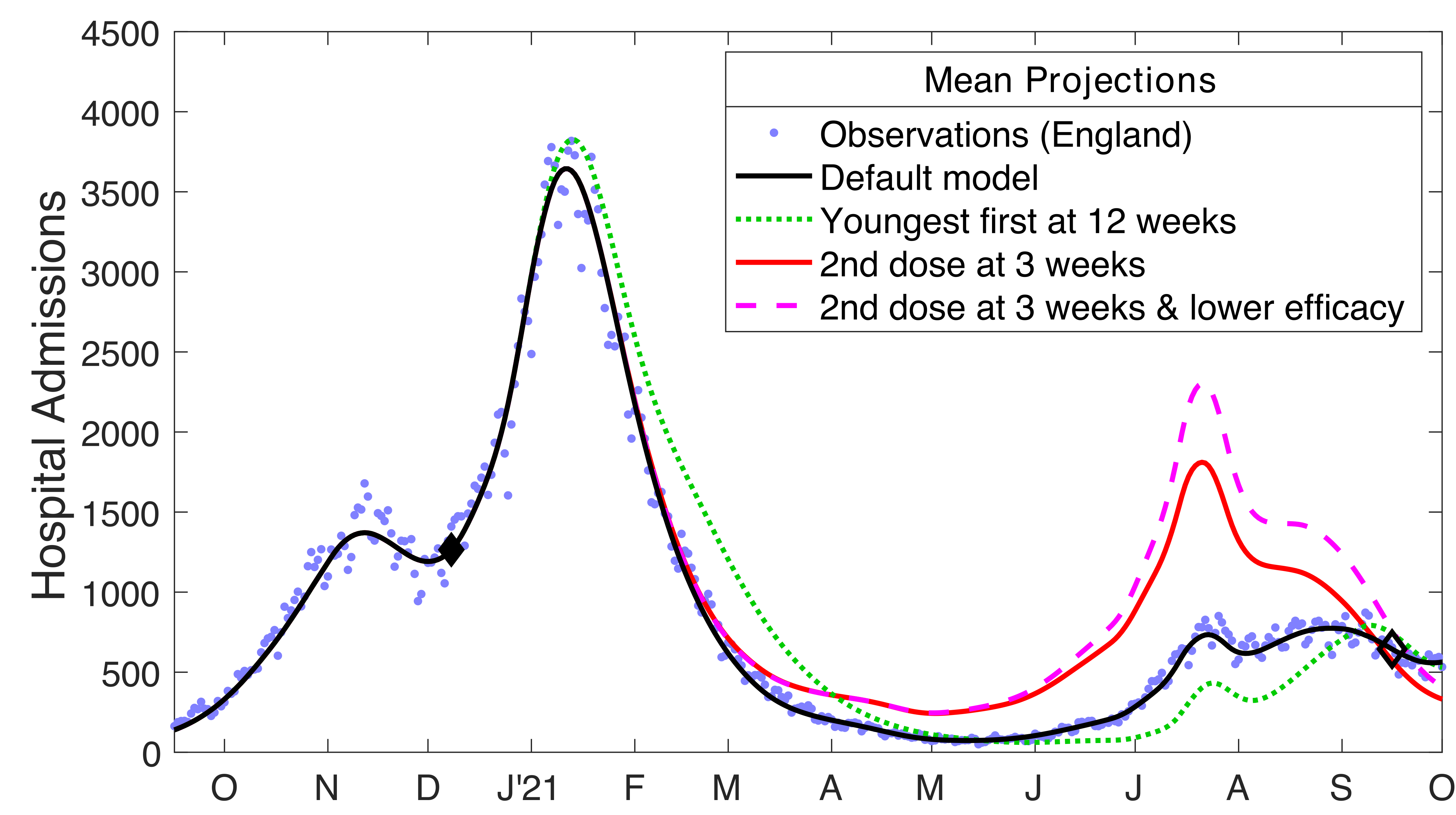
The 12-week delay was also highly beneficial, estimated to have averted between 32,000-72,000 hospital admissions and 4,000-9,000 deaths over the first ten months of the campaign (December 2020 - September 2021) depending on the assumed interaction between dose interval and efficacy (comparing the black line with the counterfactual red and pink lines).
|
Hospital admissions |
Deaths |
|
|
Observed |
243,573 |
62,163 |
|
Modelled scenarios |
||
|
(1) Default |
245,800 (243,500-247,900) |
61,200 (59,900-62,400) |
|
(2) Prioritise youngest |
261,400 (223,600-487,100) |
84,500 (71,200-163,600) |
|
(3) Three-week interval, default efficacy |
314,100 (302,800-329,300) |
69,300 (67,000-71,100) |
|
(4) Three-week interval,lower efficacy |
341,400 (322,400-368,600) |
74,900 (70,700-79,900) |
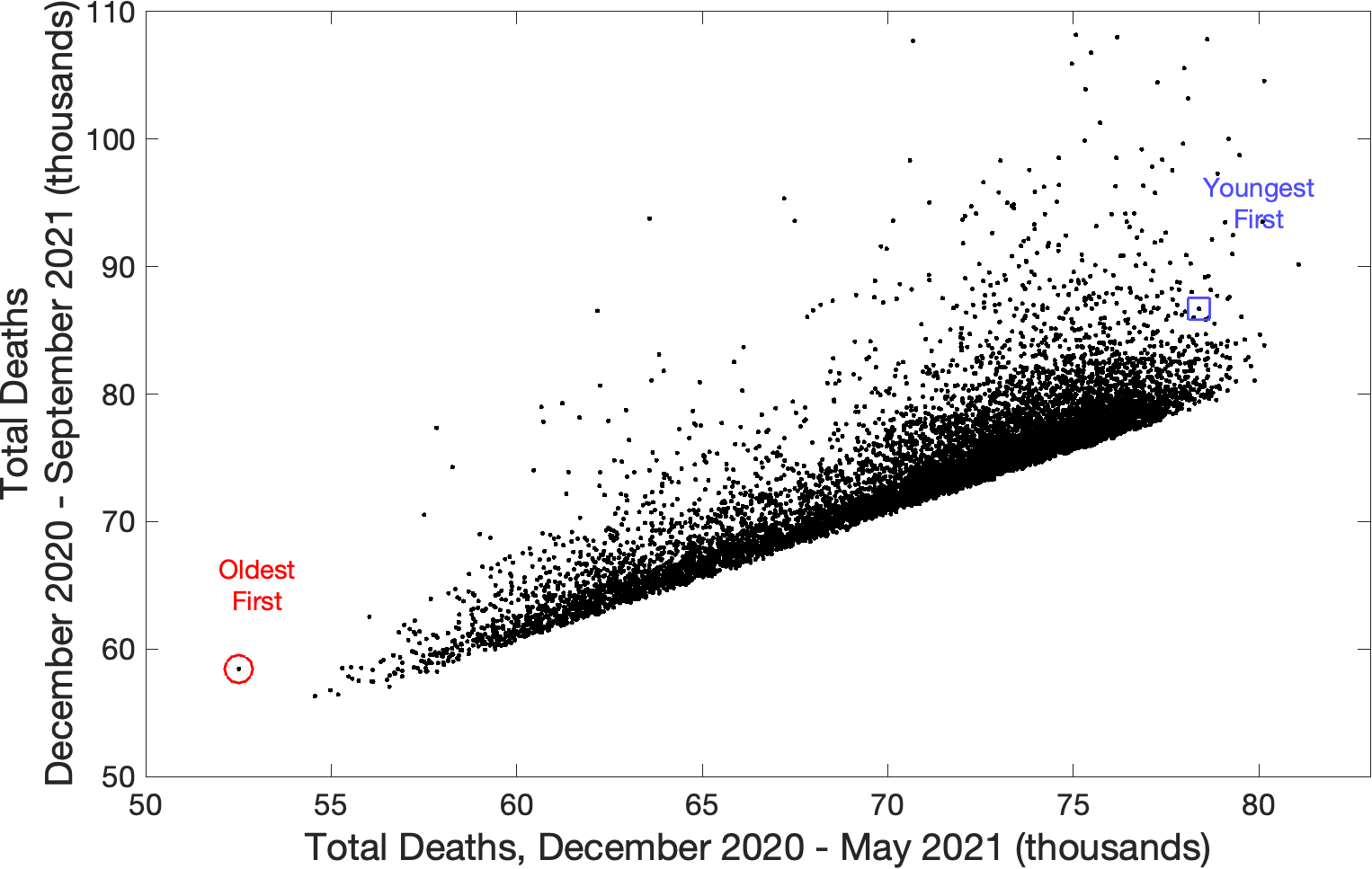
This initial analysis provoked a further question: were there other choices of age-dependent ordering of vaccination that could further reduce the projected number of severe case outcomes due to COVID-19? Through model simulations we tested a random sample of 10,000 different age-orders, whilst maintaining the number of doses delivered per day and the recorded uptake in each age-group. The strategy of vaccinating in age-order from oldest to youngest appeared one of the best-performing strategies in terms of minimising severe cases (with deaths presented in Figure 3), reinforcing the conclusions from earlier work on vaccine prioritisation [7,8].
We must recognise the importance of interpreting findings from model-based studies by considering the assumptions made and deliberating the potential implications under alternative assumptions. These reflections are required because the real world is always much more complex than can be represented in a model and unanticipated external factors may often play a role. For example, our analyses assumed that irrespective of the vaccination scenario the same behavioural changes and legal changes would occur. This is unlikely to be true as the higher number of hospital admissions and deaths observed in some scenarios would likely shift the relaxation of restrictions and lead to a greater precautionary reaction from the general public. In our models we also did not split the population by other risk factors other than age, though that is a result of the majority of epidemiological data not being stratified according to comorbidities.
Implications of our modelling study
In general, we anticipate such results to hold for future pandemics in other geographical or demographic settings whenever first doses generate substantial protection against severe disease in the most vulnerable [9] and whenever the most vulnerable are at high initial risk. Nevertheless, our ideas and understanding will always change as new information comes to light during the outbreak. To assess the benefits on a case-by-case basis, ideally bespoke models matched to available national data are ideally needed.
Overall, the advice given by the JCVI in late 2020 and early 2021, was based on very limited data about vaccine efficacy against the newly emerged Alpha variant, and with no knowledge of the forthcoming waves of infection or the waning of protection. Under such conditions, our modelling investigation suggests that a simple yet precautionary strategy performs exceedingly well from a public health perspective, rapidly providing broad protection to those individuals that need it the most.
For further details, our full paper is available at: https://doi.org/10.1038/s41467-023-35943-0
References
- Department of Health and Social Care. Joint Committee on Vaccination and Immunisation: advice on priority groups for COVID-19 vaccination, 30 December 2020. https://www.gov.uk/government/publications/priority-groups-for-coronavirus-covid-19-vaccination-advice-from-the-jcvi-30-december-2020/joint-committee-on-vaccination-and-immunisation-advice-on-priority-groups-for-covid-19-vaccination-30-december-2020 (2021).
- Joint Committee on Vaccination and Immunisation. Prioritising the first COVID-19 vaccine dose: JCVI statement. https://www.gov.uk/government/publications/prioritising-the-first-covid-19-vaccine-dose-jcvi-statement (2021).
- MJ Keeling et al. Predictions of COVID-19 dynamics in the UK: Short-term forecasting and analysis of potential exit strategies. PLOS Comput. Biol. 17, e1008619 (2021). doi: 10.1371/journal.pcbi.1008619.
- DS Khoury et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat Med 27, 1205–1211 (2021). doi: 10.1038/s41591-021-01377-8.
- RH Shaw et al. Effect of priming interval on reactogenicity, peak immunological response, and waning after homologous and heterologous COVID-19 vaccine schedules: exploratory analyses of Com-COV, a randomised control trial. Lancet Respir Med (2022). doi: 10.1016/S2213-2600(22)00163-1.
- UK Government Cabinet Office. Roadmap out of lockdown. https://www.gov.uk/government/publications/covid-19-response-spring-2021/covid-19-response-spring-2021-summary (2021).
- S Moore, EM Hill, L Dyson, MJ Tildesley & MJ Keeling. Modelling optimal vaccination strategy for SARS-CoV-2 in the UK. PLOS Comput Biol 17, e1008849 (2021). doi: 10.1371/journal.pcbi.1008849.
- S Moore, EM Hill, MJ Tildesley, L Dyson & MJ Keeling. Vaccination and non-pharmaceutical interventions for COVID-19: a mathematical modelling study. Lancet Infect. Dis. 21, 793–802 (2021). doi: 10.1016/S1473-3099(21)00143-2.
- EM Hill & MJ Keeling. Comparison between one and two dose SARS-CoV-2 vaccine prioritization for a fixed number of vaccine doses. J. R. Soc. Interface 18, 20210214 (2021). doi: 10.1098/rsif.2021.0214.
Follow the Topic
-
Nature Communications

An open access, multidisciplinary journal dedicated to publishing high-quality research in all areas of the biological, health, physical, chemical and Earth sciences.
Related Collections
With Collections, you can get published faster and increase your visibility.
Women's Health
Publishing Model: Hybrid
Deadline: Ongoing
Advances in neurodegenerative diseases
Publishing Model: Hybrid
Deadline: Mar 24, 2026

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in