Seeing Through the Patient’s Eyes: Co-designing a Video and Infographic to Transform Professional Care Relationships
Published in Healthcare & Nursing, Biomedical Research, and Public Health

What does it feel like to seek help?
This question guided our efforts to translate qualitative research into a co-designed video and infographic that helps healthcare professionals, students, and researchers reimagine what good care relationships look and feel like. The project aims to shift the way we approach relational care by utilising storytelling, metaphor, and evidence-informed design.
The research that started it
The project forms part of a program of research on relational care led by Dr Feo at Flinders University. As part of this program, in 2021, Dr Feo led a qualitative story completion study to understand how healthcare recipients and informal carers define and experience good professional caregiving relationships. Seventy-two participants (35 healthcare recipients and 37 carers) across Australia wrote fictional stories in response to a prompt about meeting a new healthcare professional. Their narratives revealed that encounters with health professionals they haven't met before often provoke emotional discomfort, even before care begins.
Participants described two primary sources of discomfort. First, concerns about their health problems. Second, concern about how the health professional might behave, often shaped by past experiences of feeling dismissed or not taken seriously.
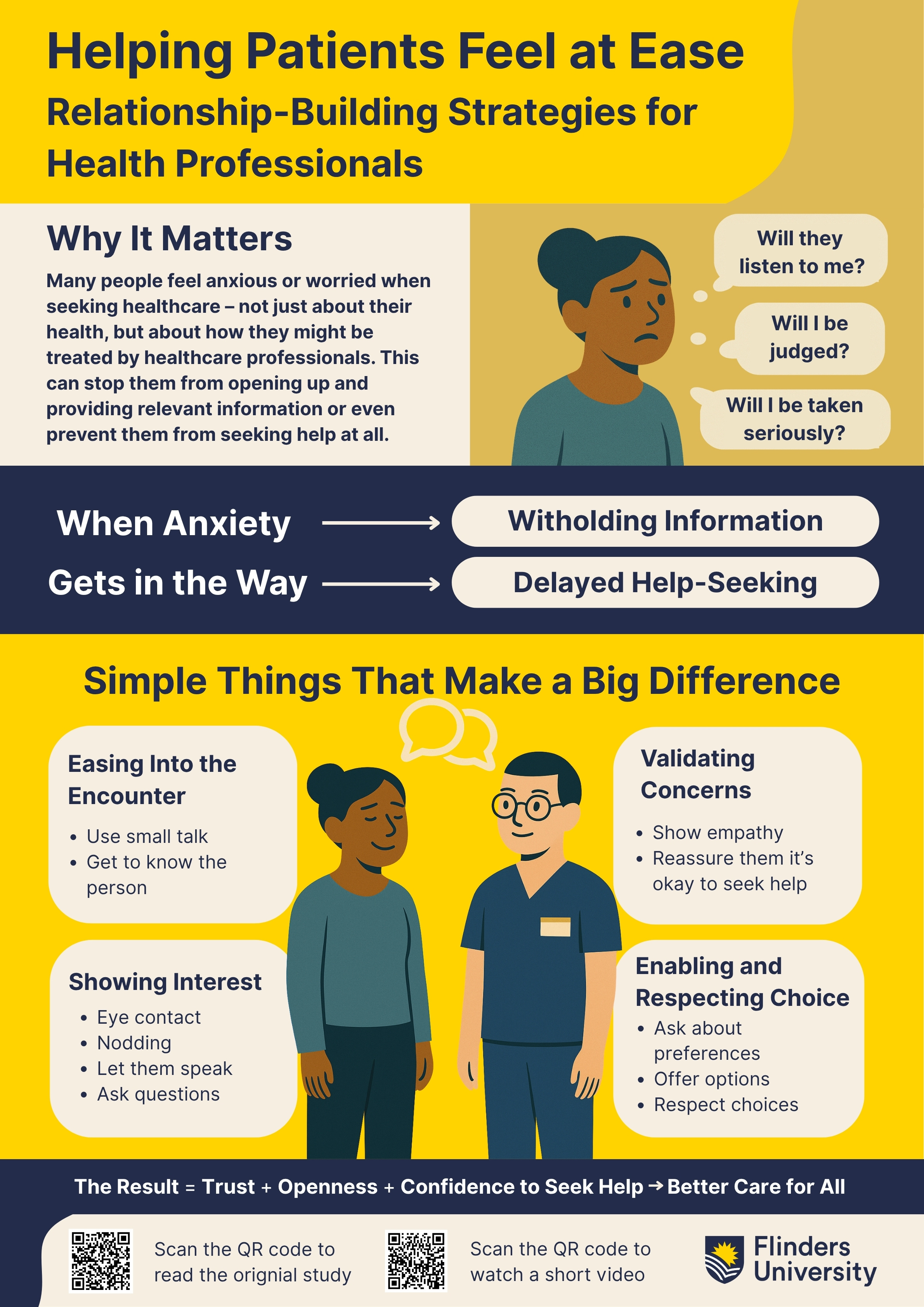
Participants consistently identified four health professional behaviours that helped reduce these anxieties:
-
Easing into the encounter (such as through small talk, introductions, and setting expectations),
-
Demonstrating interest and understanding (listening carefully, asking relevant questions, and being emotionally present),
-
Validating the presenting concern (acknowledging the legitimacy of the patient's or carer's worry),
-
Enabling and respecting choice (offering understandable explanations, presenting options, and allowing time to decide).
These behaviours contributed to feelings of safety, trust, and ease. They also made carers feel more confident in the encounter, even when their role was primarily observational. What emerged was a clear picture of relational care as something that is not just beneficial but essential.
Why a video and infographic?
Evidence alone does not shift clinical culture. To move from findings to action, we created tools that are visual, engaging, and emotionally resonant. We followed an integrated knowledge translation approach, guided by the Knowledge-activated Tools framework, and involved researchers, clinicians, and people with lived experience in every step.
Our co-design team included 13 academics and 4 co-researchers who had also participated in the original study. Together, we explored the best way to present the findings to healthcare professionals and students across various disciplines. The video concept was developed in partnership with Frankie Films, and two rounds of co-design workshops helped refine the tone, messaging, and visual elements.
The result is a short video that uses narrative and metaphor to show how everyday healthcare interactions can feel disorienting or overwhelming, and how seemingly small, thoughtful behaviours by healthcare professionals can reduce that burden. The infographic summarises the four core behaviours in a format suitable for education, workshops, and clinical environments.
What makes this project different
Several features distinguish this project. First, the method of story completion, as used in the original study, allowed participants to express ideal and imagined care experiences, going beyond what they had personally encountered. Second, the analysis identified relational behaviours that are applicable across disciplines, settings, and clinical conditions.
Third, we treated carers as central to the care relationship, not peripheral. Their emotional responses were often shaped by how the clinician treated the person they supported. When recipients felt safe and respected, carers did too.
Finally, the video and infographic were not produced after the fact. They were co-designed from the outset. Consumer and carer voices helped ensure the tools were meaningful, respectful, and relevant.
Dissemination and impact
The video and infographic have been disseminated through Flinders University’s ROADS repository, shared across internal teaching programs, and are currently being promoted through academic and clinical networks.
An evaluation plan is currently under development. Early feedback suggests that the materials encourage meaningful discussion and reflection, particularly among health students and early-career professionals. Educators are incorporating the video into communication and ethics modules, while researchers are using the infographic to support presentations focused on relational care, communication, and patient-centred practice.
To ensure that the impact of these tools can be adequately assessed, we are considering the use of a human-centred evaluation approach. This model emphasises how users engage with and apply evidence-based resources in real-world settings. Rather than relying solely on numerical indicators such as view counts or download metrics, this approach explores contextual relevance, practical usability, and sustained engagement over time. It has previously been applied in the evaluation of digital health tools, especially in projects where co-design and implementation science principles intersect with communication and knowledge translation.
By exploring this approach, we aim to strengthen the evaluative rigour of our dissemination activities and ensure that relational care resources like this video and infographic not only reach their intended audiences but are understood, used, and embedded meaningfully in practice.
Why this matters
Despite growing attention to person-centred care, relational quality remains inconsistently addressed in health systems. Emotional safety, validation, and communication are not always emphasised in training or guidelines, yet they influence whether people seek care, disclose symptoms, or engage in follow-up.
This project, and Dr Feo’s broader program of work on professional caregiving relationships, demonstrates that relational care can be effectively supported through teachable actions. These behaviours do not require more time, only more intention. They also do not belong to any one discipline. They are foundational to all forms of good care.
For example, a related initiative led by Dr Piñero de Plaza and her team (including consumer co-researchers co-leading the study), the Frail, Homebound, and Bedridden People (FHBP) project at Flinders University, similarly placed human experience at its core through socio-scientific storytelling. Promoted through the ENLIGHTEN exhibition —homEbouNd peopLe agInG witH TEchNology—the initiative integrated artistic expression, personal narratives, and policy advocacy to highlight the lived experiences and unmet needs of people with chronic illness, frailty, and disability. Using participatory research methods, engaging multimedia presentations, and extensive public outreach, the project amplified the voices of those frequently excluded from digital health innovation (#FHBP). This work was also formally submitted to the Royal Commission into Violence, Abuse, Neglect, and Exploitation of People with Disability, reaching thousands of stakeholders through open-access platforms.
A third example is the development of My Wellbeing Journal, by Dr Michael Lawless and team, a co-designed communication and goal-setting tool to support personalised care planning for older adults living with chronic conditions and multimorbidity. This tool was created through an experience-based co-design process and refined with feedback from 88 older adults and their carers across Australia. It supports meaningful goal setting and enhances the ability of clinicians and carers to engage in collaborative, person-centred discussions. The study behind the tool demonstrated how older adults' direct involvement in designing solutions helps ensure usability, relevance, and emotional resonance in real-world care planning.
Together, these three projects show that relational care is not abstract. It can be made visible, measurable, and improvable when people with lived experience are treated as co-creators of knowledge, not just recipients of care. All three underscore the same truth: to create inclusive and effective health systems, we must first listen deeply to the lived realities of those we care for, and recognise the central role of the therapeutic relationship.
References
- Feo, R., Lawless, M., Baldwin, C., Block, H., Hunter, S., Mortimer, S., Murray, J., Pinero de Plaza, M. A., Willcourt, E., Aspinall, C., Pene, B.J., Rey, S., Benson, T., Clark, C., Kelly, L., Sharples, D., & Adams, A. (2025). Video: Helping patients feel at ease - relationship-building strategies for health professionals. Flinders University. Dataset. https://doi.org/10.25451/flinders.29152025.v1
- Feo, R., Young, J., Urry, K., Lawless, M., Hunter, S.C., Kitson, A., & Conroy, T.. (2023). ‘I wasn't made to feel like a nut case after all’: A qualitative story completion study exploring healthcare recipient and carer perceptions of good professional caregiving relationships. Health Expectations, 27(1). https://doi.org/10.1111/hex.13871
- Feo, Rebecca, Pinero de Plaza, Maria Alejandra, & Lawless, Michael. (2025). Infographic: Helping patients feel at ease – relationship-building strategies for health professionals. Flinders University. Dataset. https://doi.org/10.25451/flinders.29289785.v2
- Pinero de Plaza, Maria Alejandra., Archibald, Mandy M., Lawless, Michael, Ambagtsheer, Rachel C., McMillan, Penelope, Mudd, Alexandra, Freeling, Michelle, & Kitson, Alison. (2024). A human-centered approach to measuring the impact of evidence-based online resources. Studies in Health Technology and Informatics, 310, 389–393. https://researchnow.flinders.edu.au/files/103324188/Pinero_De_Plaza_Human-Centered_P2023.pdf
- Archibald, Mandy M., Ambagtsheer, Rachel C., Lawless, Michael, Thompson, Mark O., Shultz, Timothy, Chehade, Mellick, Whiteway, Lyn, Sheppard, Anna E., Pinero de Plaza, Maria Alejandra, & Kitson, Alison. (2021). Co-designing evidence-based videos in health care: A case exemplar of developing creative knowledge translation “evidence-experience” resources. International Journal of Qualitative Methods, 20. https://doi.org/10.1177/16094069211019623
- Tieu, M, Mudd, A, Conroy, T, Pinero de Plaza, MA, & Kitson, A. (2022). The trouble with personhood and person‐centred care. Nursing Philosophy, 23(3). https://doi.org/10.1111/nup.12381
- Pinero de Plaza, Maria Alejandra. (2021). Making the Invisible Visible: Exploring the Experiences of Frail Homebound and Bedridden People. figshare. Online resource. https://doi.org/10.6084/m9.figshare.14417987.v3
- Pinero de Plaza MA., Dafny H., Lawless M., McMillan P., Buchanan R., Leon Z., Beleigoli A., Archibald M., Mudd A., Lange B., Tieu M., Feo R, Visvanathan R., Clark R., Hendriks J., Hallmann G., Del Fante P., Morton E., Hunter S., and Kitson A. (2022). ENLIGHTEN: homEbouNd peopLe agInG witH TEchNology. A socio-scientific and artistic exhibition submitted to The Royal Commission into Violence, Abuse, Neglect, and Exploitation of People with Disability (SUB.001.02754 & SUB.001.02754). Flinders University. Dataset. https://doi.org/10.25451/flinders.21569445.v2
- Lawless, Michael, Archibald, Mandy M., Ambagtsheer, Rachel C., Pinero de Plaza, Maria Alejandra, & Kitson, Alison. (2023). My Wellbeing Journal: Development of a communication and goal‐setting tool to improve care for older adults with chronic conditions and multimorbidity. Health Expectations, 27(1). https://doi.org/10.1111/hex.13890
- Pinero de Plaza MA, Gebremichael L, Brown S, Wu CJ, Clark RA, McBride K, Hines S, Pearson O, Morey K. Health System Enablers and Barriers to Continuity of Care for First Nations Peoples Living with Chronic Disease. Int J Integr Care. 2023 Dec 11;23(4):17. https://ijic.org/articles/10.5334/ijic.7643
- Pinero de Plaza, Maria Alejandra; Allande-Cussó, Regina; Conroy, Tiffany; Porcel-Gálvez, Ana Maria; Feo, Rebecca; Chipchase, Lucy; Nørby Adams, Anne Mette; Parr, Jenny; & Kitson, Alison. (2025). Piloting Structural Equation Modeling for Fundamental Care Decision-Making Across Healthcare Settings. PREPRINT (Version 1) available at Research Square. https://doi.org/10.21203/rs.3.rs-6365026/v1






Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in
This is fantastic - to have patients think beyond their experience to - express ideal and imagined care experiences.
Thank you, Nisha. I really appreciate your comment.
It was a privilege to help translate these insights into tools that support more visible and teachable relational care. The way participants imagined ideal care experiences helped shape how we approached the video and infographic.
I'm glad the piece resonated with you. :)
Agree - thank you, Nisha! Enabling participants to think beyond experience was one of my main reasons for choosing the method of story completion in the original study - whilst care experiences are undoubtedly important, unfortunately they're not always optimal. Exploring what 'could be' helps us to look beyond 'what is' and envision a new future for healthcare.