It's Stem Cell Awareness Day
Published in Cell & Molecular Biology and General & Internal Medicine
 This Q&A accompanies an Editorial published today in Stem Cell Research and Therapy entitled 'Stem cells as biological drugs for incurable diseases'. The article was written by members of our own Editorial Board in celebration of Stem Cell Awareness Day 2025.
This Q&A accompanies an Editorial published today in Stem Cell Research and Therapy entitled 'Stem cells as biological drugs for incurable diseases'. The article was written by members of our own Editorial Board in celebration of Stem Cell Awareness Day 2025.
Dr. Ichiro Sekiya serves as the Director of the Center for Stem Cell and Regenerative Medicine at the Institute of Science Tokyo. His research focuses on cartilage and meniscus regeneration using autologous synovial stem cells. Dr. Sekiya received the New Investigator Research Award from the Orthopaedic Research Society in 1998 and the Japanese Society for Regenerative Medicine Clinical Award in 2016.
1) Can you briefly explain the focus of your current research?
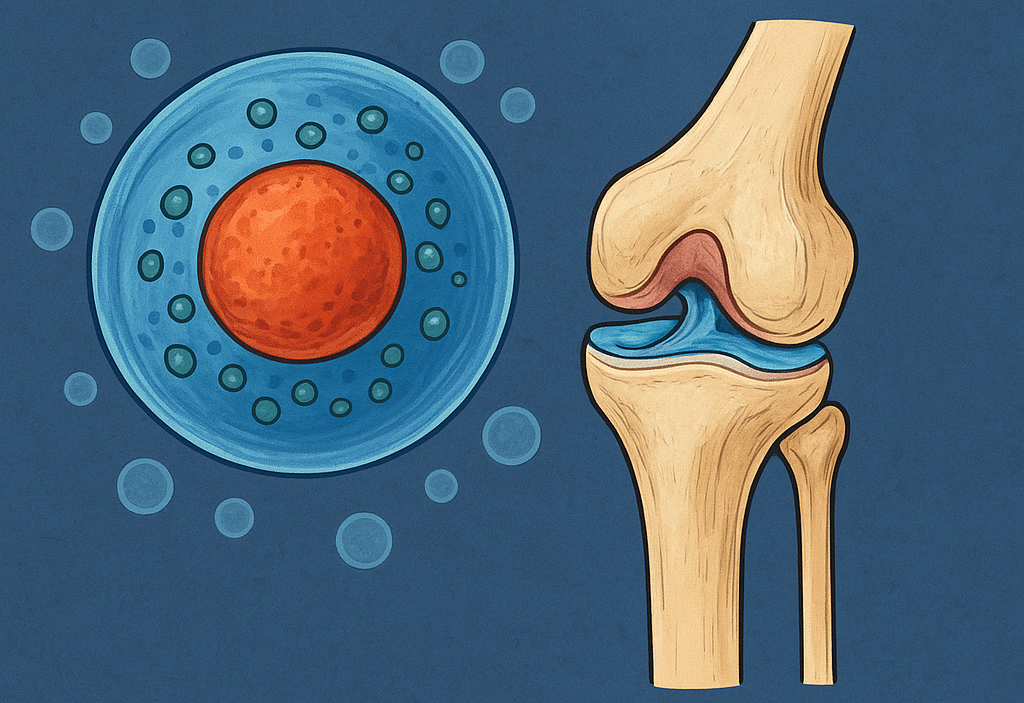
My research focuses on developing stem cell-based therapies for meniscus preservation in the knee joint. The meniscus plays a crucial role in load distribution, joint stability and cartilage protection. However, once injured, its natural healing capacity is extremely limited. Traditional partial meniscectomy, while providing pain relief, may accelerate the progression of osteoarthritis over the long term.
We utilize synovial mesenchymal stem cells (MSCs), which can be harvested from the knee synovium through minimally invasive procedures. These cells are transplanted following meniscus repair, with the goal of enhancing healing and potentially preventing the onset and progression of osteoarthritis. Synovial MSCs demonstrate promising proliferative potential and secrete reparative factors, showing encouraging results in both preclinical and clinical studies.
Our approach represents a potential paradigm shift - from the traditional “remove the damaged tissue” strategy to “repair and preserve using biological enhancement.” This biological augmentation could change how we treat meniscus injuries, with the hope of preventing the degenerative cascade that may lead to osteoarthritis.
2) Why is meniscus preservation so important?
The meniscus appears to be fundamentally linked to long-term knee health and function. Partial meniscectomy increases the risk of cartilage degeneration and the development of osteoarthritis. In young, active individuals, the loss of meniscal function can significantly impact quality of life and athletic performance. Furthermore, successful articular cartilage regeneration appears to depend on the meniscus serving as a biological "template" - without it, cartilage regeneration becomes extremely challenging.
Our research using 3D MRI technology has provided new insights into this process. Through cross-sectional studies utilizing our developed 3D MRI techniques, we observed that in medial-type knee osteoarthritis, the medial meniscus becomes extruded, and cartilage wear occurs along the inner edge of the medial meniscus. We also found associations between medial meniscus damage and degeneration and this extrusion process. These findings highlight the critical role of meniscal integrity in maintaining joint health.
From an SDG 3 perspective, meniscus preservation addresses non-communicable disease prevention (Target 3.4) and supports healthy aging across the lifespan. Preventing osteoarthritis through early intervention aligns with the goal of ensuring healthy lives and promoting well-being for all at all ages.
Current treatment options are limited. While allograft transplantation exists, it faces significant challenges, including donor shortages, size-matching difficulties, and potential complications. Furthermore, in my country, Japan, this procedure is not institutionally approved. Many patients are told their only option is conservative treatment, which has significant limitations, or they may eventually require joint replacement.
Stem cell therapy may offer hope by potentially enhancing the body’s intrinsic healing potential, opening new avenues for preserving the meniscus—even in cases previously considered irreparable. This is particularly relevant given that knee osteoarthritis affects millions worldwide and represents a major public health burden. By potentially preventing meniscus loss, we may be able to delay osteoarthritis progression, maintain patients' mobility and quality of life, and reduce healthcare costs globally.
3) What advantages do synovial MSCs have compared to other stem cell sources?
While MSCs can be derived from various sources—including bone marrow, adipose tissue, and umbilical cord—synovial MSCs appear to possess certain advantages for orthopedic applications. They can be harvested under arthroscopy or ultrasound guidance using only local anesthesia, making the procedure minimally invasive and patient-friendly. These cells demonstrate promising expansion capabilities in culture and show potential for cartilage and meniscus repair.
In comparative studies where MSCs from various tissue sources were prepared under identical conditions and evaluated both in vitro and in vivo, synovial MSCs showed consistent cell yields and superior cartilage matrix production under our laboratory conditions. These results support the potential advantages of synovial MSCs for cartilage and meniscus repair applications.
Importantly, synovial MSCs secrete various reparative and anti-inflammatory factors, including lubricin, bone morphogenetic proteins (BMPs), and tumor necrosis factor-stimulated gene-6 (TSG-6). Because they originate from the intra-articular environment, they may integrate more naturally with meniscal tissue and potentially adapt better to the joint's biological environment.
Compared to bone marrow MSCs, which face challenges in ensuring consistent cell yields, or adipose-derived MSCs, which may have different differentiation potentials, synovial MSCs appear well-suited for joint applications. Their location within the synovial membrane suggests that they may already be adapted to the joint environment and may have evolved to respond to joint injuries.
4) What have clinical studies revealed so far?
We have conducted three clinical trials, progressing through Phase 3, using autologous synovial MSCs in patients with difficult-to-treat meniscus tears that would otherwise typically require resection. The safety profile has been encouraging—no serious adverse events were observed, demonstrating apparent safety and feasibility of this approach.
Arthroscopic re-evaluation and MRI have suggested possible preservation of meniscal morphology, with many patients reporting improvements in both symptoms and knee function. Remarkably, cell transplantation not only prevented re-tearing of the sutured meniscus but also resulted in cases where the meniscus actually increased in size. The results showed variation depending on patient populations and injury types within our study cohorts.
However, it's important to note that long-term follow-up studies and accumulating clinical data through real-world usage remain essential to more definitively establish efficacy and confirm potential osteoarthritis prevention. While the structural and symptomatic improvements we've observed are encouraging and suggest potential clinical value, larger datasets and longer follow-up periods are needed to draw definitive conclusions about long-term outcomes.
These preliminary findings represent an important step forward in translating laboratory discoveries into potential patient benefits, and we remain cautiously optimistic about the prospects for broader clinical implementation pending further validation.
5) How do you think this therapy will impact patients with meniscus injuries?
For young athletes and active middle-aged individuals, this therapy could potentially transform the treatment paradigm from a resection-based approach to "repair plus biological augmentation with MSCs." This shift might reduce meniscectomy rates, potentially lowering the incidence of secondary osteoarthritis, extending activity longevity, and delaying or preventing the need for joint replacement surgery.
The potential impact extends beyond individual patients and directly supports SDG 3's vision of good health and well-being. From a public health perspective, delaying or preventing osteoarthritis could offer significant benefits in reducing healthcare costs and improving population health, contributing to sustainable healthcare systems (Target 3.8). Currently, millions of people live with activity limitations due to knee problems that often originate from meniscus injuries sustained years or decades earlier.
By potentially preserving meniscal function, we're not just treating an injury—we may be preventing a cascade of joint degeneration that affects patients' entire lives. Active individuals might maintain their sports participation longer, workers could potentially avoid activity limitations, and elderly patients could preserve their independence and mobility.
This represents a move toward potentially preventive medicine in orthopedics, addressing underlying pathology rather than just managing symptoms. However, these anticipated benefits require validation through long-term follow-up studies to confirm their realization in clinical practice.
6) How does your research on Stem Cell-Based Therapy for Meniscus Preservation support and contribute to Sustainable Development Goal 3: Good health and wellbeing, and why is this goal so important to meet?
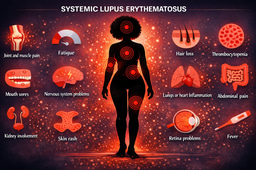
Our meniscus preservation research directly addresses several key targets within SDG 3. First, by potentially preventing osteoarthritis progression, we aim to reduce premature mortality and morbidity from non-communicable diseases (Target 3.4). Osteoarthritis affects over 500 million people globally and represents a leading cause of disability, particularly among aging populations.
Second, this therapy supports universal health coverage (Target 3.8) by potentially offering a more accessible and cost-effective alternative to joint replacement surgery. By preserving natural joint function, we may reduce the substantial healthcare burden associated with advanced osteoarthritis management, making quality orthopedic care more sustainable and available to broader populations.
Third, our work aligns with the goal of ensuring healthy lives and promoting well-being for all ages. Mobility is fundamental to independence, mental health, and social participation. By potentially maintaining joint health throughout the lifespan, we support not just physical health but overall quality of life and well-being.
SDG 3 is critical because health is foundational to all other development goals. Without good health, individuals cannot pursue education, work productively, or participate fully in society. In the context of aging populations worldwide, preventing chronic conditions like osteoarthritis becomes increasingly important for sustainable healthcare systems and thriving communities.
Our research represents the type of innovative, preventive approach needed to achieve SDG 3—addressing disease before it becomes disabling, using biological solutions that work with the body's natural healing capacity, and potentially making advanced care accessible to diverse populations globally.
7) What challenges remain before this therapy can be widely adopted?
Several significant challenges must be addressed for potential widespread adoption. First, we need to standardize MSC manufacturing processes and achieve comprehensive regulatory approval across different countries. This includes establishing consistent protocols for cell harvesting, expansion, quality control, and delivery.
Second, we must establish clear patient selection criteria to identify those who will benefit most from this therapy. Not all meniscus injuries may be suitable, and we need better predictive tools to optimize treatment decisions.
Third, conducting long-term follow-up studies and accumulating clinical data through real-world usage is essential to confirm efficacy, demonstrate cost-effectiveness, and satisfy regulatory requirements. We need robust evidence that this therapy may prevent osteoarthritis progression over decades, not just years—evidence that currently remains limited.
Additionally, raising awareness among physicians and patients is crucial. Meniscus injuries are often underestimated in terms of their potential long-term consequences, but the impact on joint health appears significant. Broad understanding and acceptance of biological preservation strategies will be key to successful adoption.
Finally, healthcare systems need frameworks for evaluating and covering these advanced therapies, which requires demonstrating both clinical and economic value through rigorous studies.
8) How do you balance communication with the public and with researchers?
Communication requires carefully tailored approaches for different audiences. For the general public, I emphasize practical, relatable concepts: that osteoarthritis risk appears to increase with aging, that meniscus dysfunction is a contributing factor, and that preserving the meniscus could be important for maintaining joint health throughout life. I use analogies—comparing the meniscus to a shock absorber in a car—to make complex biology understandable.
For researchers and clinicians, I focus on detailed mechanisms of action, statistical evidence, clinical outcomes, and methodological rigor. I present data transparently, including limitations and areas needing further investigation.
My goal is to provide hope and understanding for patients while maintaining the highest standards of scientific accuracy for professionals. I believe it's crucial to be honest about both the potential promise and the current limitations of our knowledge. Patients deserve realistic expectations, and scientists need complete information to advance the field.
Both audiences benefit from understanding that this research represents a potential shift in how we approach joint injuries—from reactive treatment to possibly proactive preservation.
9) What excites you most about stem cell therapy in orthopaedics?
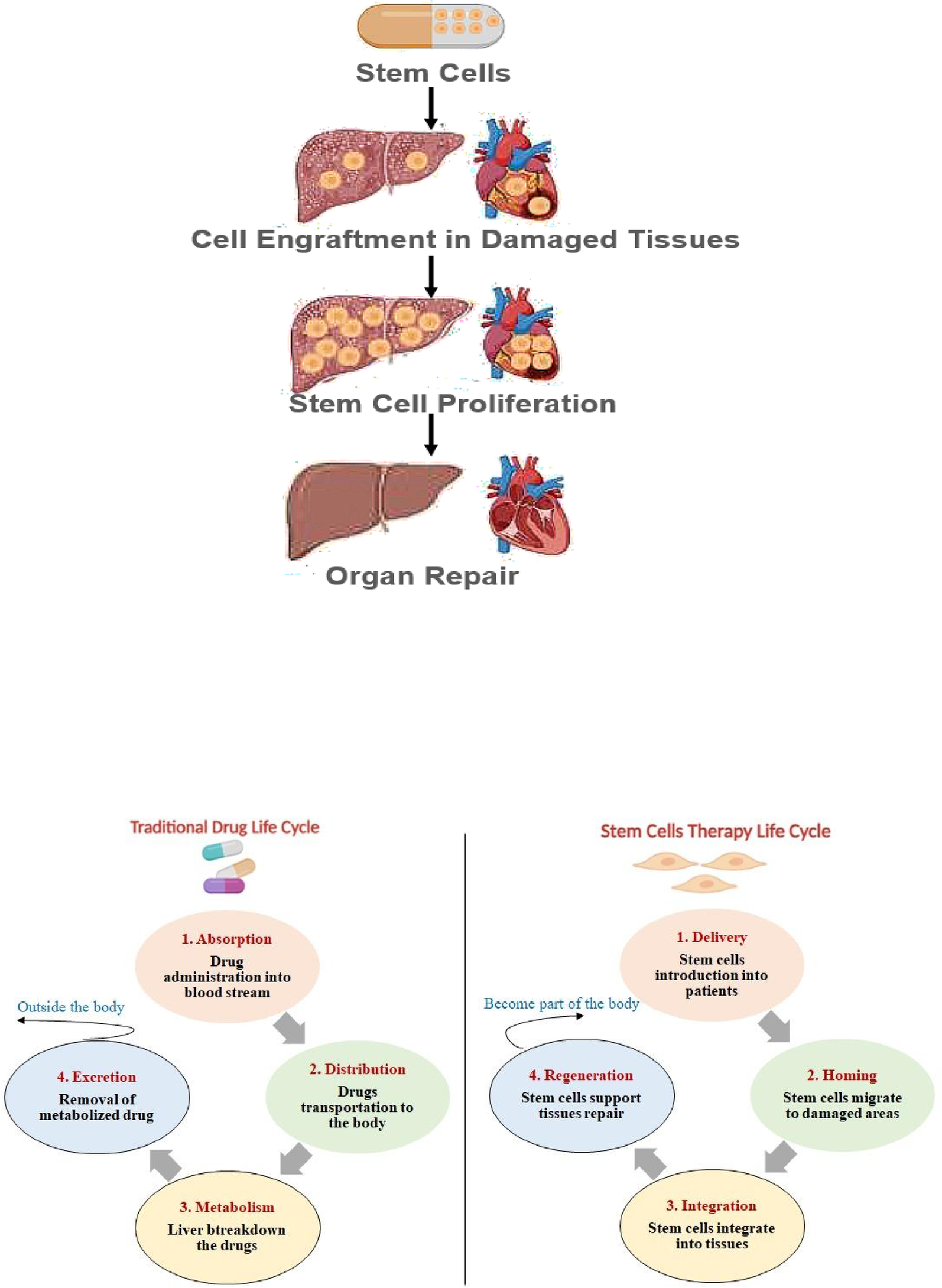
The most exciting aspect is the potential to shift orthopaedics from symptomatic treatment to possible disease-modifying therapy. Traditionally, orthopedics has focused on mechanical solutions—surgical repair, joint replacement, pain management. Stem cell therapy may enable biological tissue regeneration and potentially suppress degenerative processes.
In meniscus preservation specifically, we may be able to interrupt the seemingly inevitable cascade from injury to osteoarthritis. This could represent a significant change in disease trajectory—instead of managing progressive joint destruction, we might prevent it entirely.
What particularly excites me is the possibility of potentially transforming patients' life stories. Instead of an athlete facing career-ending surgery or a middle-aged worker anticipating decades of progressive disability, we might offer preservation of function and prevention of degeneration.
This represents the convergence of multiple scientific advances—our understanding of stem cell biology, tissue engineering, regenerative medicine, and joint physiology—into therapies that could potentially alter the natural history of joint disease. If successful, this could be among the most significant advances in orthopedics in recent decades.
10) How important are collaborations in this field?
Collaboration is absolutely essential for success in stem cell therapy development. This field requires seamless integration of basic science research, cell manufacturing expertise, clinical surgery skills, advanced imaging techniques, regulatory science knowledge, and biostatistics. No single institution possesses all these capabilities at the highest level.
In our work, we collaborate extensively with universities for basic research, hospitals for clinical trials, government agencies for regulatory guidance, and industry partners for manufacturing and commercialization. Each brings unique expertise and resources that are critical for advancing the field.
International collaboration is equally vital. By sharing protocols, data, and experiences across borders, we can accelerate progress for everyone while preventing duplication of effort. The challenges we face—regulatory approval, manufacturing standardization, patient selection—are similar worldwide, and solutions developed in one country may benefit patients globally.
These partnerships also help ensure that potentially effective therapies reach patients as quickly and safely as possible, regardless of their geographic location. The global nature of scientific collaboration is one of our greatest strengths in tackling complex medical challenges.
11) What is your vision for the next decade of meniscus preservation research?
Over the next decade, I envision stem cell therapy potentially progressing from clinical trials toward broader clinical application, though this timeline depends on successful validation of efficacy and safety. Key advances may include refined patient selection algorithms and the possible development of standardized "off-the-shelf" allogeneic MSC products that could eliminate the need for individual cell harvesting.
Advanced imaging technologies, including high-resolution 3D MRI and biomarker analysis, may enable more precise evaluation of meniscus healing and earlier detection of treatment success or failure. We may develop predictive models to identify which patients could benefit most from different therapeutic approaches.
My aspiration is that by 2035, meniscus injuries once routinely treated with resection might instead be managed with repair plus stem cell transplantation as a potential standard of care. Through this possible paradigm shift, we might preserve numerous menisci and potentially prevent many cases of osteoarthritis, achieving meaningful impact on joint health.
This represents more than just a potential new treatment—it could be a fundamental change in how we approach joint injury, moving from acceptance of inevitable degeneration to possible prevention through biological enhancement. By contributing to SDG 3's targets for reducing non-communicable diseases and ensuring healthy lives at all ages, this research could improve many lives worldwide and support more sustainable, equitable healthcare systems. This potential for global impact—preventing disability and preserving quality of life for millions—is what makes this work truly important.
Follow the Topic
-
Stem Cell Research & Therapy

The major forum for translational research into stem cell therapies. An international peer-reviewed journal, it publishes high-quality open access research articles with a special emphasis on basic, translational and clinical research into stem cell therapeutics and regenerative therapies.
Related Collections
With Collections, you can get published faster and increase your visibility.
Neural Stem Cell-derived EVs for Treating Neurological and Neurodegenerative Disorders
As we advance our understanding of the role of neural stem cells (NSCs) and the composition of extracellular vesicles (EVs) they release, we begin to unveil promising pathways to address the challenges posed by debilitating neurological and neurodegenerative disorders. Recent advancements employing NSC-EVs in animal models of disease are showing promise for neuroregeneration and neurorepair. These breakthroughs involve the modulation of neuroinflammation, alleviation of amyloid-beta and phosphorylated tau-related pathological changes, repair of the blood-brain barrier, and improvements in cognitive and mood function. As we further explore these developments, the potential for enhanced synaptic plasticity and improved patient outcomes is becoming increasingly viable. NSC-derived EVs are laden with a rich cargo of microRNAs, proteins, and lipids, capable of mediating powerful antioxidant and anti-inflammatory effects, enhancing cognitive function, and providing neuroprotection. Moreover, the innovative engineering of NSC-EVs can significantly improve their therapeutic potential, positioning them as an ideal biologic for slowing down brain aging and combating a range of diseases, including the difficult-to-treat conditions such as Alzheimer’s disease, Parkinson’s disease, stroke, subarachnoid hemorrhage, traumatic brain injury, multiple sclerosis, and spinal cord injury. These disorders urgently call for groundbreaking therapeutic strategies, and harnessing NSC-derived EVs may pave the way for transformative interventions in the field of neurology.
We invite researchers to contribute to this special Collection by submitting original research articles. A few insightful review articles will also be considered.
Topics of interest include, but are not limited to:
- Mechanisms of NSC-EVs-mediated neuroregeneration and neurorepair
- The role of microRNA and protein cargo of NSC-EVs in neuroprotection
- Strategies for BBB penetration of intravenously administered NSC-EVs
- Targeting of NSC-EVs into specific cell types in the brain
- Mechanisms of antioxidant and antiinflammatory effects of NSC-EVs in the brain
- Modulation of synaptic plasticity by NSC-EVs
- Insights from studies of NSC-EVs in animal models of brain aging, Alzheimer’s and Parkinson’s diseases, traumatic brain and spinal cord injuries, and multiple sclerosis
- Pathway for clinical applications of NSC-EVs in neurological and neurodegenerative disorders
- Production of clinical-grade NSC-EVs
- Innovations in cell-free therapeutic approaches
All submissions in this collection undergo the journal’s standard peer review process. Similarly, all manuscripts authored by a Guest Editor(s) will be handled by the Editor-in-Chief. As an open access publication, this journal levies an article processing fee (details here). We recognize that many key stakeholders may not have access to such resources and are committed to supporting participation in this issue wherever resources are a barrier. For more information about what support may be available, please visit OA funding and support, or email OAfundingpolicy@springernature.com or the Editor-in-Chief.
Publishing Model: Open Access
Deadline: Jun 05, 2026




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in