
The enormous advances in oncological research have led to a significant improvement in the prognosis of many cancer patients in the last decade. In contrast, patients suffering from brain metastases usually have a significantly shortened life expectancy and a poor quality of life. Unfortunately, the current therapeutic options for brain metastases are still very sparse and ineffective. Moreover, the brain is inherently a highly immunosuppressed organ and for this reason, patients with brain metastases were often excluded from clinical trials with immunotherapies. However, the first clinical trials recently proved that the modulation of the immune system is a very promising therapeutic option also for brain metastases.
In our study in Oncogene, we focused on the activation of various members of the Toll-like receptor (TLR) family as potential therapeutic targets in brain metastasis. The TLR family consists of ten different receptors in humans, which are mainly expressed on the plasma membrane. There recognize bacterial components, such as lipoprotein of Gram-positive bacteria (TLR1, 2, 6, and 10) or lipopolysaccharide (LPS) of Gram-negative bacteria (TLR4). The others are located intracellularly (TLR3, 7, 8, and 9) and are mostly able to detect bacterial or viral nucleic acids. TLR signaling in general is a fundamental defense mechanism and very important in the protection of the brain integrity.
In this context, we evaluated systematically the expression of several TLRs in two different cohorts of breast cancer brain metastasis (BCBM) patients and identified TLR4 as interesting druggable candidate target. To investigate this further, we made use of our previously published 3D organotypic ex vivo co-culture system and brain colonization in vivo model. Our experiments confirmed that low-level endogenous activation of the TLR4 pathway supports metastatic brain infiltration. In contrast, a robust exogenous TLR4 stimulation strengthens the organ defense against colonizing cancer cells in the brain microenvironment. This effect was limited on TLR4 activation with LPS. Interestingly, the activation of other TLRs by exogenous ligands did not lead to a comparable result, which underlined the special character of TLR4. Furthermore, we show that therapeutic intervention with the TLR4 agonist LPS leads to a reduction of the metastatic infiltration of the cancer cells at the macro-metastasis / brain parenchyma interface (MMPI) in vivo, which is in line with a better survival of the mice.
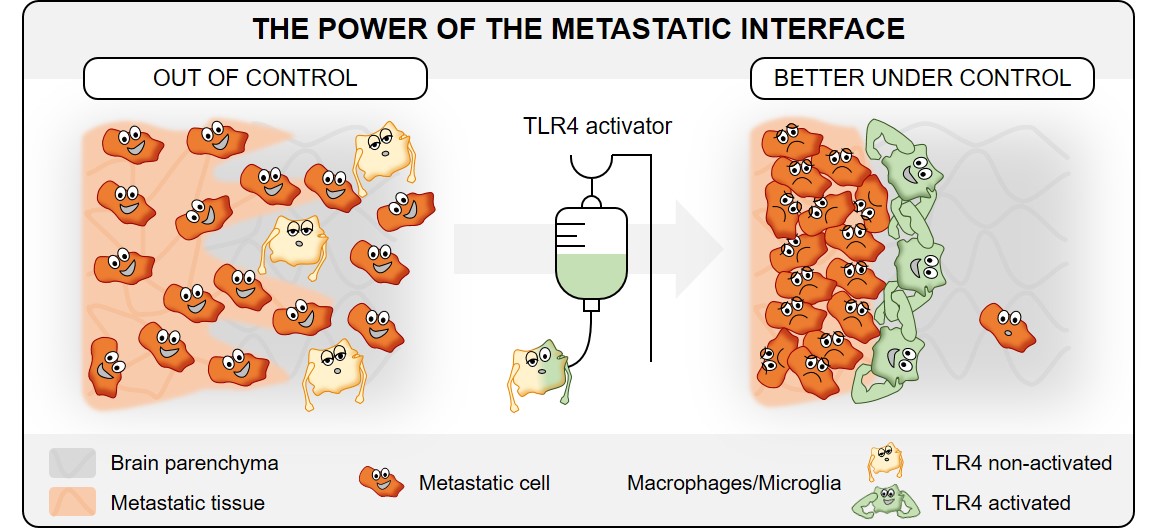
Taken together, in our Oncogene publication we identified TLR4 among the TLR family as the most promising therapeutic target for brain metastasis patients. However, it seems that the application route and time of the treatment are also very important and need further systematic analyses.
Follow the Topic
-
Oncogene

This journal aims to make substantial advances in our knowledge of processes that contribute to cancer by publishing outstanding research.



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in