Enabling the surveillance and therapeutics development at speed for syncytial viruses like SARS-CoV-2
Published in Bioengineering & Biotechnology, Microbiology, and Protocols & Methods
Background
The coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) led to a major public health crisis. Early autopsies showed extensive alveolar damage and multinucleated pneumocytes in the lung tissue of COVID-19 patients.1 The formation of multinucleated syncytia is primarily determined by the fusogenicity of the SARS-CoV-2’s spike protein.2 SARS-CoV-2 variants have been continuously evolving since its emergence. Mutations of spike protein result in numerous variants with varying degrees of infectivity and lethality.3 So, by mapping specific SARS-CoV-2 spike mutations that enhance syncytium-formation potential, we can better predict the pathological consequences of emerging viral genetic variants. In addition, identifying the host factors that are crucial for syncytia formation may reveal new therapeutic targets for disease treatment. Here we developed high-throughput droplet microfluidics and size-exclusion selection methods for studying cell-cell fusion and coupled them with large-scale mutagenesis and clustered regularly interspaced short palindromic repeats (CRISPR) screening to profile the syncytium-forming potential of the spike variants and identify the crucial cellular determinants.
Developing droplet microfluidics- and size-exclusion selection-based screening methods
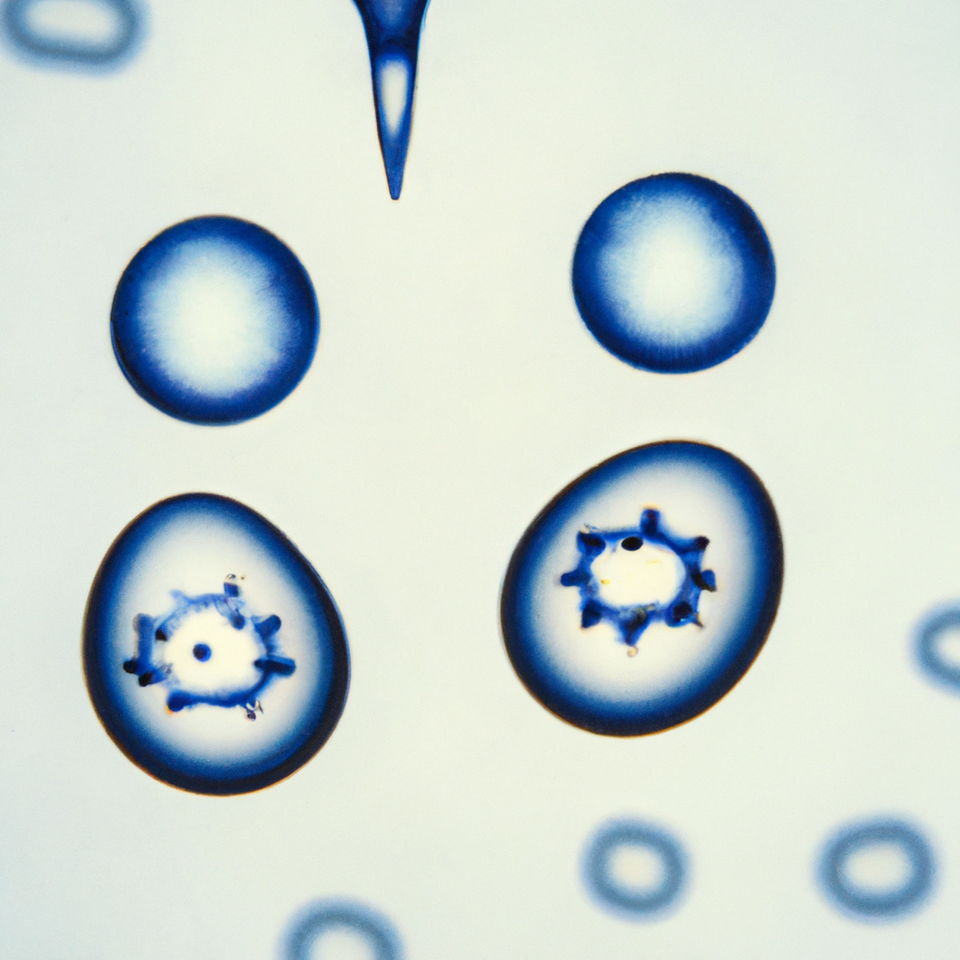
Large-scale screening to characterize cell-cell fusion is technically challenging as this would require a rapid functional readout upon cell-cell contact between two cells. We implemented a split-green fluorescent protein (GFP) complementary system4 to convert the cell fusion event into a GFP signal for detection under microscope and for sorting using fluorescence-activated cell sorting (FACS). Two complementary fragments of GFP are separately expressed on spike-displaying cells and angiotensin-converting enzyme 2 (ACE2)-expressing cells. The GFP signal could be reconstituted upon cell-cell fusion.
In all prior studies, the syncytium-forming potential of different spike variants was profiled one by one using high content microscopy5, 6 but there is a lag time for imaging the first well until the last well of the variant. In the meantime, it would be laborious to construct all the variants one by one thus limiting the throughput of the screening. We utilized the microfluidics-based system to compartmenting the two cells inside the droplets and directly quantify the cell fusion events among a large number of Spike variants. We performed deep mutational scanning on the furin cleavage site and the fusion peptide proximity region (FPPR) 7 of the spike protein to identify key mutations affecting cell-cell fusion. The profiling data uncovered syncytium-enhancing spike mutants and reveals how Omicron could turn from a low- to a high- rate of syncytium-forming strain with a single K854H mutation.
To further increase the throughput of the cell-cell fusion screening, we developed a size-exclusion selection-based strategy which utilize a cell strainer to filter large syncytia as a compartmentation-free method to massively sort fused and unfused cells. We showed that the greater throughput only results in slight reduction in precision and does not compromise the overall screen performance.
Genome-wide CRISPR screening reveals cellular determinants of syncytia
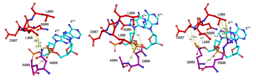
Then we performed a genome-wide CRISPR screen on the receiver cell based on the size-exclusion selection method to find cellular factors that are required for SARS-CoV-2 spike-induced syncytia formation. Considering the ultra-large pool of cells for genome-wide CRISPR screening, we took a reverse selection approach by collecting the unfused single guide RNA (sgRNA)-infected receiver cells in the coculturing system and comparing them with the cell pool before coculture to identify host factors crucial for the syncytium formation.
In addition to the known ACE2 receptors, five other genes (AP2M1, FCHO2, CAB39, RNF2, and GBP6) were identified as potential host factors in the syncytium formation process. Among them, two regulators of clathrin-mediated endocytosis (CME) AP2M1 and FCHO2 knockout showed the best effect of inhibiting spike-induced syncytium formation. These results led us to further investigate the role of CME in SARS-CoV-2 spike-induced syncytium formation. We targeted CME by knocking down clathrin heavy chain (CHC) with siRNA and CME inhibitor Pistop2. They all markedly reduced the SARS-CoV-2 spike-induced syncytium formation. We next validated our findings using live SARS-CoV-2 D614G strain both in vitro and in vivo. We demonstrated that treatment of three FDA-approved drugs (Chlorpromazine, Fluvoxamine, and Promethazine) targeting CME inhibits syncytium formation in SARS-CoV-2 D614G infected cells. Chlorpromazine and Fluvoxamine can inhibit SARS-CoV-2 replication and syncytium formation in the lung of SARS-CoV-2 D614G-infected hamsters.
Overall, these results validated our high-throughput screening strategy for identifying key factors for SARS-CoV-2 spike-induced syncytium formation. Our findings underscore the involvement of CME in this process and provide support for the repurposing of chlorpromazine, fluvoxamine, and other potential CME inhibitors to alleviate the virus-induced pathological damages.
Conclusion
Blending the cross-disciplinary expertise in high-throughput CRISPR screening, large-scale mutagenesis, droplet microfluidics, and virology, we developed new methods for biomedical applications. The new platform will allow systematic profiling of the fusogenicity of a broad spectrum of the viruses in addition to SARS-CoV-2, including human immunodeficiency virus (HIV)8, respiratory syncytial virus (RSV)9, herpesviridae10 and other coronaviridae which induce syncytium formation. On top of that, defining the common and unique determinants for each type of virus-induced syncytium formation could help combat the disease pathogeneses. The system can even be applied to study a variety of pathological, physiological, and even synthetic cell fusion events. For example, revealing cellular regulators for tumor-normal somatic cell fusion could help combat the disease pathogeneses. Fusion of specific cell types form multinucleated cells including syncytiotrophoblasts, myotubes, and osteoclasts to aid their physiological functions in controlling maternal-fetal material exchange at the placenta, coordinating muscle contraction, and facilitating bone resorption, respectively.11 Artificial fusion of B-cells and myeloma cells produces hybridoma as the workhorse for antibody production.12 Fusion of human embryonic stem cells with somatic cells reprograms them to pluripotency as cell sources for regenerative medicine.13 Fusion of dendritic cells with tumor cells was reported to produce hybrids that express the tumor-associated antigens and is being tested as potential cancer immunotherapy reagents.14
References
- Bussani, R. et al. Persistence of viral RNA, pneumocyte syncytia and thrombosis are hallmarks of advanced COVID-19 pathology. EBioMedicine 61, 103104 (2020).
- Braga, L. et al. Drugs that inhibit TMEM16 proteins block SARS-CoV-2 spike-induced syncytia. Nature 594, 88-93 (2021).
- Rajah, M.M. et al. SARS-CoV-2 Alpha, Beta, and Delta variants display enhanced Spike-mediated syncytia formation. EMBO J 40, e108944 (2021).
- Cabantous, S., Terwilliger, T.C. & Waldo, G.S. Protein tagging and detection with engineered self-assembling fragments of green fluorescent protein. Nat Biotechnol 23, 102-107 (2005).
- Braga, L. et al. Drugs that inhibit TMEM16 proteins block SARS-CoV-2 spike-induced syncytia. Nature 594, 88-+ (2021).
- Sanders, D.W. et al. SARS-CoV-2 requires cholesterol for viral entry and pathological syncytia formation. Elife 10 (2021).
- Cai, Y. et al. Structural basis for enhanced infectivity and immune evasion of SARS-CoV-2 variants. Science 373, 642-648 (2021).
- Lifson, J.D. et al. Induction of CD4-dependent cell fusion by the HTLV-III/LAV envelope glycoprotein. Nature 323, 725-728 (1986).
- Chanock, R., Roizman, B. & Myers, R. Recovery from infants with respiratory illness of a virus related to chimpanzee coryza agent (CCA). I. Isolation, properties and characterization. Am J Hyg 66, 281-290 (1957).
- Hoggan, M.D. & Roizman, B. The isolation and properties of a variant of Herpes simplex producing multinucleated giant cells in monolayer cultures in the presence of antibody. Am J Hyg 70, 208-219 (1959).
- Brukman, N.G., Uygur, B., Podbilewicz, B. & Chernomordik, L.V. How cells fuse. J Cell Biol 218, 1436-1451 (2019).
- Kohler, G. & Milstein, C. Continuous cultures of fused cells secreting antibody of predefined specificity. Nature 256, 495-497 (1975).
- Yamanaka, S. & Blau, H.M. Nuclear reprogramming to a pluripotent state by three approaches. Nature 465, 704-712 (2010).
- Chen, E.H. & Olson, E.N. Unveiling the mechanisms of cell-cell fusion. Science 308, 369-373 (2005).
Written by Charles Chan and Bei Wang
Follow the Topic
-
Nature Biomedical Engineering

This journal aspires to become the most prominent publishing venue in biomedical engineering by bringing together the most important advances in the discipline, enhancing their visibility, and providing overviews of the state of the art in each field.
Related Collections
With Collections, you can get published faster and increase your visibility.
Biosensing
Publishing Model: Hybrid
Deadline: Mar 26, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in