Top Six Articles on Antimicrobial Stewardship
Published in Microbiology
-
Introduction: Why AMR and AMS Matter in 2024
Antimicrobial resistance (AMR) remains a pressing global health crisis, with its implications threatening the efficacy of life-saving treatments. In 2024, the urgency to address AMR has intensified, driven by its growing impact on healthcare systems worldwide. Antimicrobial stewardship (AMS) emerges as a pivotal strategy to mitigate the spread of resistance by promoting the judicious use of antibiotics and preserving their effectiveness for future generations.
This article highlights significant advancements in AMR and AMS from the past year, summarising key research findings and their implications for global health. By reflecting on these developments, we aim to provide actionable insights for advancing AMS strategies and addressing the ever-evolving challenges posed by AMR.
-
Summary of Tops Highlighted 2024 Research Articles

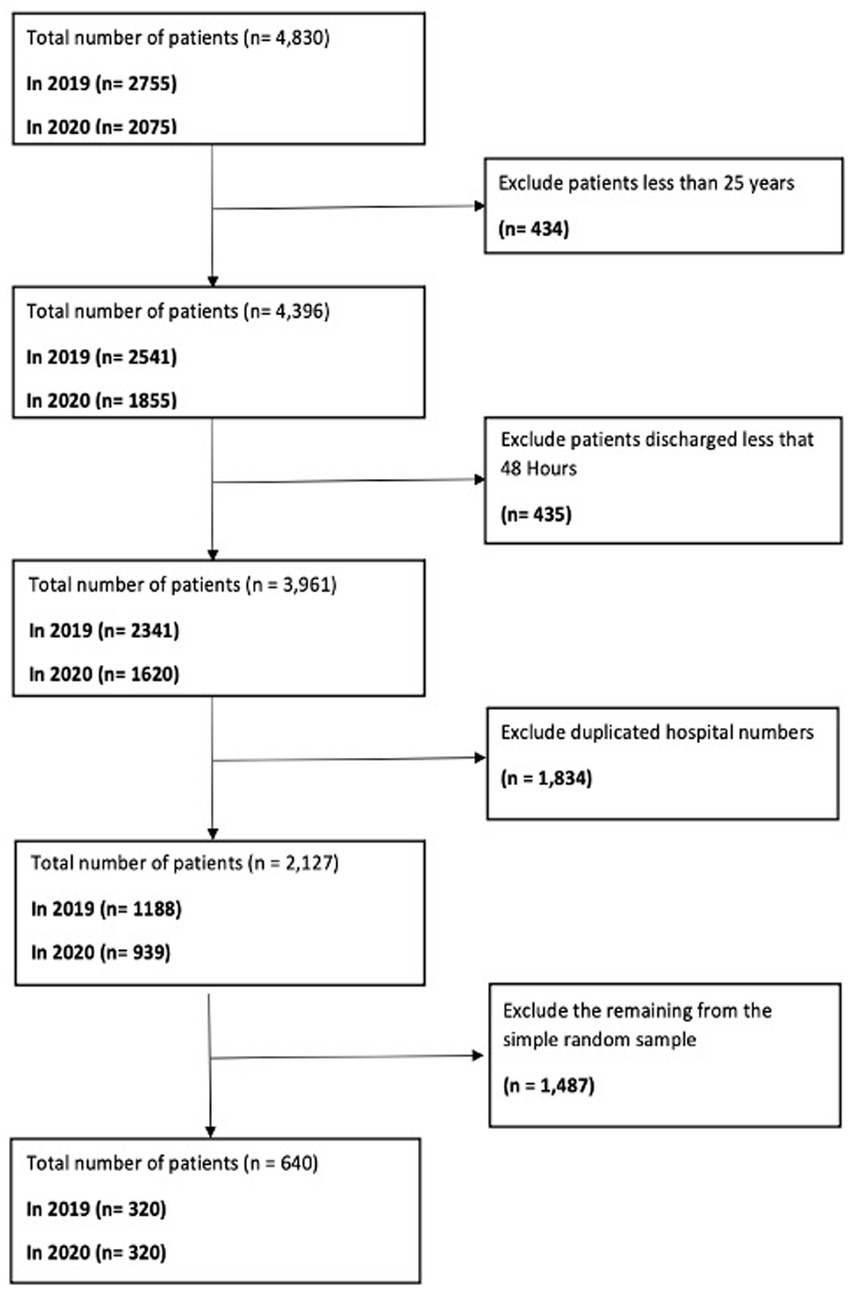
Study 1: WHO AWaRe Classification for Antibiotic Stewardship – Tackling AMR in an English NHS Foundation Trust During COVID-19
Key Findings:
- Significant rise in azithromycin and amoxicillin/clavulanic acid usage during the COVID-19 pandemic.
- Increased prescribing of "Watch" category antibiotics raises AMR risks.
- Analysis of 640 RTI cases using WHO’s AWaRe classification highlights the importance of structured prescribing and AMS measures to address shifting antibiotic trends in a global health crisis.
Implications:
- Elevated use of "Watch" antibiotics underscores the necessity for strengthened AMS policies and targeted training.
- WHO’s AWaRe classification serves as a critical tool for monitoring antibiotic usage and addressing AMR.
- Findings emphasise the need for robust prescribing protocols to safeguard patient safety and mitigate resistance.
Future Directions:
- Conduct longitudinal studies to assess sustained prescribing trends.
- Broaden research scope to include outpatient settings and diverse infection types.
- Implement AMS training programmes and digital tools for enhanced real-time antibiotic monitoring.
- Advocate for integrating global AWaRe-based AMS frameworks to effectively combat AMR.
Link of the study
Study 2: Antimicrobial Stewardship Implementation Before and During the COVID-19 Pandemic in Acute Care Settings – A Systematic Review
Key Findings:
- AMS strategies were categorised into core and supplemental strategies and their implementation measured before (BP) and during (DP) the pandemic.
- Analysis of 13 studies highlighted the effectiveness of AMS strategies in maintaining rational antibiotic use and mitigating AMR risks, especially during crises.
- Lessons learned from the COVID-19 pandemic revealed the importance of adaptable AMS approaches to ensure preparedness for future health emergencies.
Implications:
- AMS programmes should integrate evidence-based core and supplemental strategies tailored to pandemic and non-pandemic settings.
- Public Health England (PHE) toolkit provides a benchmark for AMS implementation, enhancing consistency and impact in acute care settings.
- Findings emphasise the need for continuous monitoring and evaluation of AMS practices to ensure the rational use of antibiotics and minimise AMR threats.
Future Directions:
- Conduct longitudinal studies to assess the long-term impact of AMS strategies BP and DP.
- Expand research scope to evaluate AMS implementation in diverse healthcare systems and resource-limited settings.
- Develop innovative AMS measures and toolkits for crisis management and emergency preparedness.
- Provide empirical data to identify which AMS strategies are most effective across varying health crises and ensure scalability and adaptability.
Link of the study
Study 3: Impact of COVID-19 on ‘Start Smart, Then Focus’ Antimicrobial Stewardship at One NHS Foundation Trust in England
Key Findings:
- Patient Profile: The study analysed 640 adult patients admitted for RTIs, including pneumonia and COVID-19 cases (2020), with the majority aged 66–85 years.
- Predominant Diagnosis: Community-acquired pneumonia (CAP) was the most common diagnosis (39.4% in 2019, 42.5% in 2020).
- Antibiotic Reviews: Reviews were conducted within 48–72 hours post-admission with no significant timing differences between 2019 and 2020.
- AMS Interventions: During the pandemic, significant differences were observed in ‘Continue Antibiotics’ (OR 3.36, p = 0.015) and ‘De-escalation’ (OR 2.77, p = 0.005) interventions, highlighting a shift in AMS practices.
Implications:
- The findings highlight the critical role of the ‘Start Smart, Then Focus’ framework in ensuring timely and effective AMS interventions during the pandemic.
- Enhanced AMS practices, including de-escalation, were vital in combating AMR risks amid increased antibiotic use during the pandemic.
- Comorbidities play a crucial role in AMS decision-making, underlining the need for tailored interventions for vulnerable populations.
Future Directions:
- Conduct further studies to explore the long-term impact of AMS adaptations during the pandemic on AMR trends.
- Investigate the scalability of SSTF guidelines across different healthcare settings.
- Develop targeted AMS strategies for high-risk groups, integrating digital tools to optimise antibiotic stewardship.
- Strengthen AMS training for healthcare professionals to ensure adherence to SSTF principles in crisis scenarios.
Link of the Study
Study 4: An Evaluation of the Five Rights of Antibiotic Safety Before and During COVID-19 at an NHS Foundation Trust in the United Kingdom
Key Findings:
- Antibiotic Prescribing Practices:
- Increased instances of inappropriate dosing and administration routes during the pandemic.
- Slight improvement in prescribing durations, reflecting some adherence to AMS guidelines.
- Stable rates of appropriate antibiotic selection aligned with antimicrobial guidelines, despite other inappropriate practices.
- Impact of COVID-19: The pandemic exacerbated inappropriate prescribing patterns, highlighting challenges in maintaining AMS during health crises.
Implications:
- Strengthened AMS Practices:
- Findings underscore the critical role of the 'Five Rights of Antibiotics' (right patient, right drug, right dose, right route, right time) in maintaining antibiotic safety.
- Stable antibiotic selection rates reflect the potential for adherence to guidelines even under pandemic pressures.
- AMS Education and Oversight:
- Increased educational initiatives targeting appropriate dosing and administration practices are necessary.
- Systematic oversight is vital to address gaps in prescribing during emergencies like COVID-19.
Future Directions:
- Enhanced Training: Develop focused AMS training programmes for healthcare professionals to reinforce the principles of the 'Five Rights.'
- Real-Time Monitoring Tools: Introduce digital AMS tools for real-time prescribing guidance and error detection.
- Crisis Preparedness: Conduct scenario-based studies to simulate AMS challenges in future health crises and create resilient prescribing strategies.
- Broader Evaluations: Expand the study to assess AMS practices across multiple NHS Trusts for a comprehensive understanding of prescribing trends.
Link of the Study
Study 5: Novel Survey Distribution Methods: Impact on Antimicrobial Resistance Research Outcomes
Key Findings:
- Achieved a 100% response rate (240 participants) within 3 months using hybrid survey strategies.
- QR-code posters and digital dissemination significantly boosted participation.
- Participant feedback praised accessibility, user-friendly design, and effective communication.
Implications:
- Enhanced AMS research by effectively engaging busy healthcare professionals.
- Customizable methods suited for resource-limited settings to overcome participation barriers.
Future Directions:
- Scale hybrid methods to broader healthcare settings and public health domains.
- Leverage AI-driven analytics for real-time tracking and response improvement.
- Integrate findings into AMS training and global AMR awareness campaigns.
This study highlights the value of hybrid survey strategies in advancing AMR research and public health efforts.
Link of the Study
Study 6: How Pharmacists Can Contribute to Effective Antimicrobial Reviews: Best Practices and Strategies
Key Findings
- Antimicrobial Resistance (AMR) Crisis: AMR is a significant global health threat, responsible for 4.95 million deaths in 2019, with projections reaching 10 million annually by 2050.
- Role of Pharmacists in AMS: Pharmacists are pivotal in implementing antimicrobial stewardship (AMS) by ensuring the judicious use of antibiotics, reducing misuse, and improving patient outcomes.
- AMS Tools and Frameworks: Utilisation of the 'Start Smart Then Focus' toolkit and Antimicrobial Prescribing and Stewardship Competency Framework enhances adherence to AMS principles.
- Best Practices: Effective antimicrobial reviews involve infection verification, appropriate antimicrobial selection, person-centred care, documentation, and monitoring.
- Educational Impact: Structured antimicrobial reviews significantly improve the understanding and application of AMS practices among healthcare professionals, including pharmacists.
Implications
- Healthcare System Improvements: The integration of AMS tools like the 'Start Smart Then Focus' toolkit leads to better antibiotic prescribing practices, improving patient safety and reducing AMR risks.
- Pharmacist-Centric Role: Empowering pharmacists through training and resource allocation strengthens AMS implementation across healthcare settings.
- Economic Impact: Reduced misuse of antibiotics minimises healthcare costs associated with resistance-related complications.
- Global Collaboration: Sharing best practices and standardised AMS protocols across regions ensures a unified approach to combat AMR.
Future Directions
- Expanded Training Programs: Develop targeted AMS training for pharmacists and healthcare providers, incorporating case-based learning and real-world applications.
- Digital Integration: Leverage technology, such as AI-driven decision support systems, to streamline antimicrobial reviews and enhance adherence to guidelines.
- Policy Development: Advocate for national and global policies mandating regular AMS audits and reviews in all healthcare settings.
- Cross-Disciplinary Collaboration: Strengthen collaboration among pharmacists, prescribers, and healthcare teams to ensure comprehensive AMS practices.
- Research Opportunities: Conduct longitudinal studies to evaluate the long-term impact of AMS tools and strategies on AMR trends.
Link of the Study
-
Global and Regional Impacts of these Antimicrobial Research
Global Impacts:
- Aligns with WHO AMR Global Action Plan, reinforcing global strategies to combat antimicrobial resistance.
- Highlights the role of AMS in reducing AMR threats, contributing to global public health improvements.
Regional Insights:
- Identifies unique challenges in high-burden areas and developing countries, such as resource limitations and lack of awareness.
- Provides tailored AMS strategies to address regional disparities, enhancing the effectiveness of global AMR initiatives.
Significance:
- Bridges the gap between global objectives and local implementation, ensuring a unified approach to AMR mitigation.
5. Vision for 2025 and Recommendations
Vision for 2025:
- Strengthen AMS integration into health systems, focusing on One Health approaches.
- Expand digital innovations for real-time antimicrobial surveillance and decision support.
- Increase collaboration across global and regional AMS networks to address AMR comprehensively.
Recommendations:
- For Policymakers: Develop and enforce national AMS frameworks aligned with WHO guidelines.
- For Healthcare Professionals: Promote continuous AMS training and implement digital tools to optimise prescribing practices.
- For Researchers: Prioritise longitudinal studies on AMR trends and assess the effectiveness of AMS interventions in diverse settings.
These initiatives will ensure sustainable progress in combating AMR and improving global health outcomes.
6. Conclusion and Call to Action
- Reinforcing Importance: Collaboration and innovation remain pivotal in combating antimicrobial resistance (AMR). The synergy between global initiatives and local implementation ensures impactful outcomes.
- Focus Areas: Strengthening antimicrobial stewardship (AMS) training, enhancing surveillance systems, and amplifying public health campaigns are essential to sustaining progress.
- Call to Action: Policymakers, healthcare professionals, and researchers must prioritise AMS efforts, leveraging technology and partnerships to mitigate AMR effectively.
Keywords: AMS goals 2025, AMR One Health strategy, AMS digital innovation




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in