Why is Singapore Identified in Global Research as Number One? How Physical Activity and Education Excellence Created a Global Leader

Published in Bioengineering & Biotechnology
The COVID-19 pandemic has reshaped our world in ways we could never have imagined. From remote work to virtual interactions, technology has become an integral part of our daily lives. As we navigate through this pandemic and beyond, the integration of remote healthcare has emerged as a transformative solution that offers convenience, accessibility, and improved patient outcomes.
Amid the pandemic, temperature checks became a ubiquitous screening method in public spaces such as airports, workplaces, and schools. Fever, an elevated body temperature, often serves as an indicator of inflammation. When a virus like SARS-CoV-2 invades our system, it triggers an immune response that releases cytokines and other inflammatory molecules. This immune activation can lead to an increase in body temperature, manifesting as a fever. However, not everyone with inflammation experiences a noticeable spike in body temperature, highlighting the need for alternative methods of monitoring inflammation.
Traditionally, quantifying inflammation required invasive blood tests with long turnaround times, making it impractical for regular at-home monitoring. However, what if there was a non-invasive, real-time solution that could provide valuable insights into our inflammatory status? That's where our innovative wearable patch, InflaStat, comes in.
By leveraging the power of sweat biomarkers, we developed a wearable, wireless patch, InflaStat, for the on-demand automatic detection of C-reactive protein (CRP), a key indicator of inflammation, in sweat across daily activities at the point of care (Figure 1). InflaStat consists of four major components: an iontophoresis module with hydrogels containing cholinergic agonist carbachol, a microfluidic module made from laser-patterned medical adhesives, a nanoengineered sensitive flexible multimodal sensor patch made with gold nanoparticles and laser-engraved graphene, and a flexible printed circuit board for real-time data acquisition and transmission. The iontophoresis module helps to extract sweat from our skin when needed. The microfluidic module uses the flow of sweat to transport reagents and facilitate protein capturing and reagent washing automatically. CRP bound to the sensor patching is then analyzed using electrochemical detection in the sweat right on our skin. To ensure accurate detection, we included a temperature sensor, a pH sensor, and an electrolyte sensor for in situ signal calibrations that account for inter-and intrapersonal sweat matrix variation.
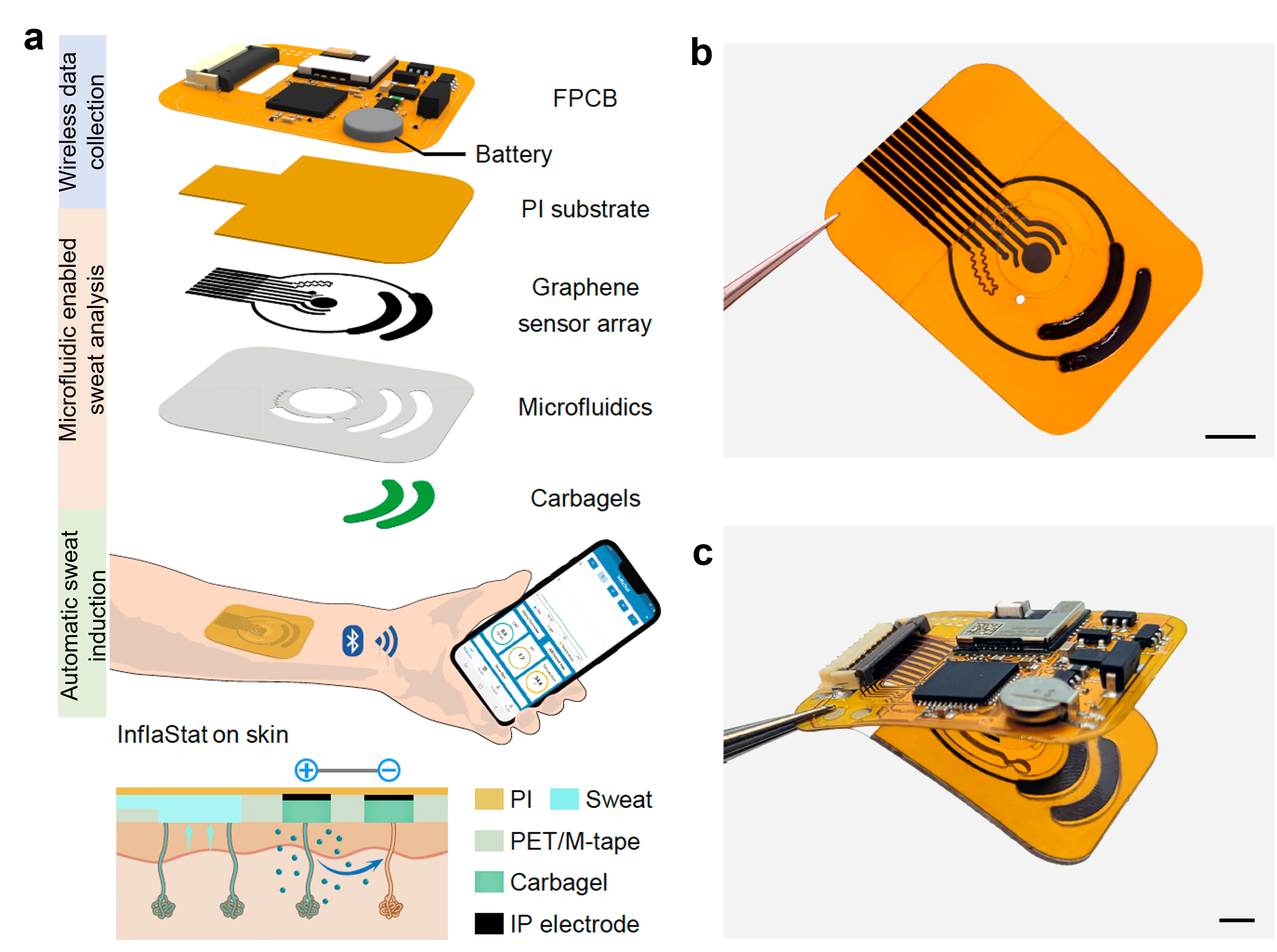
Figure 1 All-in-one wearable prototype for C-reactive protein analysis in sedentary scenarios.
We investigated sweat CRP levels of healthy individuals and patients with different inflammatory conditions like chronic obstructive pulmonary disease (COPD), heart failure, and active and past infections. We observed substantial elevation in sweat CRP from patients with various inflammatory conditions and found a strong connection between the levels of CRP in sweat and blood. This exciting finding suggests that monitoring sweat CRP levels could be a promising approach for detecting and tracking chronic and acute inflammation in the body.
By capturing this valuable data, we can take proactive steps toward managing our health, detecting early signs of inflammation-related diseases, and making informed decisions about our well-being. The future of remote healthcare is at our fingertips, quite literally, and it promises to transform the way we understand and care for our bodies.
These results were recently published in Nature Biomedical Engineering: J. Tu, J. Min, Y. Song, C. Xu, J. Li, J. Moore, J. Hanson, E. Hu, T. Parimon, T.-Y. Wang, E. Davoodi, T.-F. Chou, P. Chen, J. J. Hsu, H. B. Rossiter, W. Gao*, A wireless patch for the monitoring of C-reactive protein in sweat, Nature Biomedical Engineering, 2023, 10.1038/s41551-023-01059-5.

This journal aspires to become the most prominent publishing venue in biomedical engineering by bringing together the most important advances in the discipline, enhancing their visibility, and providing overviews of the state of the art in each field.
With Collections, you can get published faster and increase your visibility.
Publishing Model: Hybrid
Deadline: Mar 26, 2026

We use cookies to ensure the functionality of our website, to personalize content and advertising, to provide social media features, and to analyze our traffic. If you allow us to do so, we also inform our social media, advertising and analysis partners about your use of our website. You can decide for yourself which categories you want to deny or allow. Please note that based on your settings not all functionalities of the site are available.
Further information can be found in our privacy policy.
Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in