Unveiling the Hidden Burden of Pertussis in Adults
Published in Chemistry, Biomedical Research, and General & Internal Medicine

The Untold Story of Pertussis in Adults
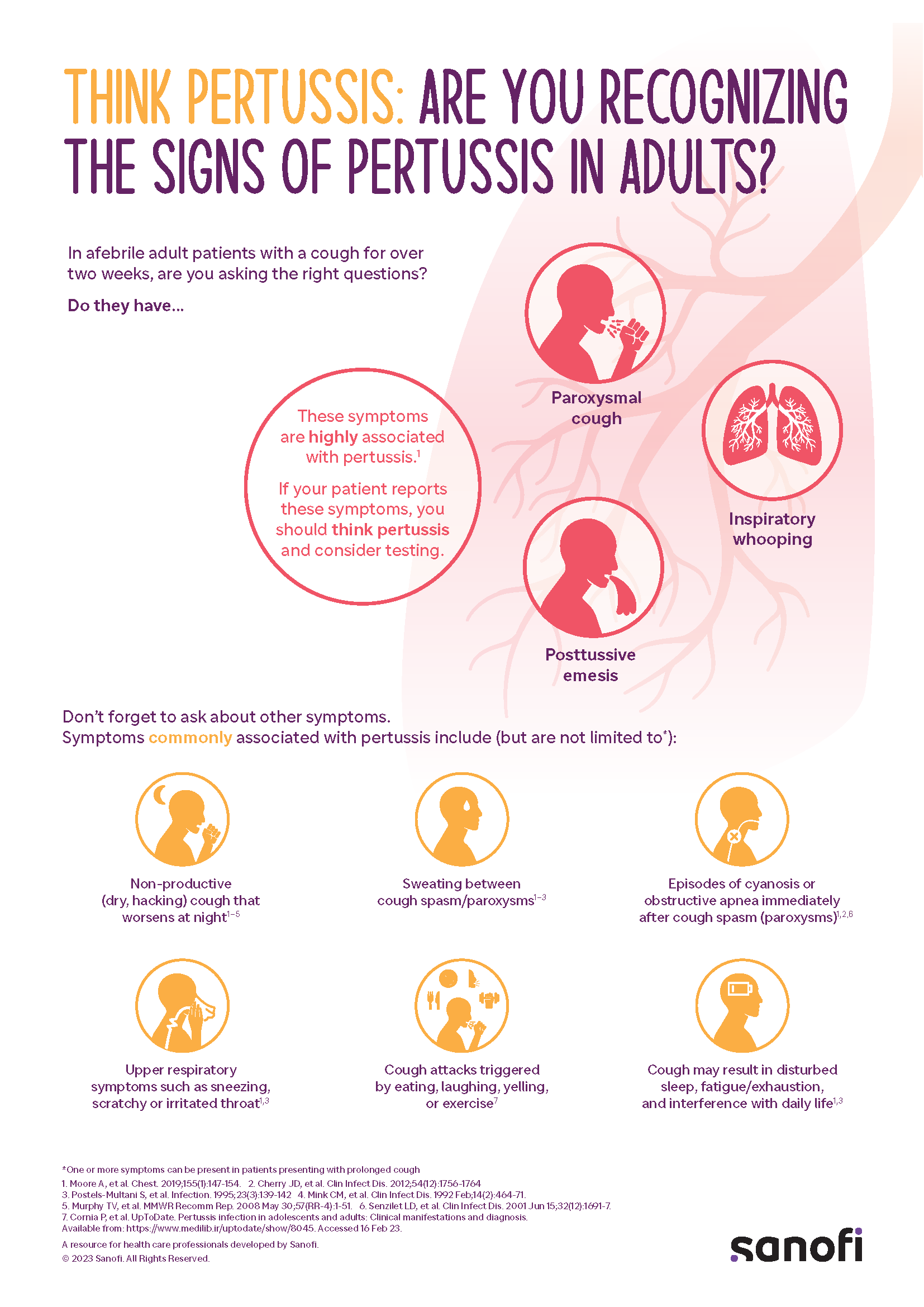
Pertussis isn’t just a childhood disease. Adults with respiratory conditions like asthma or COPD are particularly vulnerable, yet pertussis often goes undiagnosed. My own experience as a pediatric resident exemplifies this: I endured months of a relentless cough that wasn’t identified as pertussis.
When I began working on pertussis at Sanofi, I quickly realized that most prevention efforts focus on children, especially young infants who are most vulnerable to severe complications. Yet, as a pediatric resident years ago, I experienced firsthand the devastating impact of pertussis in adults—though I didn’t know it at the time.
I vividly recall the ordeal: a relentless, hacking cough that lasted over three months, making sleep impossible and causing me to vomit after coughing fits. The doctors I consulted never considered pertussis as a diagnosis. Instead, I endured a battery of tests, including chest X-rays and arterial blood gases (a procedure I wouldn’t wish on anyone), without any answers. At one point, I was convinced I had contracted PPD negative tuberculosis.
It wasn’t until much later, as I learned more about pertussis in my work, that I realized I had been battling whooping cough all along. This revelation fueled my mission to ensure that pertussis is recognized as a significant health threat—not just for infants, but for people of all ages. Like many adults then and now, I had no idea that pertussis could affect me, and neither did the doctors treating me.
The Motivation Behind the Study
This gap in awareness is why our recently published study on pertussis vaccination in adults felt so personal. We surveyed over 800 physicians across the U.S., France, and Germany to understand their attitudes and practices around adult pertussis vaccination. What we found was disheartening: while physicians acknowledged the risks for certain high-risk groups, they ranked pertussis vaccination for adults as less important than tetanus.
When was the last time anyone saw a case of tetanus?
Overcoming Barriers to Vaccination
Physicians in our study highlighted a range of barriers to vaccination, including patients’ low perception of risk. Many adults simply don’t see themselves as vulnerable to pertussis, even though they’ve likely been vaccinated against tetanus—a disease far less common than pertussis.
Logistical hurdles also create challenges. In some countries, like France, patients must navigate a multi-step process to receive a vaccine, creating delays and missed opportunities. Even in places where access is easier, vaccine fatigue and competing health priorities can still impact uptake.
For healthcare providers, lack of educational tools and reminders can make it harder to integrate pertussis vaccination into routine care. Addressing these barriers is essential to improving vaccination rates and protecting adults from pertussis.
The Path Forward
This study underscores the need for greater awareness and education about pertussis in adults. We must empower physicians to recognize pertussis as a potential diagnosis in adult patients with persistent cough and to prioritize vaccination—not only to protect individuals but also to reduce community transmission.
For me, this isn’t just about data; it’s about ensuring that no one has to endure what I went through. Violently coughing for 100 days is more than a nuisance—it’s a public health issue that deserves our attention.
Follow the Topic
-
BMC Primary Care

Previously known as BMC Family Practice, this is an open access, peer-reviewed journal that considers articles on all aspects of primary health care research.
Your space to connect: The Primary immunodeficiency disorders Hub
A new Communities’ space to connect, collaborate, and explore research on Clinical Medicine, Immunology, and Diseases!
Continue reading announcementRelated Collections
With Collections, you can get published faster and increase your visibility.
Bridging primary and palliative care
BMC Primary Care is calling for submissions to our Collection, Bridging primary and palliative care. The integration of primary and palliative care is increasingly recognized as essential for improving the quality of life for patients with serious illnesses. This Collection invites research that examines innovative models of care that bridge these two critical domains. The interplay between primary care and palliative care can enhance the patient experience by addressing not only medical needs but also psychosocial and spiritual aspects of care. As healthcare systems evolve, understanding how these two areas can collaborate effectively is crucial for optimizing patient-centered approaches and ensuring comprehensive support for individuals and families.
Advancements in this field highlight the importance of shared decision-making and advanced care planning as mechanisms to enhance communication between healthcare providers and patients. By fostering a collaborative environment, we can empower patients to express their preferences and values concerning their care journey, particularly in the context of end-of-life decisions. Research has shown that integrated approaches lead to better symptom management, reduced hospitalizations, and increased patient and family satisfaction. Ongoing research could transform how we think about and deliver care for patients with serious illnesses.
In this Collection, we welcome submissions that span a wide array of topics, including but not limited to:
- Integrating advanced care planning in primary care
- Shared decision-making in end-of-life care
- Models of palliative care in primary care settings
- Enhancing communication between care teams
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer-review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Jun 08, 2026
Indigenous health and well-being
BMC Primary Care is calling for submissions to our Collection, Indigenous health and well-being. Historically, Indigenous communities have faced significant health disparities driven by systemic inequalities, cultural disconnection, and barriers to accessing healthcare. This Collection seeks to address these issues by gathering research that highlights the unique health challenges faced by Indigenous peoples, including chronic diseases, mental health issues, and the impact of social determinants on health outcomes. By amplifying Indigenous voices and perspectives, we aim to foster a deeper understanding of their health needs and aspirations.
The significance of researching Indigenous health lies in its potential to inform and transform healthcare practices, policies, and systems to achieve health equity. As research grows, we anticipate developments in the field of Indigenous health that may lead to the co-creation of innovative healthcare models. By fostering collaborations between Indigenous communities and healthcare providers, there is potential for enhanced accessibility, culturally appropriate care, and the development of policies that prioritize Indigenous health and well-being. Future studies may also uncover new insights into the role of traditional practices in modern healthcare systems, ultimately bridging the gap between Western medicine and Indigenous healing practices.
In this Collection, we welcome submissions that span a wide array of topics, including but not limited to:
- Barriers to healthcare access for Indigenous populations
- Community health initiatives in Indigenous communities
- Health equity strategies for Indigenous well-being
- Cultural competency in Indigenous healthcare
This Collection supports and amplifies research related to SDG 3: Good Health and Well-being and SDG 10: Reduced Inequalities.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Aug 05, 2026





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in