Using Mind Mapping in Research Methods to Achieve Impactful Outcomes
Published in Social Sciences, Microbiology, and Sustainability

I am Dr. Rasha Abdelsalam Elshenawy, a clinical pharmacist with 20 years of experience and pursuing my PhD in Antimicrobial Stewardship at the University of Hertfordshire in the UK. I held an American Board of Pharmacy certification and am recognised as a global lead in Antimicrobial Stewardship (AMS). My career is dedicated to optimising medicine use, ensuring patient safety, and combating antimicrobial resistance (AMR).
Educating healthcare professionals on best practices through maintaining effective teaching, learning, and research methodology enhances my capacity to lead effectively. My lifelong mission is to mitigate the global burden of AMR, fostering improvements in antibiotic prescribing practices and enhancing public health education. This commitment to global health advancements motivates me to pursue innovative solutions to AMR worldwide.
Using Mind Mapping in Research Method
In my research project investigating antimicrobial use during the COVID-19 pandemic, I initially utilised the 'MindMap' to arrange my mindset before conducting my research methodology. This helped me to be organised with a structured mindset, pursuing my belief in 'Begin With the End in Mind'.
The transformative role of mind mapping in revolutionising research strategy and execution was pivotal in a study on 'Start Smart, Then Focus' antimicrobial stewardship at an NHS Foundation Trust during the COVID-19 pandemic.
By organising complex data and simplifying the research process, mind mapping significantly aided in addressing the implementation of antimicrobial stewardship throughout the medication use process, from antibiotic prescribing to transcribing, dispensing, administering, and monitoring.
It also facilitated the development of stewardship intervention strategies and metrics to measure the outcomes of stewardship implementation, essential in tackling the challenges of antimicrobial resistance during a global health crisis, and identify antibiotic trends during the pandemic according to the World Health Organisation, AWaRe classification.
This approach was crucial in achieving meaningful research outcomes and offers a valuable model for future healthcare studies.
Introduction to Mind Mapping
Mind mapping is a visual organisation technique that helps represent ideas around a central theme in a non-linear graphical format. This approach is invaluable in research for brainstorming, structuring projects, and organising complex information, facilitating clearer understanding and systematic thinking.
It's particularly effective in disciplines requiring extensive planning and analysis, aiding in hypothesis generation, study design, and interpretation of results. By visually connecting disparate data points, mind mapping enhances creativity and focus, accelerating the research process and leading to more coherent and impactful outcomes. Its application spans various fields, making it a versatile tool in academic and professional research settings.
The Role of Mind Mapping in Enhancing Research Strategy
Mind mapping plays a crucial role in enhancing research strategies by facilitating the organisation of complex data through visual representation. This method allows researchers to clearly see relationships and hierarchies between different pieces of information, making it easier to generate new ideas and identify gaps in data.
Utilising mind mapping in planning and executing research not only improves the clarity and efficiency of the research process but also enhances problem-solving abilities. It encourages a more organised approach to both qualitative and quantitative data, ensuring that researchers can address research questions more comprehensively. This leads to more thorough preparation and impactful research outcomes.
Case Study from my Research Project
Using Mind Mapping to Achieve Impact in Antibiotic Research
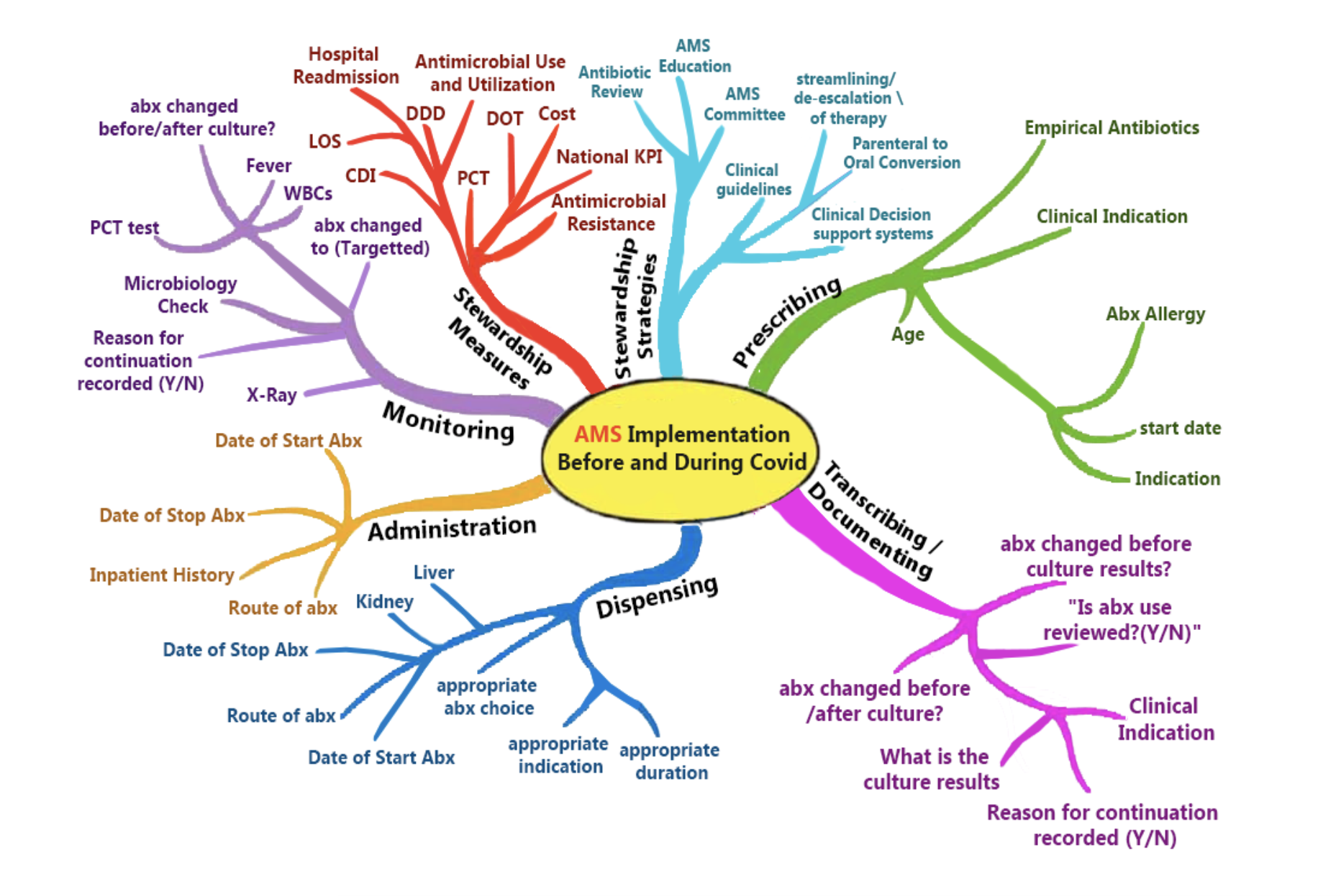 Figure 1. Using Mind Mapping in Research Method
Figure 1. Using Mind Mapping in Research Method
(Image Credit to Rasha Abdelsalam Elshenawy), published at MDPI COVID Journal.
In the exploration of the impact of COVID-19 on 'Start Smart, Then Focus' antimicrobial stewardship at an NHS Foundation Trust, the integration of mind mapping emerged as a quintessentially British innovation, fundamentally reshaping the research approach. Its transformative influence streamlined the research strategy and execution, enabling a comprehensive investigation into antimicrobial stewardship amidst the trials posed by the pandemic.
A notable instance of mind mapping's application was its role in organizing data extraction for antimicrobial stewardship, exemplified in Figure 1. By visually structuring intricate information, researchers adeptly categorized and synthesised data concerning antibiotic prescribing, transcribing, dispensing, administering, and monitoring. This facilitated a proper understanding of stewardship practices, vital for designing efficacious intervention strategies.
Additionally, mind mapping fostered collaboration amongst researchers, clinicians, and policymakers, ensuring a holistic approach to antimicrobial stewardship. It facilitated fruitful brainstorming sessions, enabling the generation of innovative ideas to optimise stewardship practices during the pandemic's challenges.
Furthermore, mind mapping played a pivotal role in developing metrics to evaluate the outcomes of stewardship interventions. By visualising key performance indicators and outcomes, researchers could assess the effectiveness of stewardship initiatives in mitigating antimicrobial resistance.
The integration of mind mapping in the research process proved instrumental in navigating the complexities of antimicrobial stewardship during the COVID-19 pandemic, offering invaluable insights for future healthcare studies.
Improving Data Collection and Analysis Through Mind Mapping
Mind mapping significantly enhances data collection and analysis, spanning from prescription to the monitoring of antibiotic usage. It simplifies complex information visually, improving comprehension and productivity.
In the prescribing phase, it categorises antibiotics and patient demographics, aiding targeted stewardship interventions. During monitoring, it charts patient responses and adverse effects, facilitating treatment adjustments.
Furthermore, mind mapping encourages collaboration among stakeholders, fostering the development of effective intervention strategies. By visually representing key performance indicators and outcomes, it facilitates the creation of metrics for stewardship implementation.
This approach enhances decision-making and optimises antimicrobial stewardship, crucial during global health crises like COVID-19.
Impact on Antimicrobial Resistance (AMR) Research
Mind mapping demonstrates remarkable efficacy in addressing challenges posed by Antimicrobial Resistance (AMR) amid global health crises. It aids in comprehensively understanding AMR dynamics, visualising complex data on antibiotic usage patterns, and contributing to targeted interventions.
By fostering collaboration, it enables interdisciplinary efforts towards developing innovative solutions. Mind mapping's visual representation of research findings enhances communication and facilitates evidence-based decision-making.
Additionally, it assists in identifying gaps in knowledge and areas requiring further investigation, guiding future research directions. Mind mapping significantly contributes to achieving meaningful research outcomes in AMR studies, offering a structured approach to address critical issues in antibiotic resistance during times of crisis.
Conclusion
In conclusion, the potential for mind mapping in healthcare research extends beyond antimicrobial stewardship, offering broader applications in various healthcare and public health domains. From disease management to health policy analysis, its versatile nature can revolutionise how we tackle complex challenges and achieve impactful research.
By fostering interdisciplinary collaboration and creative problem-solving, mind mapping cultivates a culture of innovative research methodologies, encouraging researchers to explore new and innovative approaches. Embracing mind mapping across healthcare disciplines holds promise for driving more impactful, effective, and evidence-based solutions to achieve the required research objectives and answer research questions properly, ultimately improving healthcare practices and outcomes for all upcoming research projects. Utilising mind maps in antibiotic research ensures proper antibiotic optimisation, enhances quality and patient safety, saves patient lives, and combats antimicrobial resistance globally.
Follow the Topic
What are SDG Topics?
An introduction to Sustainable Development Goals (SDGs) Topics and their role in highlighting sustainable development research.
Continue reading announcement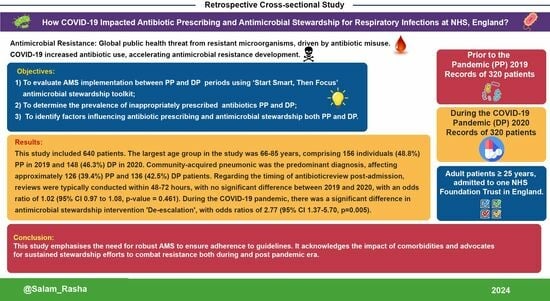





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in