Biting the Bloodsuckers Back: Turning Human Blood into Mosquito Poison
Published in Cell & Molecular Biology and Zoology & Veterinary Science
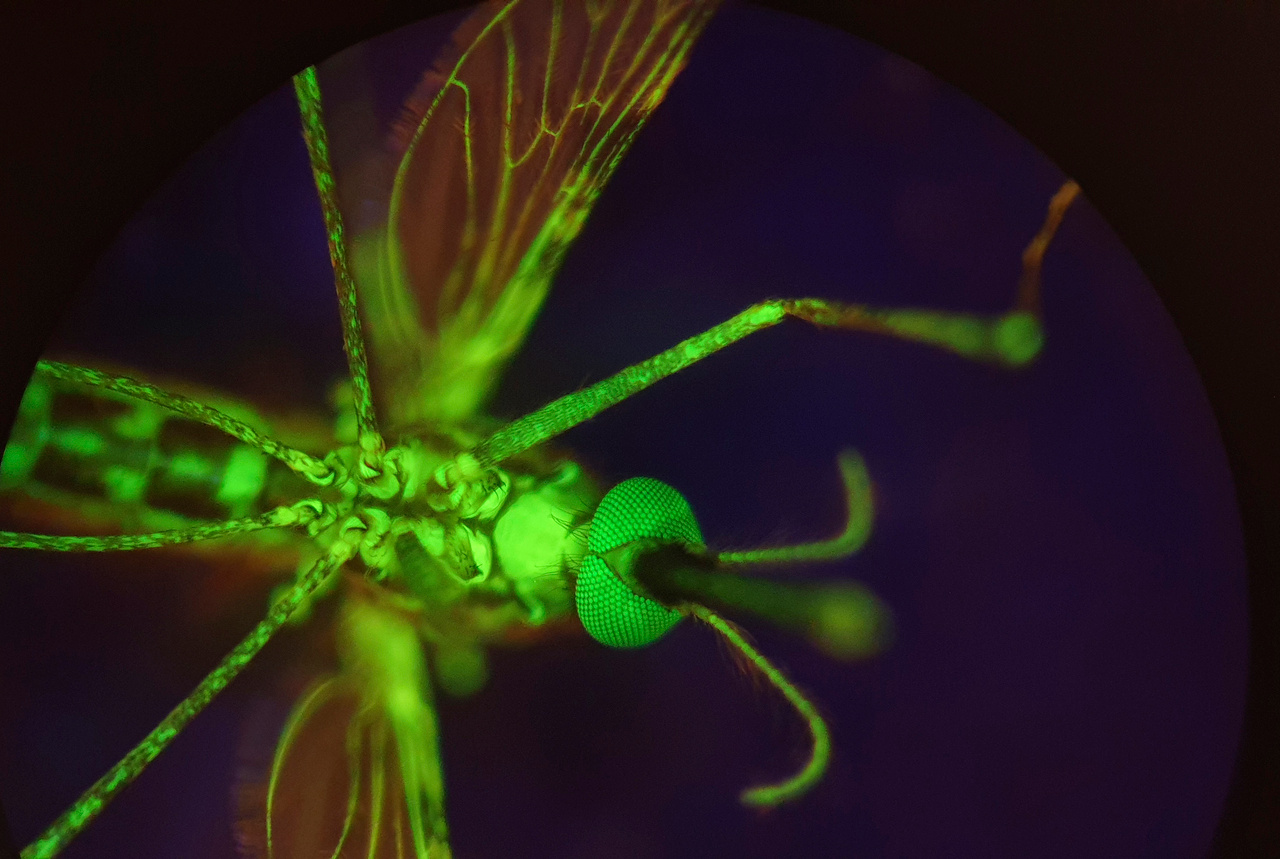
In the photograph above, a female An. gambiae mosquito appears to glow an eerie green—a result of a specialized diet containing fluorescein. When illuminated by ultraviolet light, this chemical compound transforms the mosquito's internal landscape, revealing the intricate network of its haemolymph system in luminescent detail. 📷 Photograph by Lee Haines.
The idea of ingesting a substance that turns your blood into poison for bloodsuckers intent on devouring your blood resembles the plot from a fantasy novel – in fact it sounds like the world of The Witcher where professional monster-slayers chug a potion that turns their blood deadly to blood-guzzling monsters that try to bite them. However, research by Haines et al. suggests that the idea may not be as fantastical as it sounds.
Playing an Uno reverse card against bloodsucking arthropods (insects and ticks) wouldn’t just be good for petty revenge; these creatures transmit deadly pathogens like malaria, which caused an estimated 597,000 deaths worldwide in 2023. Malaria transmission occurs when a female Anopheles mosquito feeds on the blood of an infected host, acquiring Plasmodium parasites in the process; after an incubation period of 1 - 2 weeks in the mosquito stomach, the parasites migrate to her salivary glands. When she bites her next victim, she gifts them the disease. While fighting this disease, we’re faced with many obstacles such as parasite resistance to antimalarial drugs, or mosquito resistance to insecticides. It’s clear we need more tools in our arsenal to combat malaria.
The sporozoite stage of the malaria parasite. 📷 Image Credit: Ute Frevert; false color by Margaret Shear
The idea of an endectocide (a drug effective against both internal and external parasites) isn’t new. They are typically administered to people and animals to rid them of parasites like worms. Several decades ago, researchers discovered that endectocides could disseminate through the bloodstream, making it poisonous to hungry mosquitoes. Ivermectin, for example, is a broad-spectrum antiparasitic drug on the World Health Organization’s list of essential medicines, administered large-scale to treat diseases like lymphatic filariasis and onchocerciasis. Ivermectin was also proven to make the blood of those taking it lethal to dining mosquitoes. It is safely administered to millions; however, children and pregnant people can’t take it, and its wide use makes resistance a concern. It is also environmentally toxic, harming other arthropods and bioaccumulating in earthworms. Even dung beetles can perish when encountering treated-cattle faeces. Consequently, the quest to find complementary alternatives is on.
Enter nitisinone.
Nitisinone
Our candidate drug is nitisinone: an inhibitor of the enzyme 4-hydroxyphenylpyruvate dioxygenase (HPPD): part of the metabolic pathway that breaks down the amino acid tyrosine. People with the rare disorders tyrosinemia type I and alkaptonuria are prescribed nitisinone to help manage their wonky tyrosine metabolic pathway, which leads to the accumulation of nasty byproducts causing debilitation. Research suggests nitisinone isn’t just helpful in treating rare metabolic conditions; it appears to have the interesting side effect of making your blood toxic to vectors like ticks, kissing bugs, tsetse flies, bed bugs and mosquitoes. This lethal bonus is due to a jamming of the essential tyrosine pathway, specifically the HPPD enzyme in bloodsucking arthropods, which creates a lethal buildup of tyrosine. Haines and colleagues posed two critical questions: how does nitisinone compare to the gold-standard ivermectin, and how effective is it against insecticide-resistant and older, malaria-transmitting mosquitoes?
Nitisinone vs Ivermectin
To compare the mosquito-slaying performance of nitisinone versus ivermectin, An. gambiae mosquitoes were fed blood containing either nitisinone or ivermectin and their mortality rates were recorded over two weeks - roughly how long it takes for a mosquito infected with Plasmodium parasites to become infective to humans. These mosquitoes were fed blood containing levels of nitisinone predicted to be circulating in the body at 7, 14, 21, and 28 days after you ingest a standard, safe dose of the drug. The international team found that mosquitoes fed nitisinone-infused blood, at predicted concentrations on days 7 and 14 after ingestion, died within 24 hours. Ivermectin didn’t fare as well; the mosquitoes survived 3.5 days for the concentration at 7 days and 8 days for the concentration at 14 days. Nitisinone also hung around in the blood longer than ivermectin due to its longer half-life of 54 hours versus ivermectin’s 18 hours.
Nitisinone vs Insecticide-Resistant Mosquitoes
The researchers were also curious whether nitisinone could take out insecticide-resistant An. gambiae mosquitoes and to their delight, discovered no significant difference between mortality rates when compared to insecticide-susceptible strains! Both strains survived less than a day when fed nitisinone. This exciting comparison highlights how nitisinone could be the only weapon against field mosquitoes with high background resistance to many insecticides, making them tough to control.
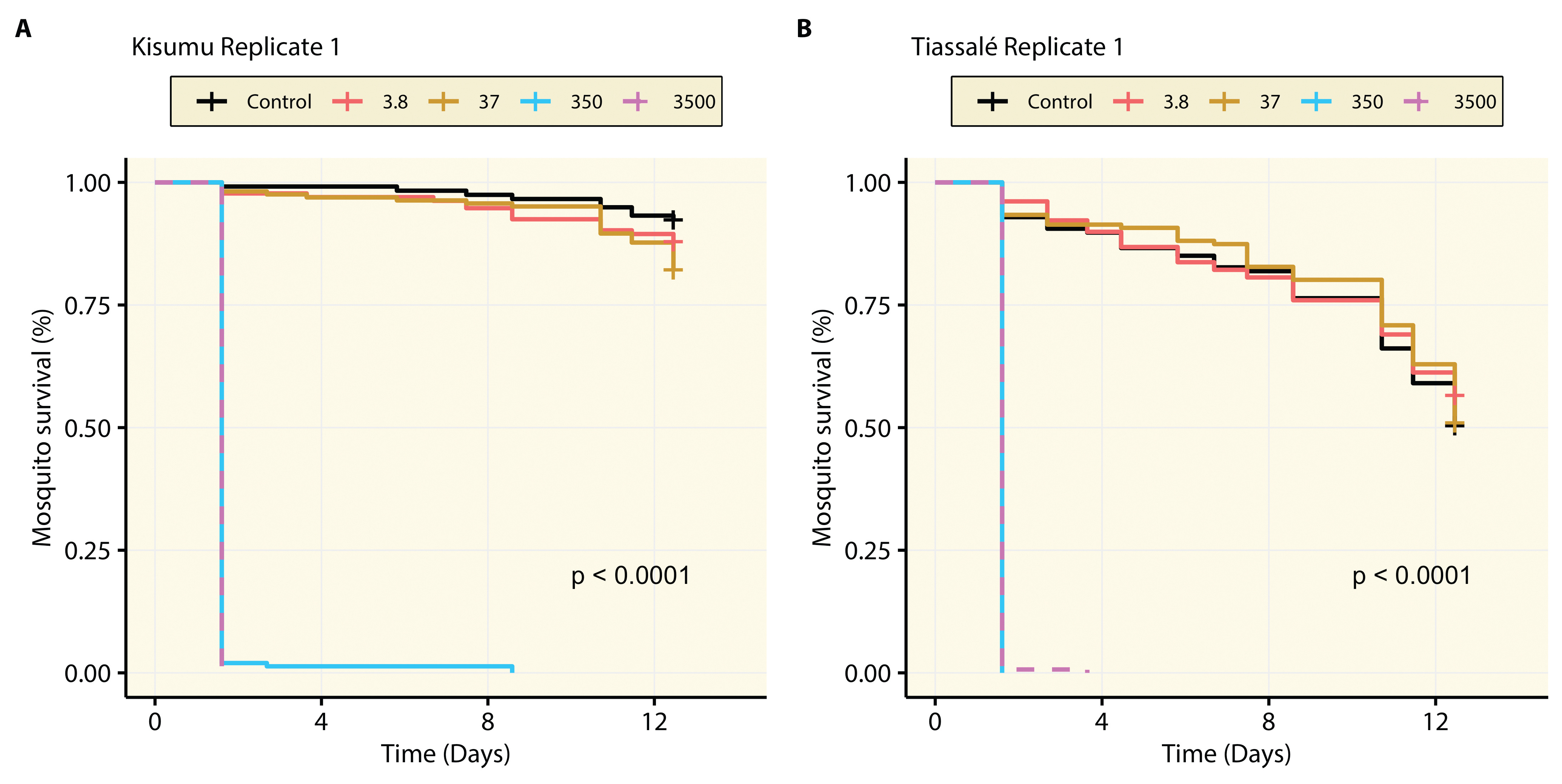
The survival rates of an insecticide-susceptible mosquito strain (Kisumu) and insecticide-resistant strain (Tiassalé) after being fed blood containing nitisinone 14 days after ingestion. They were fed concentrations (in nanograms per millilitre) with some being fed pure blood as a control. This figure shows just one of three replicates. Source: Haines et al.
Blood donated by people taking nitisinone
To drive home the point that taking a small, baby-aspirin-sized dose of nitisinone could still produce mosquitocidal blood, blood samples were donated by three people with alkaptonuria who had been taking 2 mg of nitisinone daily for years. This freshly drawn blood was fed to An. gambiae mosquitoes and killed them within just 12 hours. It was truly a Witcher’s black blood poison! The second person, with the highest blood concentration of nitisinone, had blood lethal to mosquitoes even when diluted five times. A fourth person who had alkaptonuria, but had not yet started nitisinone treatment, donated their blood as a control. This nitisinone-free blood did not harm the mosquitoes, meaning metabolites associated with having alkaptonuria were not mosquitocidal. The previous mosquitoes had died specifically from the nitisinone alone.
In summary, these results show the advantages of developing nitisinone as a new malaria control tool. It not only kills mosquitoes within a short period of time, it’s also effective against those resistant to insecticide-based control methods. Furthermore, a less obvious advantage is that repurposing nitisinone as a mosquitocidal drug (besides a treatment for rare metabolic diseases), could lead to reduced patient costs as increased demand drives greater availability. So, while we might not have people walking around as nitisinone-laced revenge piñatas for mosquitoes any time soon, a future may exist where mosquitoes fear biting us rather than the other way around…
About the author
Kate Moran has an MSc in Tropical Disease Biology from the Liverpool School of Tropical Medicine. She is often found typing instructions into a computer to electrocute pieces of silicon in a specific pattern to solve problems for humans. During her free time, she wonders how she can use her ability to tackle software bugs to help combat vector-borne diseases.
Follow the Topic
-
BugBitten

A blog for the parasitology and vector biology community.




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in