Conditional reprogramming: Modeling urological cancer and translation to clinics
Published in Cancer
Explore the Research
Just a moment...
onlinelibrary.wiley.com needs to review the security of your connection before proceeding.
Urological cancers, including those of the prostate, bladder, and kidneys, are a major health concern. In the United States alone, over 351,000 new cases and more than 67,000 deaths are expected in 2020 [1]. Prostate cancer remains the most common cancer among men in the U.S. There's a significant need for advanced methods to study these cancers and improve treatment outcomes, which remains a key goal for researchers globally.
One of the biggest challenges in cancer research is the limited number of effective models to study the disease. Traditional cell lines used for this purpose often fail to capture the complexity of actual tumors, with only a 1-10% success rate in creating these lines. Similarly, animal models, while useful, do not always mimic human responses, making it hard to translate findings into treatments for people.
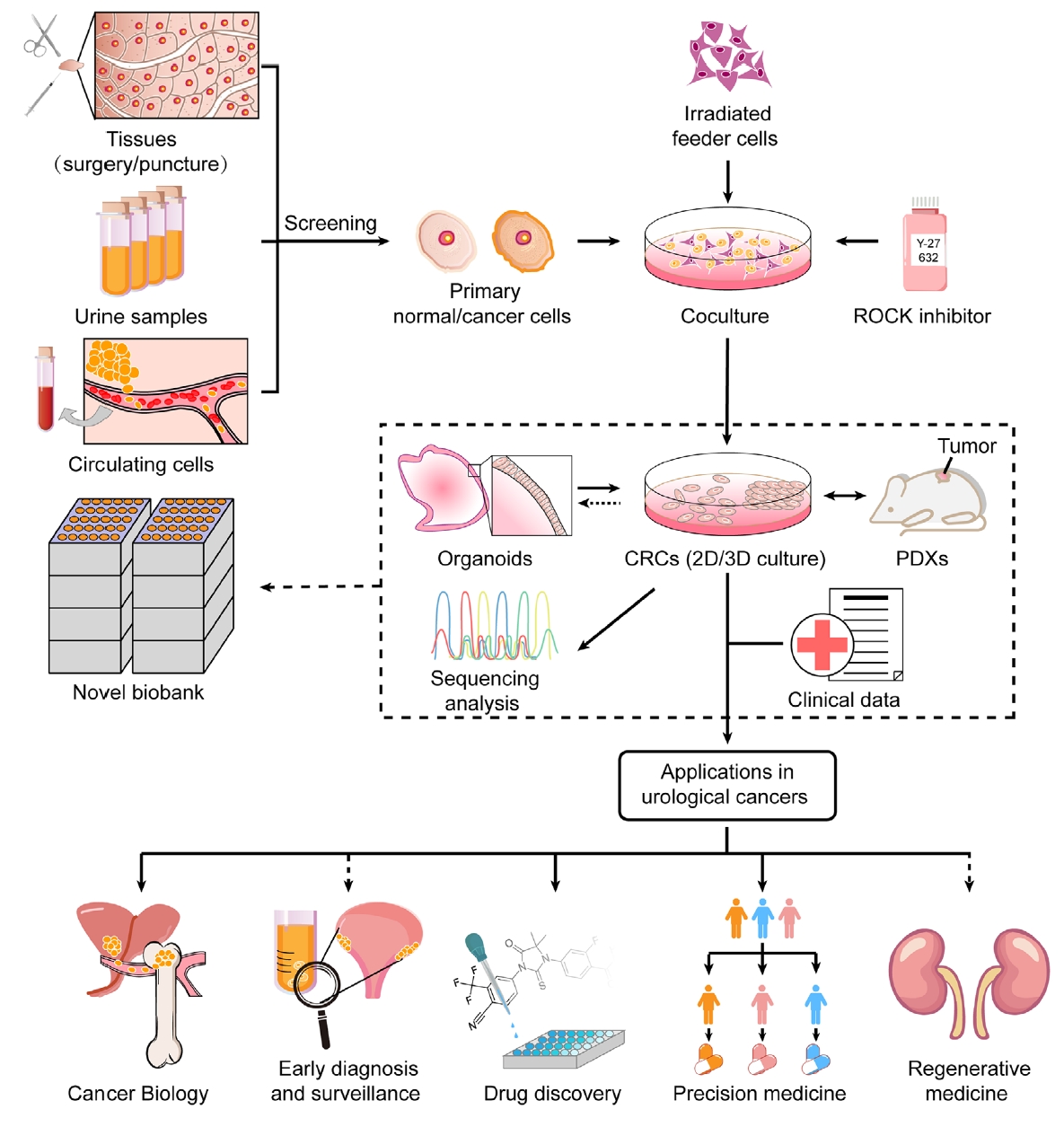
Recent advancements in biotechnology have led to the development of patient-derived models (PDMs), such as organoids, induced pluripotent stem cells (iPSCs), patient-derived xenografts (PDXs), and conditionally reprogrammed cells (CRCs) [2]. These models maintain the genetic characteristics of the original tumors and are increasingly used in cancer research. They are crucial for developing personalized treatments and understanding cancer better.
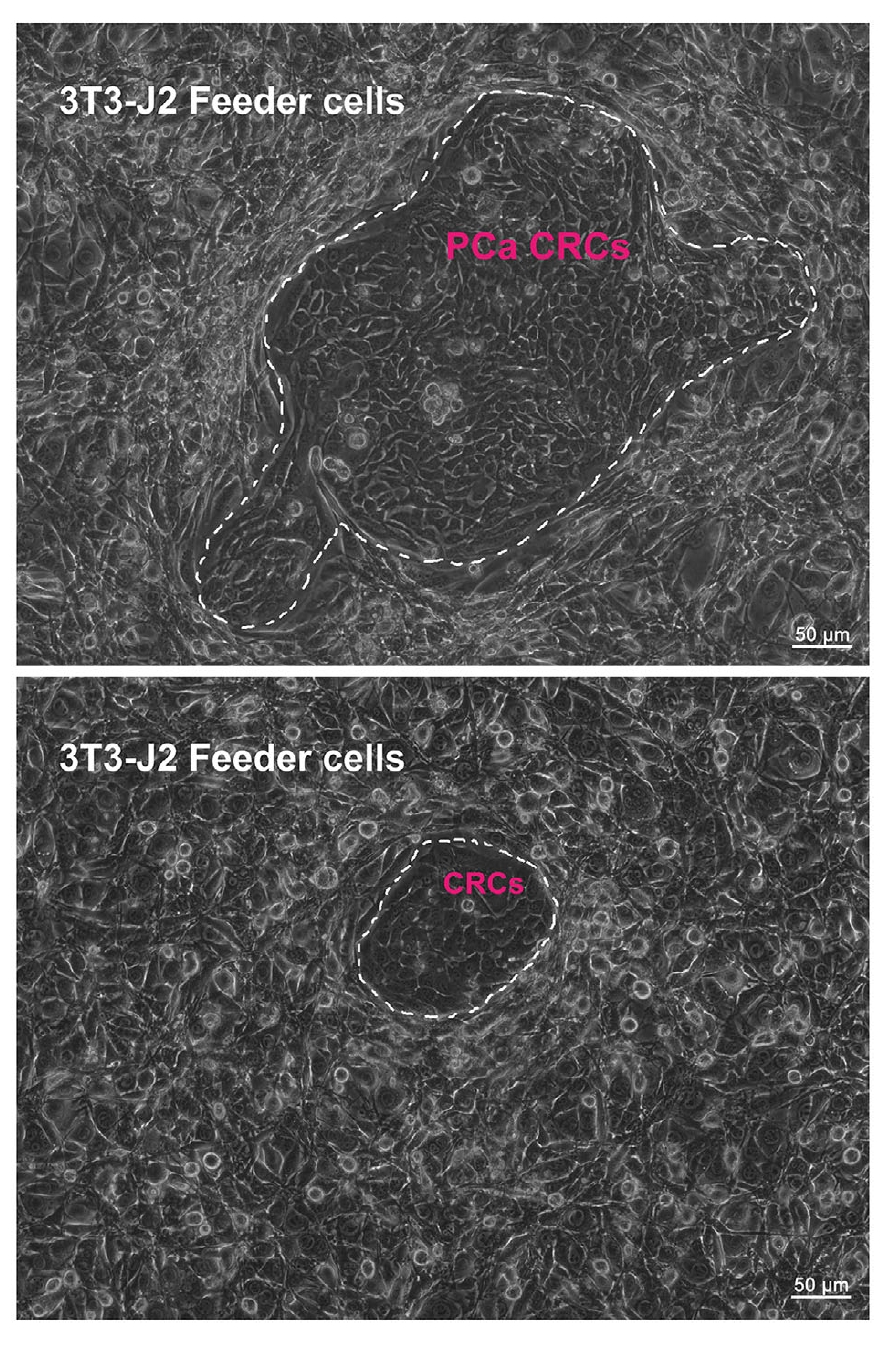
One breakthrough technique in this area is conditional reprogramming (CR). CR allows for the rapid creation of large numbers of human cells that closely represent the diversity of cells in actual tumors. This method does not require genetic modification, making it a powerful tool for studying cancer biology, testing drugs, and developing personalized therapies [3].
Overall, CR and other patient-derived models are transforming how we approach urological cancer research, offering new ways to study the disease, develop drugs, and create more effective treatments. These advancements hold promise for better understanding and managing urological cancers, potentially leading to improved patient outcomes.
References
[1] Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7-30.
[2] Liu X, Krawczyk E, Suprynowicz FA, et al. Conditional reprogramming and long-term expansion of normal and tumor cells from human biospecimens. Nat Protoc. 2017;12:439-451.
[3] Qian K, Wang G, Ju L, et al. A novel germline EGFR variant p.R831H causes predisposition to familial CDK12-mutant prostate cancer with tandem duplicator phenotype. Oncogene. 2020; 39(44):6871-6878.
Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in