Fortifying gastric defences against Helicobacter pylori
Published in Microbiology

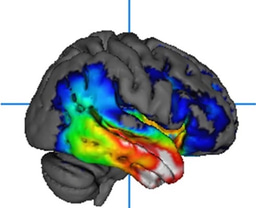
Helicobacter pylori (H. pylori) is a gram-negative, spiral-shaped bacterium spread by the oral route that colonises the stomach of approximately half the global population. In infected individuals, the bacteria reside in the mucus of the stomach and in the duodenum, mainly leading to asymptomatic chronic gastritis but the infection can lead to peptic ulcers and the bacterium is an identified risk factor for gastric cancer development. The exact nature of protective immunity against H. pylori has not been fully resolved but cell mediated immunity, particularly Th1 and Th17 responses are thought to be important for protection in animal models and these cells are found in the gastric mucosa and peripheral blood of infected individuals. Despite significant efforts, no H. pylori vaccine has yet been developed for clinical use. Given the site of colonisation and importance of mucosal responses for protection, an effective oral vaccine would in principle be the best means of preventing infection. However, developing non-living oral vaccines is a daunting challenge in part due to the lack of safe and effective vaccine adjuvants. Our group at Trinity College Dublin had been working with Dr Ivan Coulter and his team, then at Sigmoid Pharma on a new capsule based approach for oral vaccination. After screening a panel of potential adjuvants we had found that the invariant natural killer T (NKT) cell activator, alpha-galactosylceramide (alpha-GalCer) was a particularly effective oral adjuvant for killed bacterial antigens. We were collaborating with the oral vaccine pioneer Prof Jan Holmgren at the University of Gothenburg on another project at the time and following a chat over a glass of red wine we planned to work together on an oral H. pylori vaccine, incorporating his formalin-inactivated H. pylori whole cell preparation as antigen (once we secured funding from the European Union for the project Helicovaxor). This led to an exciting 5 years of collaboration looking into the potential of this vaccine to trigger mucosal cellular immunity and protection against gastric infection with H. pylori in mice. Through the work of a number of excellent researchers, including the lead author Dr Stephanie Longet at Trinity and the team in Gothenburg, particularly Dr Sukanya Raghavan we established that this novel vaccine promoted protective cellular immunity and found that interferon gamma was pivotal. Furthermore, the antigen specific Th1 response induced by the vaccine depended on roles for IL-1 and IL-17 receptors. More work will be needed to fully resolve the roles for these pathways as while the IL-17 receptor was required there was no detectable vaccine induced Th17 response.
In summary, our results show that α-GalCer is a promising adjuvant for inclusion in an oral vaccine against H. pylori infection and further highlights the potential of oral vaccination against this pathogen.
Follow the Topic
-
npj Vaccines

A multidisciplinary journal that is dedicated to publishing the finest and high-quality research and development on human and veterinary vaccines.
Related Collections
With Collections, you can get published faster and increase your visibility.
Therapeutic HPV vaccines
Publishing Model: Open Access
Deadline: Jun 30, 2026
Lipid nanoparticle (LNP)-adjuvanted vaccines
Publishing Model: Open Access
Deadline: May 19, 2026




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in