‘HIV Vaccine Awareness Day 2025’ - Harnessing T Cells in the Fight Against HIV: Insights from the AELIX-003 Trial
Published in Bioengineering & Biotechnology, Biomedical Research, and General & Internal Medicine
Why is the research valuable?
HIV remains a major global health challenge. Antiretroviral therapy (ART) can suppress the virus but does not eliminate it from the body. This means people living with HIV (PLWH) must remain on lifelong treatment, which can be difficult, especially in low-resource settings. The search for a functional cure—defined as long-term control of the virus without ART—is a key goal and can inform strategies that could lead to complete elimination of the virus.
Therapeutic vaccines aim to train the immune system to better control the virus after treatment interruption. The HTI vaccine strategy focuses on stimulating T-cell responses against parts of the virus that are commonly targeted in people who naturally control HIV without medication. In the AELIX-003 study (NCT04364035), researchers explored whether combining HTI vaccines with vesatolimod (VES), a TLR7 agonist that boosts innate immunity, could improve post-treatment control. AELIX-003 was designed based on results from the preceding AELIX-002 trial testing HTI vaccines alone and studies in non-human primates combining T-cell vaccines with VES. The trial focused on individuals who began ART early within weeks after acquisition of HIV, as this group tends to have stronger immune responses and smaller HIV reservoirs. The study offers important insights into how immune-based strategies might be used to delay viral rebound and reduce dependence on lifelong ART.
What did the authors do?
AELIX-003 was a randomized, double-blind, placebo-controlled trial involving 50 cisgender men with HIV in Spain who had started ART early after HIV acquisition and maintained undetectable viral loads. Participants were assigned to receive either a combination of two HTI-based vaccines (ChAdOx1.HTI and MVA.HTI) plus VES, or a placebo. The vaccines were delivered over several months, and VES was given orally every two weeks for a total of ten doses.
Following this regimen, all participants paused their ART under close clinical monitoring in what is called an analytical treatment interruption (ATI), lasting up to 24 weeks. ART was to be resumed if certain safety thresholds were crossed, such as high viral load or reduced CD4 counts.
The combination treatment was well tolerated. Most side effects were mild to moderate, and included injection-site pain and flu-like symptoms. No serious adverse events related to the study drugs were reported.
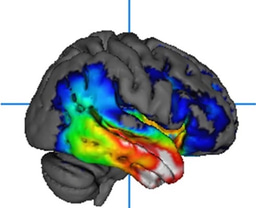
The key finding was that participants who received the active combination developed significantly stronger and broader T-cell responses against HIV than the placebo recipients. These responses were maintained during the vaccination period and were still elevated at the start of the ATI. While all participants eventually experienced viral rebound, those with stronger HTI-specific T-cell responses stayed off ART longer. By the end of the 24-week interruption, one-third of the treated group remained off ART, compared to one-quarter in the placebo group.
What are the implications of this study?
Although the intervention did not prevent viral rebound, it demonstrated that enhancing T-cell immunity through vaccination may help delay the return of detectable HIV after ART treatment is stopped. This was achieved with a simplified vaccine schedule than used in an earlier study, showing that strong immune responses are possible without highly complex vaccine regimens.
The study also supports the use of immune markers—such as T-cell response magnitude and HIV reservoir size—as predictors of treatment-free control. These markers could be used to guide future clinical trials or tailor treatment strategies.
Importantly, the intervention did not reduce the size of the HIV reservoir. This highlights the challenge of targeting long-lived latently infected cells and suggests that additional strategies may be needed, such as higher doses of VES or combining vaccines with other agents like broadly neutralizing antibodies (bNAbs).
Overall, AELIX-003 reinforces the idea that combination approaches—vaccines, immune modulators, and potentially bNAbs—may offer the best chance at achieving durable, ART-free viral control. Ongoing trials are already exploring these synergies, and this study helps lay the groundwork for future HIV cure strategies.



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in