Identification of novel immune biomarker in TNBC
Published in Cancer

Due to the lack of targetable receptors, chemotherapy is a current mainstay in the treatment of triple negative breast cancer (TNBC). The development of alternative therapeutics for TNBC is on the rise, many of which are immune-based strategies, due to their efficacy in immunogenic cancers, such as melanoma. Good patient outcomes in response to immune checkpoint inhibitors (ICIs) largely rely on an immune-reactive or ‘hot’ tumor microenvironment (TME). Unfortunately, the use of ICIs in TNBC has been met with limited success, likely due to their documented immune-poor TME. Better implementation of ICIs in breast cancer requires a more thorough understanding of the immune landscape in TNBC, as well as the development of predictive markers that will assist in the stratification of patients likely to respond to such agents.
Tumor infiltrating lymphocytes, which have been traditionally used to define a reactive TME, are known to correlate with improved outcomes in TNBC. Efforts to profile the immune landscape in breast cancer have ranged from histological analysis to single cell RNA-seq, in pursuit of predictive signatures. However, due to ill-defined thresholds and the requirement of multiple platforms to truly inform on the immune reactive state, no consensus has been reached regarding prognostic identifiers of disease progression or therapeutic response. Biomarkers ultimately need to be reliable, reproducible and easy to integrate into standard diagnostic procedures.
Herein we present a tumor inherent biomarker of favorable patient outcome and enhanced tumor immune reactivity. We have identified tumor inherent interferon regulatory factor 9 (IRF9) as a robust and reliable biomarker that is homogenous across tumor samples. IRF9 is a standard immunohistochemical marker with defined cut-offs for patient stratification based on simple H score. Tumor expression of IRF9 represents both the signaling status of the type I interferon (IFN) pathway, which drives immune activation, and the infiltration of tissue resident memory T cells, both of which have been identified as important for therapeutic response and long-term outcomes. Our study shows that patients with a loss of tumor inherent IRF9 are likely to rapidly succumb to metastasis and are unlikely to respond to chemotherapy and perhaps ICIs.
Our report highlights a way forward for the implementation of personalized medicine in TNBC (Figure 1). Our proposed model is that, upon diagnoses, patients should undergo a biopsy that allows for evaluation of tumor inherent IRF9 and tumor heat. This will allow for patient stratification based on the immune-reactive nature of their tumor and likelihood of response to conventional chemotherapy. This paper offers an opportunity to explore IRF9 as a treatment-guiding biomarker for chemotherapy and gives important information about patient outcomes. Its use in other malignancies may allow stratification of patients likely to respond to ICIs given the known link between response and an immune reactive TME. Furthermore our study highlights that restoration of tumor inherent type I IFN signaling increases tumor-immune reactivity and therapeutic response.
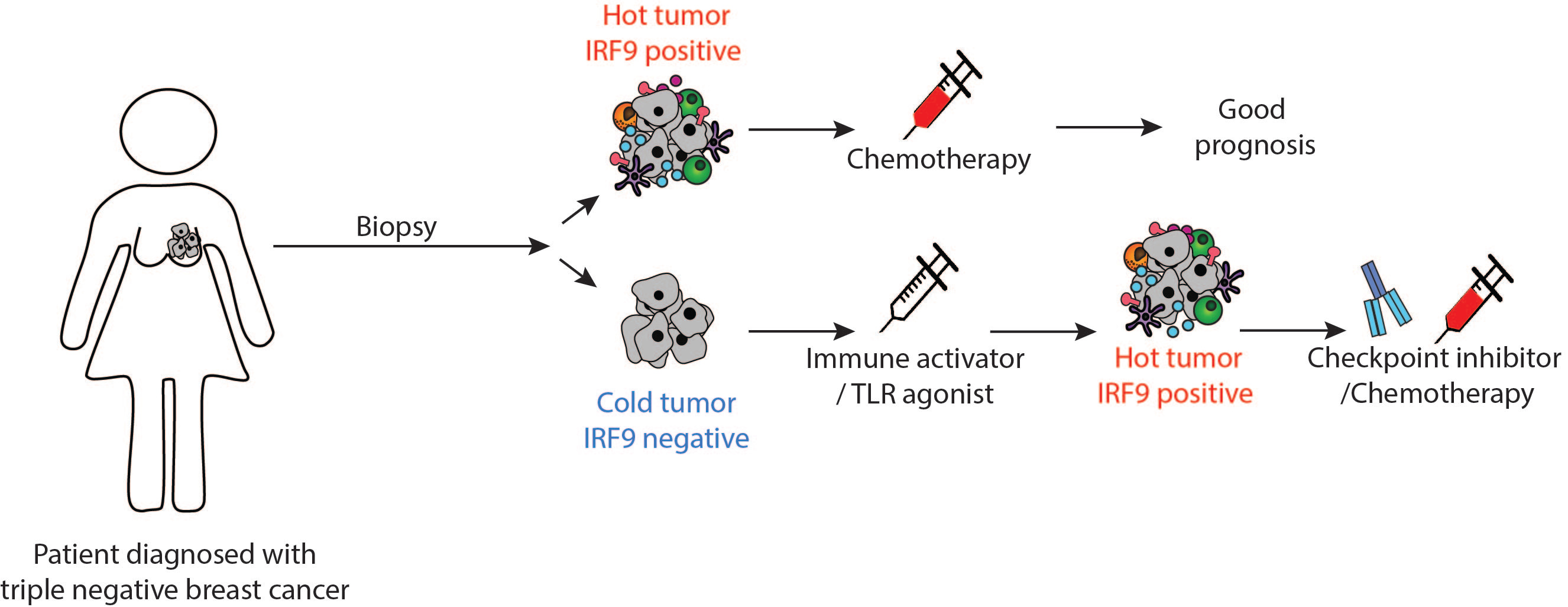
Figure 1: Personalized therapy in TNBC based on IRF9
Patients with IRF9 positive, hot tumors are likely to do well on chemotherapy and have a good prognosis. Patients with cold/IRF9 negative tumors will require additional treatment with an immune activator, such as a TLR agonist to induce IFN signaling, increasing IRF9 expression and immune infiltrate. This will then be followed by checkpoint inhibitors and/or chemotherapy dependent on cancer type.
The article can be found online here: https://rdcu.be/bPO1g
Follow the Topic
-
npj Precision Oncology

An international, peer-reviewed journal committed to publishing cutting-edge scientific research in all aspects of precision oncology from basic science to translational applications to clinical medicine.
Related Collections
With Collections, you can get published faster and increase your visibility.
Tumor-type-agnostic biomarkers and treatments in oncology
Publishing Model: Open Access
Deadline: Mar 05, 2026
Emerging adjuvant and neo-adjuvant treatment approaches in solid tumors
Publishing Model: Open Access
Deadline: Mar 30, 2026





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in