Obesity Day: Highlighting the Role of Perivascular Adipose Tissue in Vascular Health
Published in General & Internal Medicine
PVAT is not merely a structural layer surrounding blood vessels; it functions as an active endocrine organ that significantly influences vascular function, inflammation, and metabolic regulation. Growing evidence suggests that PVAT plays a fundamental role in the pathophysiology of obesity-related cardiovascular diseases, necessitating further research and clinical interventions.
The Cardiovascular-Endocrinology Connection
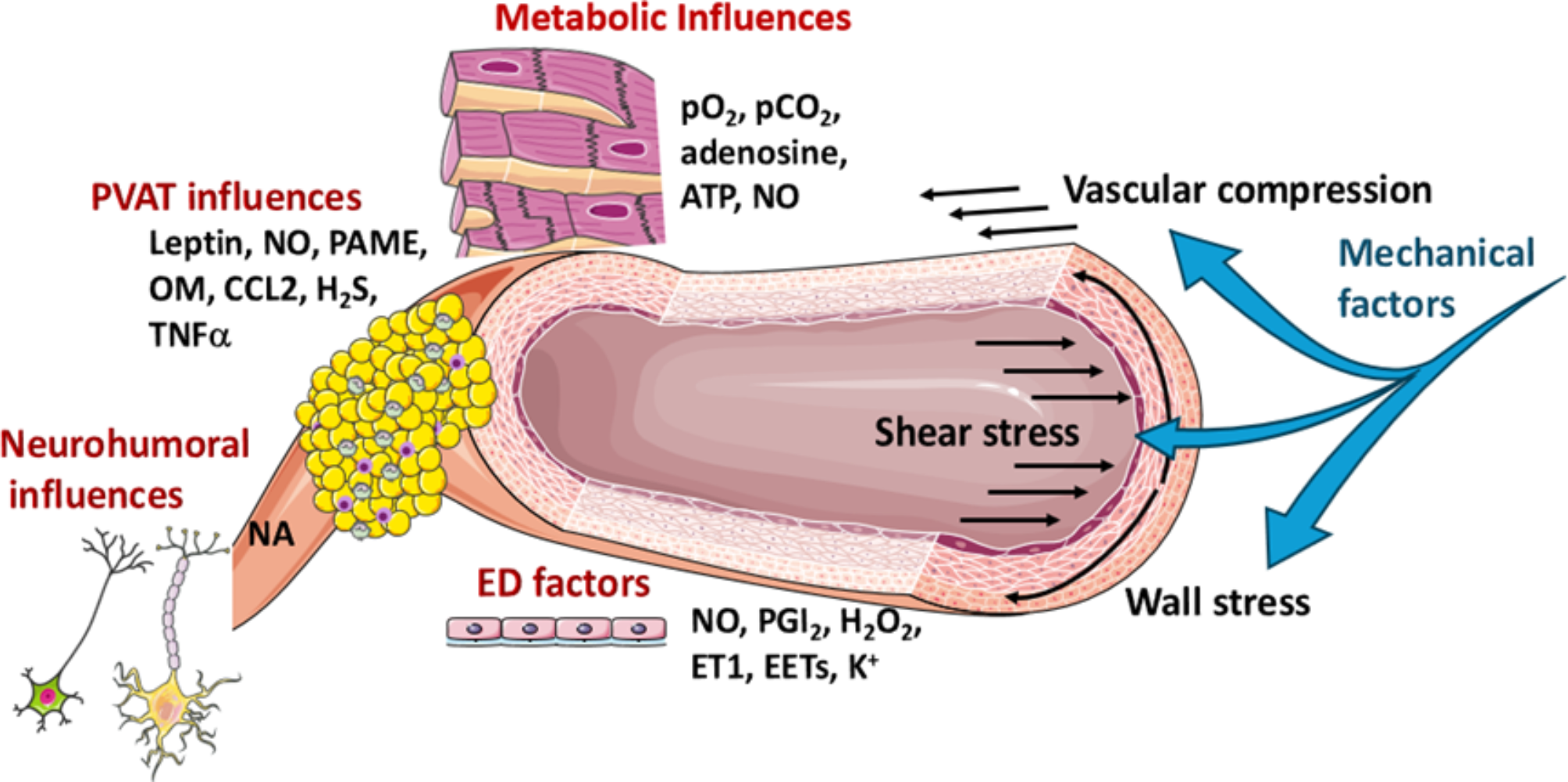
PVAT is a key player in the intersection of endocrinology and cardiovascular health. As an endocrine organ, PVAT secretes a variety of adipokines, including leptin, adiponectin, resistin, and visfatin, which modulate vascular homeostasis, immune responses, and metabolic balance. Dysfunctional PVAT, as seen in obesity, alters these secretions, leading to insulin resistance, increased sympathetic nervous system activity, and systemic inflammation—key drivers of cardiovascular disease. The bidirectional relationship between PVAT and metabolic dysfunction underscores the importance of integrating cardiovascular and endocrine approaches in research and clinical management.
The Significance of PVAT
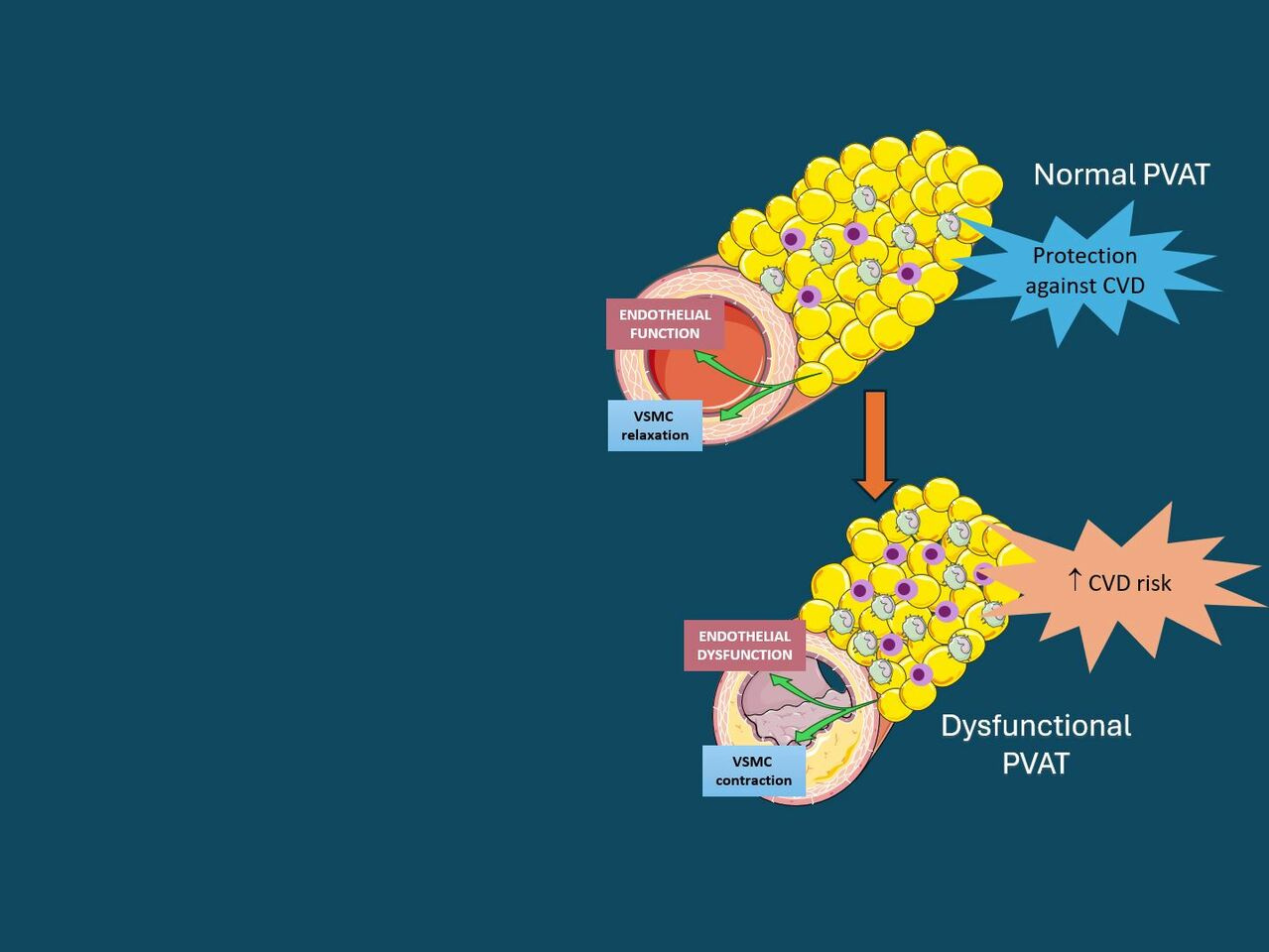
PVAT secretes bioactive molecules known as adipokines, which regulate vascular tone, immune responses, and inflammation. Under normal physiological conditions, PVAT provides protective effects by releasing anti-inflammatory and vasodilatory factors such as adiponectin and nitric oxide. However, in the presence of obesity, PVAT undergoes pathological changes that contribute to metabolic dysregulation and vascular dysfunction.
The Impact of Obesity on PVAT
Obesity induces PVAT dysfunction, resulting in: 1) Increased infiltration of immune cells, exacerbating vascular inflammation and immune system overactivation. 2) Dysregulated adipokine secretion, leading to a reduction in protective factors such as adiponectin and an increase in pro-inflammatory cytokines. 3) Endothelial dysfunction, contributing to the development of atherosclerosis, hypertension, and reduced vascular compliance. 4) Elevated oxidative stress and lipid imbalances, promoting insulin resistance, type 2 diabetes, and cardiovascular complications. 5) Increased perivascular fibrosis, which impairs normal vessel function and contributes to arterial stiffness and hypertension.
The Importance of Addressing PVAT Dysfunction
Given the rising prevalence of obesity worldwide, understanding PVAT’s role is crucial for developing strategies to combat obesity-related cardiovascular diseases. This issue extends beyond body mass index, emphasizing the impact of adipose tissue behavior on systemic health. Studies have demonstrated that PVAT dysfunction can serve as a biomarker for early cardiovascular disease detection, making it a potential target for preventive and therapeutic strategies.
Potential Interventions
- Lifestyle Modifications: Regular physical activity and a balanced diet have been shown to restore PVAT function, reduce inflammation, and improve metabolic health. Diets rich in omega-3 fatty acids, polyphenols, and fiber have been linked to improved adipose tissue homeostasis and reduced vascular inflammation.
- Pharmacological Strategies: Targeting inflammatory pathways with anti-inflammatory drugs, utilizing insulin-sensitizing agents, and developing novel metabolic therapies may offer promising outcomes in treating PVAT-related diseases. Emerging treatments such as sodium-glucose co-transporter-2 (SGLT-2) inhibitors and glucagon-like peptide 1 (GLP-1) receptor agonists show potential in mitigating PVAT dysfunction.
- Advancements in Research: Innovative imaging technologies, including magnetic resonance imaging, positron emission tomography/computed tomography scans, and Raman spectroscopy, are providing new insights into PVAT dynamics. These advancements facilitate early detection of PVAT-related vascular pathology and allow for the development of targeted interventions.
- Epigenetic and Molecular Research: Studies suggest that epigenetic modifications in PVAT adipocytes contribute to obesity-induced vascular dysfunction. Exploring these molecular pathways may open new avenues for gene-targeted therapies aimed at reversing adipose tissue dysfunction.
- Surgical and Interventional Approaches: Bariatric surgery has been shown to reduce PVAT mass and improve vascular function. Additionally, novel minimally invasive techniques are being investigated to modify or remove PVAT in patients with severe metabolic complications.
Conclusion
Obesity represents a systemic condition with profound effects on metabolism and vascular health. PVAT is increasingly recognized as a key factor in obesity-related cardiovascular diseases, necessitating further research and targeted interventions. On World Obesity Day 2025, we emphasize the need for interdisciplinary collaboration in developing innovative strategies for improving metabolic and cardiovascular health. Addressing PVAT dysfunction through lifestyle modifications, pharmacological treatments, and advanced imaging techniques may significantly reduce the burden of obesity-related diseases.
References
- Szasz T, Webb RC. Perivascular adipose tissue: more than just structural support. Clin Sci (Lond). 2012;122(1):1-12.
- Antoniades C, Tousoulis D, Vavlukis M, et al. Perivascular adipose tissue as a source of therapeutic targets and clinical biomarkers. Eur Heart J. 2023;44(38):3827-3844.
- Agabiti-Rosei C, Saxton SN, De Ciuceis C, et al. Influence of Perivascular Adipose Tissue on Microcirculation: A Link Between Hypertension and Obesity. Hypertension. 2024;81(1):24-33.
- Queiroz M, Sena CM. Perivascular adipose tissue: a central player in the triad of diabetes, obesity, and cardiovascular health. Cardiovasc Diabetol. 2024;23(1):455.
Follow the Topic
-
Cardiovascular Diabetology

This journal considers manuscripts on all aspects of the diabetes/cardiovascular interrelationship and the metabolic syndrome; this includes clinical, genetic, experimental, pharmacological, epidemiological and molecular biology research.
Your space to connect: The Nitric oxide signalling in cardiovascular health and disease Hub
A new Communities’ space to connect, collaborate, and explore research on Cardiovascular Physiology, Clinical Medicine, and Diseases!
Continue reading announcementRelated Collections
With Collections, you can get published faster and increase your visibility.
Organoids as emerging models in diabetes and cardiovascular research
Organoids—three-dimensional structures derived from stem cells—are transforming biomedical research by modeling key aspects of human physiology and disease. By replicating native tissue architecture, cellular heterogeneity, and functional behavior, they provide human-relevant systems that address limitations inherent to conventional in-vitro and animal models.
Diabetes and cardiovascular disease are deeply interconnected conditions, characterized by shared, multi-organ pathophysiology. Organoid technologies offer unique opportunities to dissect disease mechanisms, evaluate therapeutic strategies, and develop personalized, physiologically relevant models. These systems enable the investigation of cardiometabolic processes in platforms that better reflect the complexity and progression of human disease.
Cardiovascular Diabetology welcomes original research articles, reviews, and meta-analyses for this Collection, which aims to highlight the use of organoid technologies in advancing our understanding of cardiovascular complications associated with diabetes.
Areas of interest include, but are not limited to:
- Organoid models of diabetic cardiomyopathy and heart failure
- Matrigel alternatives for organoid development
- Cell-cell and extracellular matrix interactions in organoids
- Organoid-based drug testing for cardiovascular diseases
- Organoid-on-chip systems for tissue crosstalk and perfusion3D bioprinting and tissue engineering for cardiovascular organoids
- Artificial intelligence–driven analysis of organoid function and phenotypes
- Organoid models of gestational diabetes–induced congenital heart disease
- Functional genomics using CRISPR in cardiovascular organoids
- Single-cell and spatial omics to map disease states in organoids
- Co-culture systems of vascular and pancreatic organoids to study metabolic-vascular crosstalk
- Organoid-based screening platforms for anti-diabetic and cardioprotective drugs
Submissions that contribute to conceptual clarity (e.g., distinctions between organoids and spheroids), incorporate multi-organ or metabolic system perspectives, or connect technological development with clinical or translational insights are especially welcome.
This Collection supports and amplifies research related to SDG 3, Good Health and Well-Being.
All submissions in this collection undergo the journal’s standard peer review process. Similarly, all manuscripts authored by a Guest Editor(s) will be handled by the Editor-in-Chief. As an open access publication, this journal levies an article processing fee (details here). We recognize that many key stakeholders may not have access to such resources and are committed to supporting participation in this issue wherever resources are a barrier. For more information about what support may be available, please visit OA funding and support, or email OAfundingpolicy@springernature.com or the Editor-in-Chief.
Publishing Model: Open Access
Deadline: Jul 07, 2026
Cardiometabolic and Hepatic Interconnections: From Mechanisms to Clinical Implications
Cardiometabolic and liver diseases are no longer viewed as isolated entities. Growing evidence shows that hepatic and cardiovascular dysfunctions are tightly interconnected through shared metabolic, inflammatory, hemodynamic, and hormonal pathways. This crosstalk shapes disease trajectories and opens opportunities for integrated diagnostics and therapies.
Key interconnections include:
- Insulin resistance. The liver is pivotal for glucose and lipid homeostasis. Hepatic insulin resistance drives excess glucose production and dyslipidemia, contributing to the cardiovascular–kidney–metabolic (CKM) syndrome.
- Metabolic dysfunction–associated steatotic liver disease (MASLD). Highly prevalent in obesity and metabolic syndrome, and especially common in type 2 diabetes (T2D), which bears the highest MASLD burden. Progression to steatohepatitis or fibrosis markedly increases atherosclerotic risk.
- Liver-derived factors. Hepatokines (e.g., FGF21) and extracellular vesicles influence cardiac tissue, vascular tone, and systemic metabolism, potentially amplifying inflammation, oxidative stress, and lipotoxicity across organs.
- Systemic inflammation and lipotoxicity. Visceral adipose tissue and the liver release inflammatory cytokines and triglyceride-rich lipids, promoting endothelial dysfunction and perpetuating metabolic disturbances.
- Dyslipidemia. Elevated triglycerides and LDL, with reduced HDL, accelerate atherogenesis and cardiovascular risk.
- Hemodynamic and metabolic stress. Heart failure can cause hepatic congestion and hypoperfusion, while advanced liver disease can precipitate cirrhotic cardiomyopathy and arrhythmias, even in the absence of prior heart failure.
In summary, hepatic and cardiometabolic systems are functionally and pathologically intertwined: liver dysfunction worsens cardiovascular and metabolic health, and cardiometabolic disturbances accelerate hepatic pathology.
This Collection welcomes original research articles, reviews, and meta-analyses focused on this reciprocal relationship. Given the high prevalence of MASLD in T2D, we especially encourage submissions at the T2D–MASLD–cardiovascular interface. Addressing hepatic and cardiometabolic health in parallel is essential for effective risk reduction and patient care.
This Collection supports and amplifies research related to SDG 3, Good Health and Well-Being.
All submissions in this Collection undergo the journal’s standard peer review process. Similarly, all manuscripts authored by a Guest Editor(s) will be handled by the Editor-in-Chief. As an open access publication, this journal levies an article processing fee (details here). We recognize that many key stakeholders may not have access to such resources and are committed to supporting participation in this issue wherever resources are a barrier. For more information about what support may be available, please visit OA funding and support, or email OAfundingpolicy@springernature.com or the Editor-in-Chief.
Publishing Model: Open Access
Deadline: Jul 15, 2026
Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in
On World Obesity Day 2025, it's crucial to recognize the pivotal role of Perivascular Adipose Tissue (PVAT) in obesity-related cardiovascular diseases and its potential as a target for innovative interventions.