Perceptual deficits in the processing of emotional faces in insomnia
Published in Neuroscience

The role of facial expressions in making socio-emotional judgments
Considered a universal domain of human behaviour, emotions reveal how individuals may feel and subsequently behave, whilst also informing critical judgments related to decision making in a psychosocial context. Emotionally salient non-verbal cues (i.e., gestural, postural and facial) allow individuals to communicate their emotional state to other people. Likewise, reading such cues projected by others offers insight into their internal state. In this context, the human face may be considered the most prevalent source of social information. Accordingly, the ability to accurately judge facially expressed emotions remains fundamental for maintaining successful social interactions. According to Ekman, there are six main cross-culturally accepted facial expressions of emotion: fear, anger, disgust, happiness, sadness, and surprise.

Deficits in the ability to correctly interpret the emotional expressions of others may lead to negative psychosocial consequences. With that in mind, individuals experiencing psychiatric difficulties such as insomnia, anxiety, depression, bipolar disorder, psychosis, and schizophrenia typically present such deficits when empirically examined. Given the prevalence of psychiatric symptoms, advancing our understanding of deficits in face processing remains vital.
Insomnia, emotion perception, and the current data
Characterised by difficulties in sleep initiation, maintenance and/or early morning awakening, and accompanied by significant impairment to daytime functioning, insomnia is often related to deficits in emotion regulation and socioemotional functioning. However, only a handful of studies have examined the perception of emotional faces in the context of poor sleep and insomnia. Here, it appears that individuals with insomnia experience perceptual difficulties when observing facially expressed fear, anger, sadness, disgust and happiness and insomnia salient faces depicting tiredness.
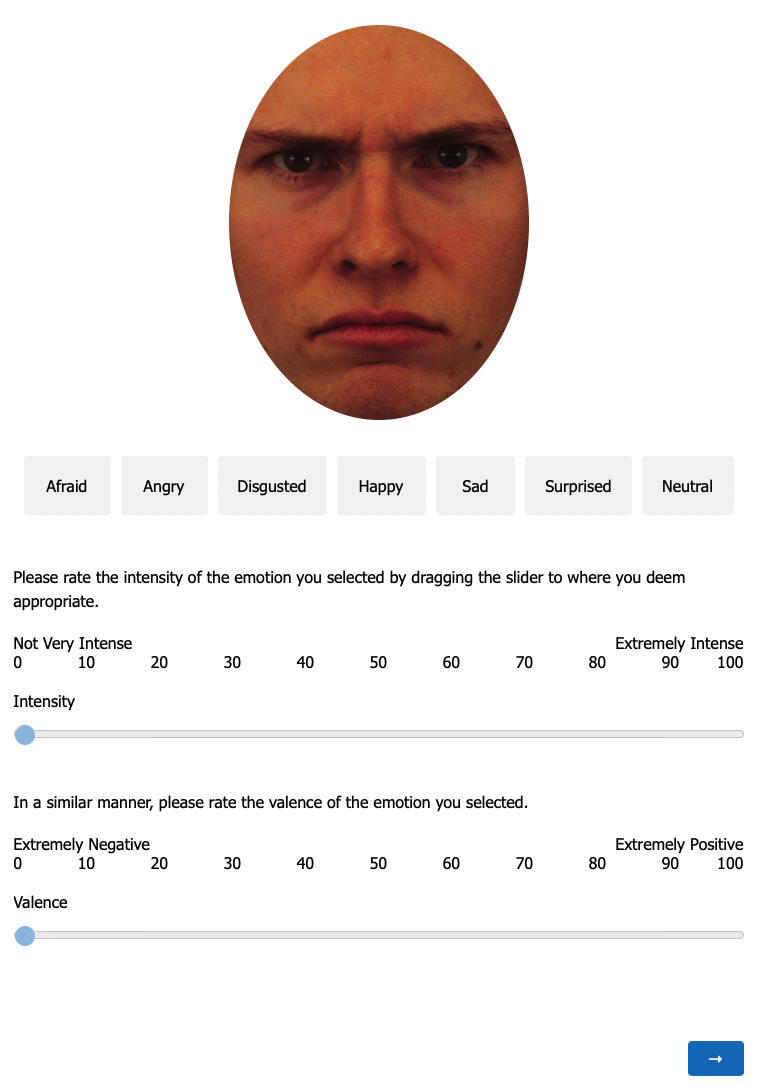
As a partial aim of the current dataset, we sought to provide additional data concerning the perception of emotional faces amongst individuals presenting symptoms of insomnia.To achieve this, N=572 respondents completed a psychometric measure of insomnia symptomatology after rating a series of fifty-six faces from an existing database. In particular, using six cross-cultural facial expressions of emotion, we examined:
- The categorisation accuracy (whether the displayed emotion was correctly identified).
- Misperception (which emotion an incorrect judgment was perceived to be).
- Intensity ratings (the strength of the emotion signal strength).
- Emotional valence ratings (the extent and direction of perceived affect in relation to intrinsic appeal or repulsion) six cross-cultural facial expressions of emotion.
What was found
- Symptoms of insomnia were related to increased intensity ratings of potentially threatening facial expressions depicting fear disgust and sadness. Interestingly, these expressions were not necessarily perceived as more or less positive or negative in terms of emotional valance.
- The outcomes also identified deficits in the ability to accurately identify fearful faces. This may possibly increase exposure to harmful situations due to an impaired ability to determine perceived threat in the faces of others which should otherwise facilitate an appropriate behavioural response.
- Increased reports of insomnia were related to the misinterpretation of fearful faces as displaying either anger or disgust. Here, facially expressed fear in others appears to be taken in a somewhat personal manner, where perceived hostility amongst those experiencing insomnia may tentatively translate into hostile and defensive behaviour towards others.
- Finally, neutral expressions were also perceived as either more threatening (displaying anger) or positive (displaying happiness). This possibly highlights an accentuation of bipolar deficits in the interpretation of an otherwise socially benign facial expression, which again may impair behavioural responses in social situations.
What may explain these deficits?
Insomnia may be associated with an interpretive bias when making emotional judgments based on the facial expression of other people. Here, similar to anxiety and depression, deficits in intensity and categorisation ratings may reflect cognitive and affective processes that contribute to the adaptation to difficult interpersonal situations. This may be explained by alterations in neural activity. Indeed, the amygdala plays a vital role in regulating behavioural responses to socially ambiguous signals. When compared to healthy subjects, imaging studies evidence those with insomnia to exhibit reduced amygdala connectivity with brain regions (striatum, insula, and thalamus) associated with the processing of emotion. When observing emotional disorder-congruent stimuli, those with insomnia display increased amygdala reactivity relative to controls. In healthy subjects, the extent of amygdala reactivity differs based on the facial emotional expression presented. Whereas increased amygdala reactivity is evidenced in those with insomnia in response to disorder-congruent stimuli (Baglioni et al., 2014). As such, alterations in face-processing presented by those with insomnia may be explained by deficits in amygdala reactivity, where the extent of such reactivity may also be influenced by the nature of the observed emotional expression. Moving forward, additional research is required to shed light on the relationship between face-processing and neural mechanisms in insomnia.
It is also relevant to note that individuals with insomnia present deficits in the self-perception of their own faces. In particular, those with insomnia display a propensity to rate their own face as more tired than they physically appear, while in comparison, this bias did not extend to the perception of other people's faces. Greater recognition of emotional expressions has previously been associated with the ability to imitate facial expressions. Considering the presence of a bias towards one's own and others' facial features based on eye-tracking data, a recent review postulates that individuals with insomnia might be less capable to correctly imitate others' expressions.
Concluding Remarks
Deficits in facial emotion processing are an important impairment in insomnia with significant consequences for social functioning and subjective well-being. Further research should explore the role of emotional faces to expand the current understanding of perceptual differences in face processing among individuals with insomnia when compared with normal sleepers, especially with a focus on eye-tracking and neural mechanisms.
Key References:
- Akram U, Stevenson J. Altered emotion perception in insomnia, anxiety, depression, mania, psychotic experiences and schizotypal symptoms: a dataset. Scientific Data. 2024 Sep 11;11(1):990.
- Huang Y, Du J, Guo X, Li Y, Wang H, Xu J, Xu S, Wang Y, Zhang R, Xiao L, Su T. Insomnia and impacts on facial expression recognition accuracy, intensity and speed: A meta-analysis. Journal of Psychiatric Research. 2023 Apr 1;160:248-57.
- Kyle SD, Beattie L, Spiegelhalder K, Rogers Z, Espie CA. Altered emotion perception in insomnia disorder. Sleep. 2014 Apr 1;37(4):775-83.
- Akram U, Sharman R, Newman A. Altered perception of facially expressed tiredness in insomnia. Perception. 2018 Jan;47(1):105-11.
- Zhang J, Chan AB, Lau EY, Hsiao JH. Individuals with insomnia misrecognize angry faces as fearful faces while missing the eyes: An eye-tracking study. Sleep. 2019 Feb;42(2):zsy220.
Follow the Topic
-
Scientific Data

A peer-reviewed, open-access journal for descriptions of datasets, and research that advances the sharing and reuse of scientific data.
Related Collections
With Collections, you can get published faster and increase your visibility.
Data for crop management
Publishing Model: Open Access
Deadline: Apr 17, 2026
Data to support drug discovery
Publishing Model: Open Access
Deadline: Apr 22, 2026






Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in