Symptoms and respiratory infections: Insights from the UK 2022/2023 winter season
Published in Public Health and Statistics
Ever wondered about the likelihood of having the flu if you’ve got a fever? Or how your age influences the symptoms you experience if ill with RSV? And can we distinguish SARS-CoV-2 from other respiratory infections based on which symptoms people report? These are some of the questions our recent research study explored. In this blog post, I’ll explain the motivation behind our study and highlight our key findings.
What was our study about?
Respiratory infections affect lots of people every winter, and cause symptoms such as sneezing or fever. Often, these symptoms are mild, but such infections can also lead to more serious illness. Understanding how many people are getting different respiratory infections over time, and what symptoms they experience, is important to accurate diagnosis and effective treatment in the NHS. Getting more knowledge about these infections can also aid healthcare preparedness and inform vaccination policies.
Influenza A/B (flu) and respiratory syncytial virus (RSV) are two common causes of respiratory infection. Since the start of the COVID-19 pandemic, SARS-CoV-2 has also been co-circulating with these viruses. Our recent study investigated these three respiratory infections in the UK during the 2022-2023 winter season, along with self-reported symptoms. This study was based on a large household survey, the Office of National Statistics COVID-19 Infection Survey. Around 750 participants in the survey were randomly selected each week to have their nose and throat swabs PCR-tested for flu, RSV, and SARS-CoV-2. Our research study analysed this data using a range of statistical methods, including generalised additive models, which is a type of regression model.
What were the main findings?
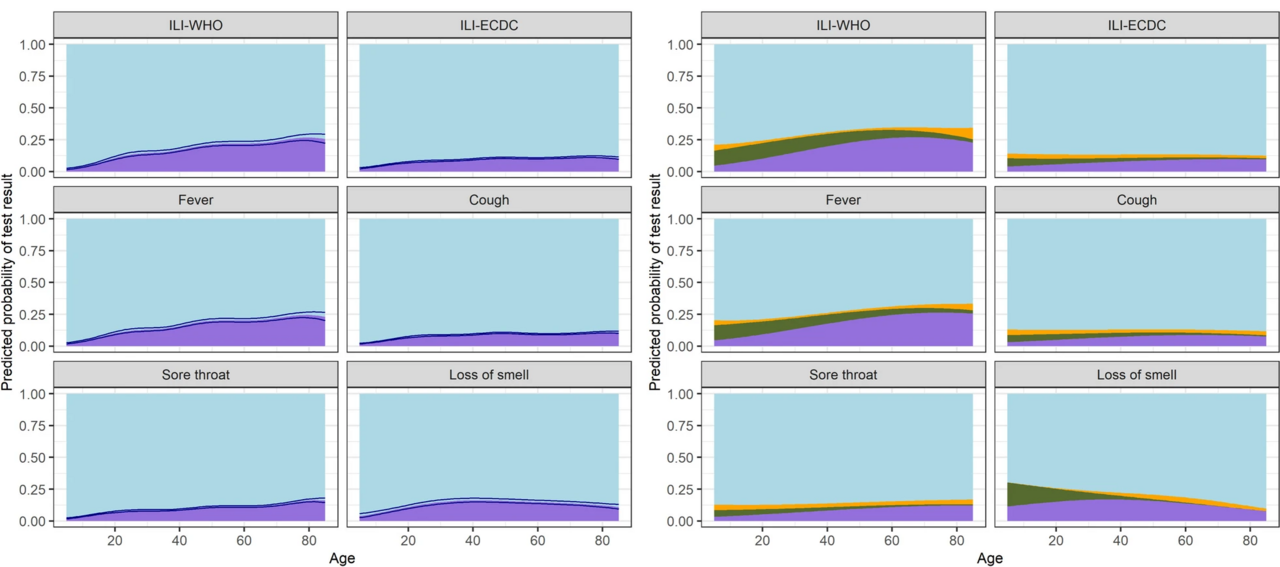
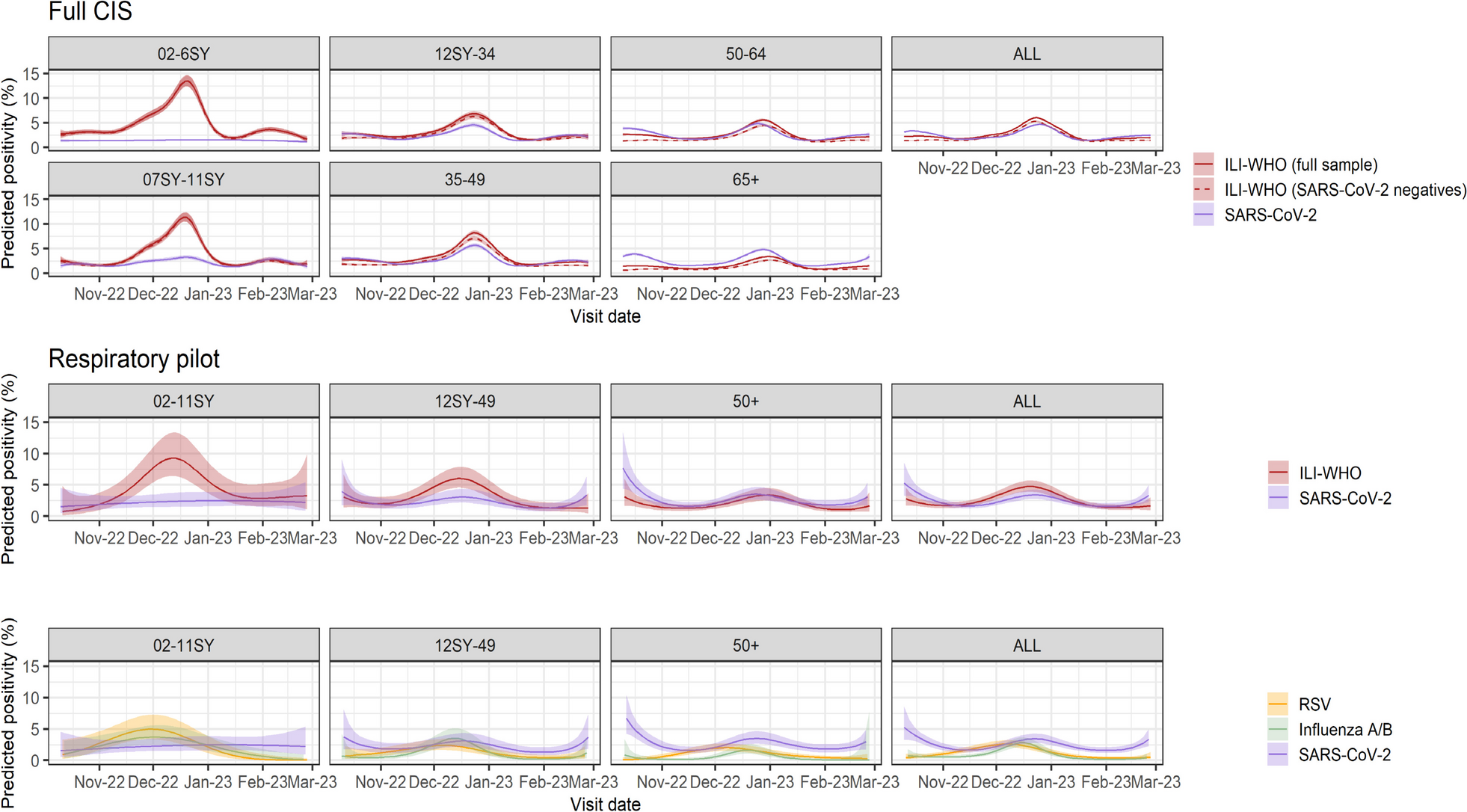
Our study found that differentiating between flu, RSV, and SARS-CoV-2 based on symptoms alone may prove difficult. Symptom profiles were largely similar across the three viruses, with middle-aged participants being more likely to report symptoms than other age groups. Cough, sore throat, sneezing, and fatigue were amongst the most common symptoms for all three infections.
We did however see some differences between the three infections. For instance, RSV-positive people in our study generally reported fewer symptoms than those who tested positive for SARS-CoV-2 or the flu. In particular, fever was relatively uncommon amongst those with RSV. Importantly, we also observed considerable background rates of several symptoms, especially cough in young children, and fatigue and headache in middle-aged participants.
SARS-CoV-2 positivity was notably higher in adults than children, and RSV was more common in children below school year 12 than in older participants. Flu was also less common in participants aged 50 years and above than in younger age groups. By estimating incidence over time using a technique called Richardson-Lucy deconvolution, we found that flu peaks occurred earlier in children than older adults, with a delay of around 2 weeks.
Many of the symptoms reported by people in the survey could not be explained by either of the three viruses we studied, highlighting the role of other infections such as the common cold. Fever was the symptom with the highest percentage of test-positive participants. The likelihood of testing positive for either of the three viruses generally increased by age across symptoms. However, even in older individuals reporting influenza-like-illness as defined by the WHO, only around ~30% had a positive test result for either SARS-CoV-2, the flu, or RSV. We also found that reporting flu vaccination in the past two winter seasons was associated with a lower likelihood of testing positive for flu in the current season.
What are the implications?
Given our findings, further research is needed on the role of other infections such as rhinovirus in causing respiratory symptoms. Future studies would benefit from having more specific data about the onset timing of symptoms and infections. However, our study emphasises the value of community-level data to understanding trends in respiratory infections and symptoms in people outside healthcare settings. Our study also raises important questions about the role of age in infection susceptibility, illness natural history, symptom reporting behaviour, and vulnerability to other symptom-inducing conditions. These questions provide promising avenues for future research, and highlight important considerations to the NHS and public health more broadly.
Follow the Topic
-
BMC Medicine

This journal publishes outstanding and influential research in all areas of clinical practice, translational medicine, medical and health advances, public health, global health, policy, and general topics of interest to the biomedical and sociomedical professional communities.
Related Collections
With Collections, you can get published faster and increase your visibility.
Weight loss interventions and their health impacts
BMC Medicine is calling for submissions to our new Collection on weight loss interventions and their health impacts, emphasizing a variety of strategies, including dietary changes, physical activity, pharmacological treatments, and surgical options. We encourage submissions that explore the long-term effects of these interventions, adherence challenges, and strategies to address health inequities. The goal is to advance understanding and improve outcomes in weight management and overall health.
Weight loss interventions encompass a wide range of strategies aimed at reducing body weight and improving health outcomes. These interventions can include dietary changes, increased physical activity, pharmacological treatments, and surgical options such as bariatric surgery. As the global prevalence of obesity and related comorbidities continues to rise, understanding the efficacy and mechanisms of various weight loss interventions becomes increasingly crucial for public health. This Collection seeks to explore the diverse methodologies and outcomes associated with weight loss interventions, offering insights into their impacts on both individual and population health.
The significance of this research is underscored by the growing body of evidence linking obesity to numerous chronic health conditions, including diabetes, cardiovascular diseases, and certain types of cancer. Advances in pharmacological treatments, such as SGLT2 inhibitors and GLP-1 agonists, have emerged as promising options for weight management, demonstrating not only weight loss but also improved metabolic health. There are, however, challenges and limitations related to drug availability, healthcare delivery, and long-term treatment adherence with rapid weight gain when stopping treatment. Additionally, integrating behavioral strategies with nutritional and physical activity interventions has shown potential in enhancing adherence and long-term success. By further investigating these modalities, we can develop comprehensive approaches that address the multifactorial nature of obesity.
Continued research in this domain may yield innovative strategies that harness technology, such as mobile health applications and telehealth, to support weight loss interventions. As we deepen our understanding of the genetic, environmental, and behavioral factors influencing obesity, personalized interventions tailored to individual needs could emerge. This progress may lead to improved health outcomes, reduced health inequities, and ultimately a shift in the paradigm of obesity treatment and prevention.
We are looking for original manuscripts on topics including, but not limited to:
•Clinical trials investigating interventions for weight loss to promote health
•Real-world data on long-term effects and challenges of weight loss interventions
•Factors affecting long-term adherence to weight-loss or weight maintenance interventions
•Challenges and inequities in access to weight loss interventions
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
This Collection supports and amplifies research related to SDG 3: Good Health and Well-being.
Publishing Model: Open Access
Deadline: May 07, 2026
Climate change and human health
BMC Medicine is calling for submissions to our new Collection on the health impacts of climate change. The relationship between global warming and human health is increasingly becoming a focal point in public health research. Rising temperatures, shifting weather patterns, and extreme weather events are projected to have profound effects on various health outcomes. From increased prevalence of vector-borne diseases to heightened risks of heat-related illnesses, the health implications of climate change are vast and multifaceted. This Collection aims to explore the direct and indirect impacts of global warming on health, examining how these changes affect vulnerable populations and health systems worldwide.
Understanding the implications of global warming for human health is crucial for developing effective public health strategies and interventions. Recent research has highlighted the links between climate change and a variety of health issues, including air pollution, water-borne diseases, and undernutrition. Advances in climate modeling and epidemiological studies have enhanced our ability to predict health outcomes related to climate change, providing invaluable insights that can inform policy decisions and health care planning.
Continued research in this area may lead to innovative solutions to mitigate the health impacts of climate change. For example, interdisciplinary approaches that integrate climate science, public health, and social determinants of health could reveal new pathways for adaptation and resilience. Future studies may also focus on the development of health infrastructure designed to withstand climate-related stresses, thus improving community health outcomes in an era of global warming.
We are considering manuscripts on, but not limited to the following topics:
-Impact of air pollution on health
-Heat-related illnesses
-Water-, and vector-borne diseases in a warming world
-Social determinants of health and climate vulnerability
-How health systems and infrastructure may be affected by climate change
-Nutrition and health in the context of climate change
-Impacts of climate change on non-communicable diseases
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
This Collection supports and amplifies research related to SDG 3 (Good Health and Well-being) and SDG 13 (Climate Action).
Publishing Model: Open Access
Deadline: Mar 02, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in