Spatial and Contextual Disparities of Influential Factors of Adult Obesity among Communities in Chicago
Published in Social Sciences, Earth & Environment, and Ecology & Evolution
This study examines the nineteen demographic, socioeconomic, behavioral, and environmental factors influencing adult obesity across Chicago’s 77 community neighborhoods. Using advanced geographic methods—including geo-visualization, Exploratory Spatial Data Analysis (ESDA), Analysis of Variance (ANOVA), and Geographically Weighted Regression (GWR), the study provides a nuanced understanding of how obesity patterns cluster geographically and how multifaceted risk factors vary spatially across the city.
Data & Methods
The demographic data (percentage of White, African American, Hispanic, and other minority groups) from the American Community Survey (ACS). Adult obesity data came from the Chicago Health Atlas. Physical environment determinants included Sidewalk Quality, Land Use Mix Index (LUMI), Number of Parks, Walkability Index (WI), Social Vulnerability Index (SVI), and density of Fitness Centers. Behavioral data, such as adult smoking, psychological distress, neighborhood safety, and loneliness, as well as socioeconomic variables, including the Hardship Index (HI), unemployment rate, Economic Diversity Index (EDI), poverty, food insecurity, and public assistance income, were also obtained from the Chicago Health Atlas. Together, these variables illustrate a complex interplay of contextual factors determining health outcomes. The analytical framework involved spatial statistics to measure clustering and spatial relationships. Local Moran’s I identified obesity "hotspots" and "coldspots," showing statistically significant geographic controls. GWR allowed coefficients to vary spatially, rather than assuming uniform effects across the city, providing a local rather than a global view of the factors driving obesity.
Spatial Distribution of Adult Obesity
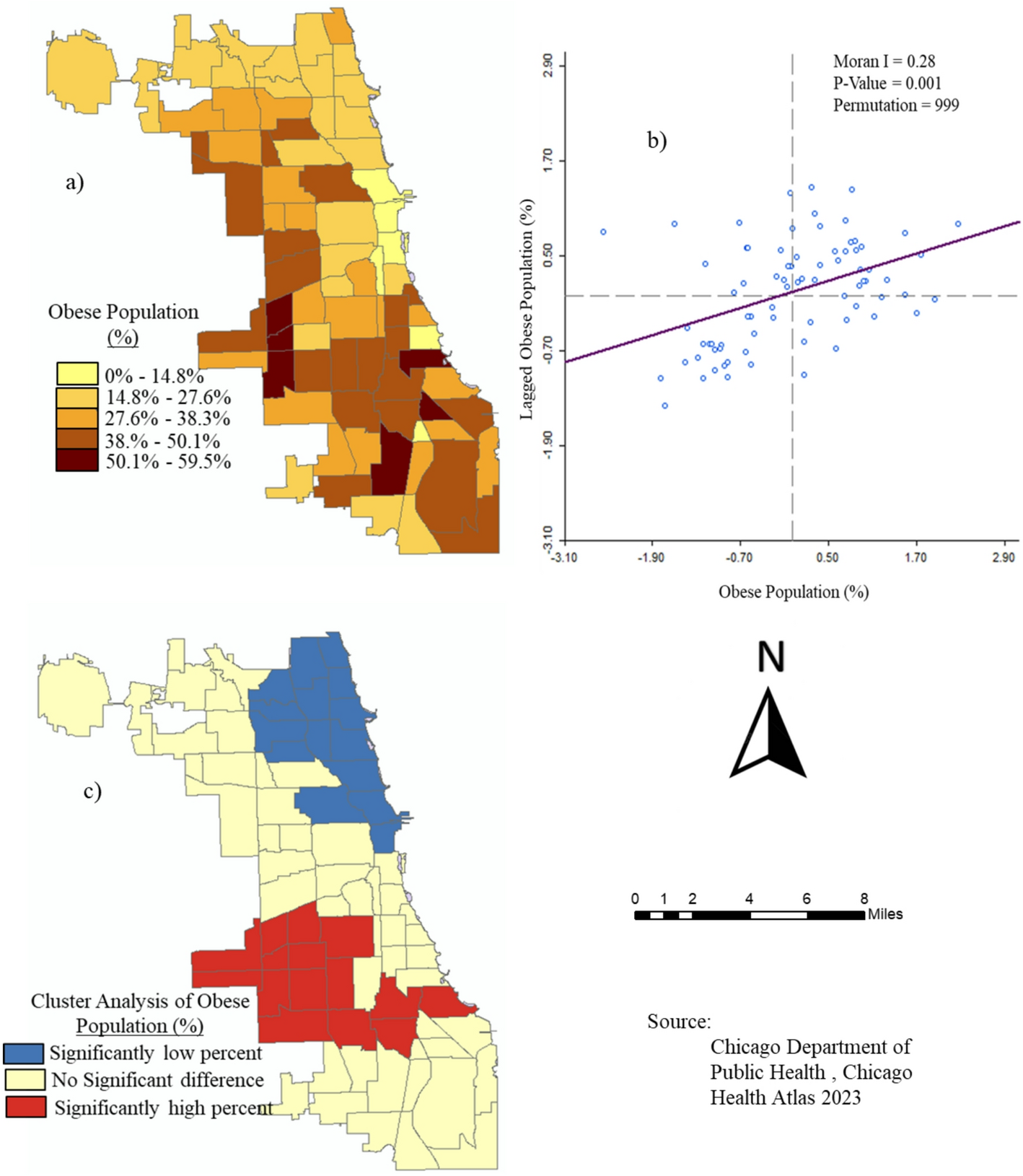
The spatial analysis revealed substantial variation at the neighborhood level. Obesity rates ranged from under 10% in parts of the Near South Side to nearly 60% in places such as Archer Heights. Chicago’s average obesity prevalence (32%) is comparable to the Illinois average but lower than the U.S. average, yet it far exceeds the global average. ANOVA confirmed statistically significant differences across Healthy Chicago Equity Zones (HCEZs), with Central, North, and Far North zones showing significantly lower rates, while Southwest and West zones exhibited the highest burdens. Moran’s, I detected significant positive spatial autocorrelation (I = 0.28), confirming obesity clustering rather than random distribution. Southwestern and western neighborhoods formed consistent high-obesity clusters; northern and central zones formed low-obesity clusters.
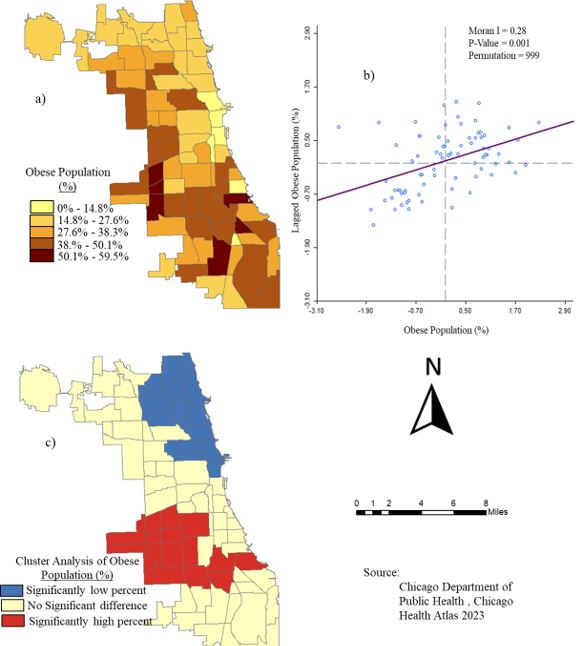
Fig. 1 Spatial analysis of the pattern of the adult obese population rate among Chicago neighborhoods: a) adult obese percentage, b) Global Spatial autocorrelation for geographic control, and c) cluster analysis
Disparities in Adult Obesity Determinants in space and context
Race and ethnicity emerged as powerful predictors of spatial location, with the White residents having a strong negative association with obesity rates (R² = 0.39), while minority residents showed strong positive associations (R² = 0.39). The strongest associations among minorities occurred in historically Black neighborhoods on the West and South Sides. Roughly 32% of neighborhoods had little to no association with demographic obesity, particularly in more racially mixed northern communities. On the other hand, Environmental determinants such as sidewalk quality, land use mix, park distribution, walkability, and fitness center density. Among environmental variables, walkability showed the strongest relationship (R² = 0.43), followed by sidewalk quality (R² = 0.33) and fitness centers (R² = 0.23). Surprisingly, the number of parks and the land use mix showed weak associations (R² = 0.06–0.08), suggesting that the mere presence of parks does not guarantee usage, accessibility, or quality, especially in neighborhoods that are not safe for walking and other physical activities.
Table 1: Spatial Relationships of Percentages of Adult Obesity and Demographic Composition of Chicago Neighborhood Communities
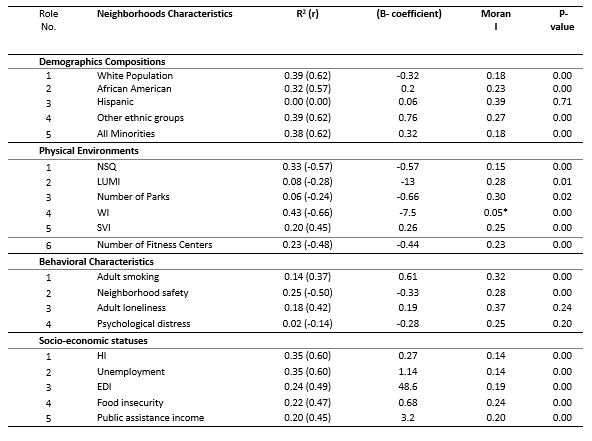
Similarly, Behavioral factors like Adult smoking and psychological distress were positively associated with obesity, while neighborhood safety was negatively associated. The findings support broader literature linking obesity to chronic stress, trauma, social isolation, and unsafe environments that limit outdoor physical activity. Lastly, the socioeconomic stressors showed some of the strongest and most statistically significant associations with obesity. Hardship Index and unemployment rate each explained 35% of the variance in obesity rates, while food insecurity, poverty, EDI, and public assistance income also showed moderate associations. Over half of the neighborhoods, however, showed no association, indicating that socioeconomic determinants alone cannot explain all variation, which underscores the multifactorial nature of obesity.
Conclusion
Adult obesity in Chicago communities is shaped by a complex interplay of demographic, environmental, behavioral, and socioeconomic factors operating within spatially distinct contexts. Obesity does not occur randomly; it clusters in neighborhoods characterized by racial segregation, economic hardship, lower walkability, limited fitness infrastructure, higher smoking rates, and psychological distress. Therefore, effective interventions must consider spatial heterogeneity and tailor strategies to local conditions. Policies should target structural inequities, enhance physical environments, increase access to health-promoting resources, and address behavioral health needs. Despite limitations including autocorrelation biases and multicollinearity, the study provides a robust empirical foundation for spatially informed public health planning and equity-focused interventions in Chicago.
Follow the Topic
-
Discover Public Health

This is an open access journal publishing research from all fields relevant to public health.
Related Collections
With Collections, you can get published faster and increase your visibility.
Public Health Strategies for the Management and Prevention of Tobacco Use and Emerging Tobacco Products
Tobacco use is considered as one of the hidden epidemics of the 21st century. Despite many efforts at policy level, tobacco use still remain one of the key factors for high morbidity and mortality worldwide. Globally around eight million people die due to tobacco consumption while daily people are diagnosed with lung cancer, COPD, cardiovascular diseases etc., with main factor being the tobacco consumption. Tobacco prevalence range between and within regions and countries as well as between male and female gender. Tobacco uses usually starts at adolescent and continue in the later life. At global level several initiatives have been undertaken with the WHO-FCTC being one of the most important. Additionally, at national levels countries have undertaken several initiatives but with not very successful results. On the other hand, tobacco industry is putting priority in the new products such as electronic cigarettes, heated tobacco etc. These products are not considered in many regions and countries as the normal tobacco products with their taxation, availability and use being different. To some extent, healthcare systems are not performing well in the management of the tobacco use which is considered a chronic condition. Availability of new medicaments and approaches and techniques is still a problem in many settings worldwide. Combination of tobacco use and other substances is also a critical issue.
This Collection aims to discuss key strategies for management of tobacco use and the new products at local, national, regional and global level as well as to propose key measures for healthcare personnel and policymakers in order to manage key challenges. Authors from different settings and different backgrounds are invited to submit their works to this Collection. Reviews and systematic analyses and meta- analyses, original articles, policy papers and case-studies are more than welcome to be submitted.
Research areas may include but are not limited to the following:
- Tobacco consumptions
- New tobacco products
- Prevention and management of tobacco use
- Substance use
- Technology and public health
- Prevention and health promotion
Keywords: tobacco, heated tobacco, public health, health policy, prevention and health promotion
This Collection supports and amplifies research related to SDG 3.
Publishing Model: Open Access
Deadline: Apr 30, 2026
Antimicrobial Resistance: The New Challenge to Global Health in a Post-Pandemic World
Antimicrobial resistance (AMR) is a seriously ongoing threat to global health, occurring when bacteria, fungi, viruses, and parasites evolve to resist the drugs designed to kill or block them. The COVID-19 pandemic has both directly and indirectly exacerbated the problem of AMR, as the overuse of antibiotics has accelerated the development of resistance in many pathogens. COVID-19 may have subsided, but AMR continues to pose a significant risk to the effectiveness of global healthcare systems, threatening to reverse decades of progress in combating infectious diseases. The interplay between population health and AMR has become increasingly critical as healthcare practices have shifted in response to the pandemic. Understanding this relationship is essential for developing effective strategies to mitigate the impact of AMR on population health in a post-COVID context.
The motivation for launching this Collection arises from the urgent need to address the rising tide of AMR as healthcare systems grapple with the long-term effects of the pandemic. Increased antibiotic use during COVID-19 treatment, changes in healthcare access, and disruptions in public health interventions have all contributed to an environment where AMR can thrive. Moreover, the pandemic has highlighted the importance of a multidisciplinary approach to tackling AMR, involving epidemiology, policymaking, and community health initiatives. This Collection aims to provide a platform for researchers and practitioners to share insights and findings that can inform future strategies to combat AMR while considering the broader implications for population health.
This Collection aims to highlight the multifaceted nature of AMR in a post-pandemic environment. We solicit articles that investigate the particular issues provided by the pandemic in terms of AMR development and containment, examine the impact of AMR on many sectors of healthcare, and propose novel strategies to minimize resistance propagation. Submissions may include original research, policy assessments, program evaluations, and comments on the following major areas:
• Epidemiology and trends of AMR post-pandemic
• Impact of COVID-19 on antibiotic usage
• Surveillance strategies for AMR
• AMR and stewardship
• Prevention and control measures to limit AMR spread
• Policies and programs to promote antibiotic stewardship
• Economic and social implications of AMR
• Global collaboration and initiatives to tackle AMR
By addressing these critical issues, this Collection aims to provide a comprehensive understanding of the emerging challenges in antimicrobial resistance in a post-pandemic world and to promote effective strategies to preserve the power of our current antimicrobials.
Keywords: antimicrobial resistance; COVID-19; antibiotics; global health; infectious diseases; public health; policy; prevention
This Collection supports and amplifies research related to SDG 3.
Publishing Model: Open Access
Deadline: Jun 30, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in