Migraine and depression: what relates these complex disorders?
Published in Neuroscience, Genetics & Genomics, and Behavioural Sciences & Psychology
In many ways, migraine and Major Depressive Disorder look very different. Migraine is a disorder with repeated attacks that usually have acute triggers and unfold over a relatively short timespan (hours to days). Triggers can include foods, sounds, smells, atmospheric pressure, lighting (too bright, too much contrast, or blinking), irregular sleep, hormones and more. Migraine attacks unfold in characteristic phases including a prodrome phase (characterized by mood changes, cognitive impairments, yawning, and other symptoms), in some patients aura (visual hallucinations and/or partial paralysis), headache (including extreme sensory hypersensitivity), and a post-drome phase (lingering symptoms, fatigue, depressive mood).
By contrast, depression tends to last much longer (weeks, months, or even years) and is much less time-specific in how symptoms may present. Patients display at least five symptoms that include depressed mood, diminished interest or pleasure, changes in weight or sleep, psychomotor agitation or slowed thinking, fatigue, feelings of worthlessness or excessive guilt, diminished concentration, or recurrent thoughts of death or suicide).
We (as authors) have known people personally who have suffered from both migraine and depression and have thought a lot about what might be the relationship, if any, between these seemingly very different conditions. Does one disorder predispose a person to the other? Are there shared underlying relationships in brain or nervous system physiology that might provide a causal link?
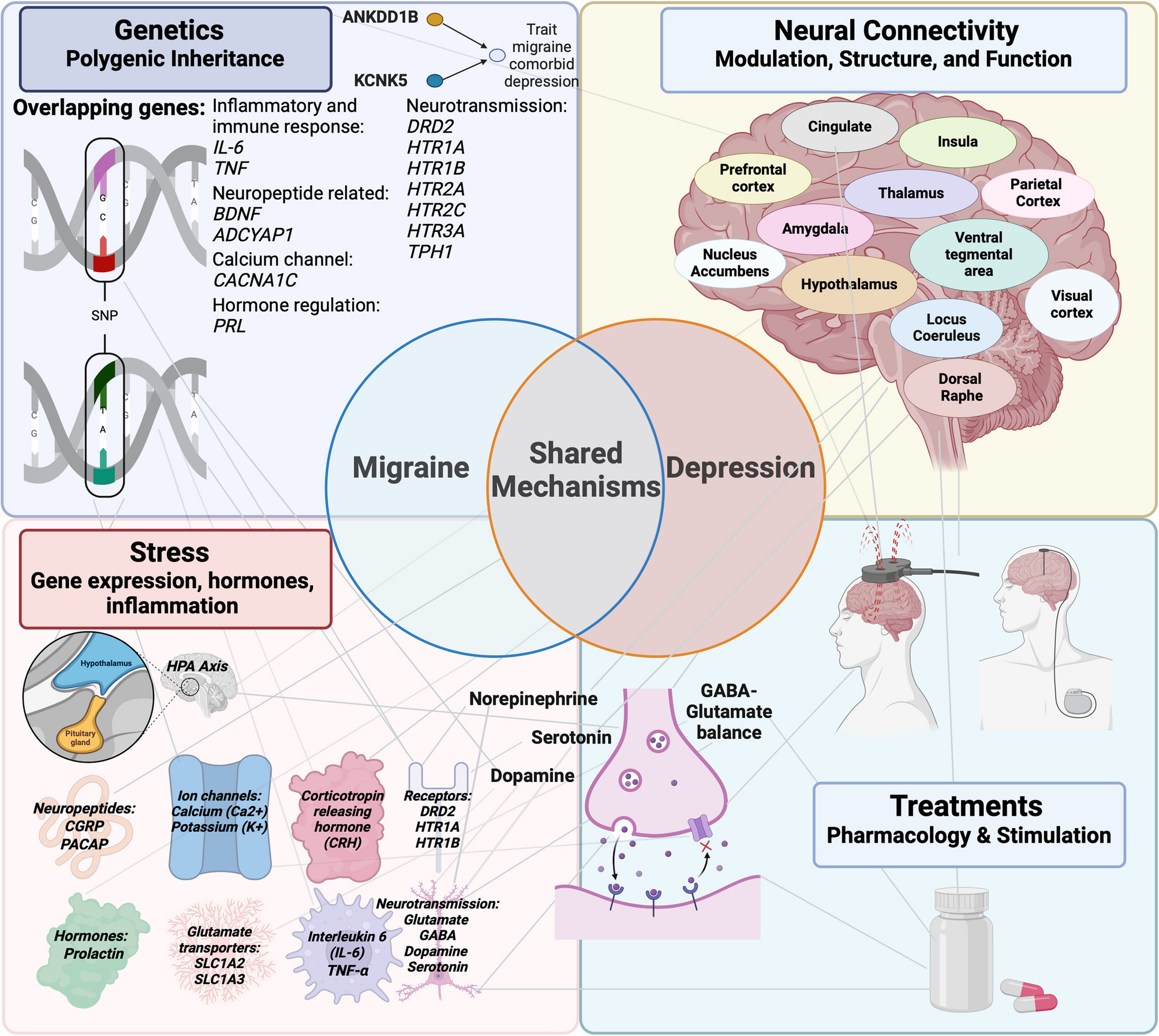
We surveyed what is currently known about the mechanistic contributors to each disorder and examined what they have in common across treatment and physiological mechanisms from genetics through brain-wide communication.
Common Threads:
Our literature search found several emergent themes of mechanistic overlap between migraine and MDD spanning multiple levels of analysis, including:
- Key genetic risk variants and genes common to both disorders
- Overlap in the mechanisms of therapeutics used to treat each disorder, including the effects of these treatments on neurotransmitters and peptides
- Shared disruptions in the regulation of sensory sensation and mood
- Key brain regions and circuits
- Common physiological responses to environmental factors
- The critical role of sex differences and clues from hormones
Why Now?
With emerging therapies for each of these disorders, there are new opportunities to consider for patients. Having a better understanding of where mechanisms between these two disorders overlap and differ can shed light on 1) therapeutics that may not have been thought of for the opposite disorder, or that may work for both conditions, 2) unexplored mechanisms that are worth further probing for each disorder and 3) for creating therapeutics with the least likelihood of unwanted side-effects. Focusing on the mechanisms that these disorders have in common provides a strategy for scientists to consider for developing therapeutics to best target the comorbid condition.
An example of an emerging therapy in migraine with relevance to depression includes anti-CGRP therapies. Calcitonin gene-related peptide (CGRP) is a peptide involved in inflammation, blood vessel dilation, and many other physiological functions and provides one of the most exciting recent examples of a therapeutic derived from neuroscience research. A promising new development is that a recent clinical trial showed success for one such anti-CGRP therapy in the treatment of migraine with comorbid depression (https://jamanetwork.com/journals/jamaneurology/fullarticle/2833452). Given that historically, patients living with migraine and comorbid depression have been excluded from many such studies, this finding represents an important step forward .
By contrast, an example of an emerging therapy in depression with relevance to migraine is ketamine. Ketamine impacts a wide range of biology but is best characterized for its role as a glutamate receptor antagonist, thus impacting excitatory/inhibitory balance, a mechanism important in migraine. Several small studies have found success with ketamine for treating migraine, opening the door to larger studies that can ask whether there are specific patients that may especially be good candidates for ketamine.
Overall, such findings may pave the way for development of novel therapeutics designed to target both disorders instead of treating them as separate problems. Our review provides a roadmap for future studies to truly understand these two disorders and the comorbid condition. We hope it will ignite conversation and provide fresh insight into patients with a dual diagnosis.
Have further thoughts or questions on this topic? Leave us a comment below!
For more information about the Laboratory for Brain-Network Based Molecular Medicine, please visit our lab website here: https://hultman.lab.uiowa.edu/
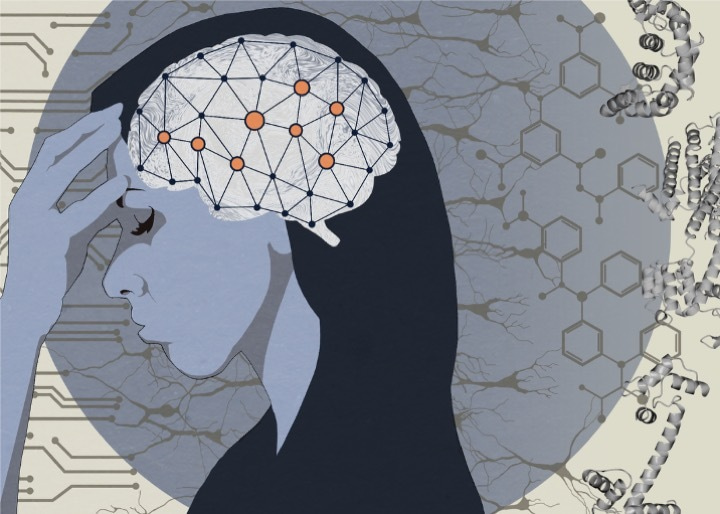
Artwork credit: Jeff MacInnes https://www.decimalpoint.studio/
Follow the Topic
-
The Journal of Headache and Pain

The Journal of Headache and Pain is a peer-reviewed open access journal specifically dedicated to researchers involved in all aspects of headache and related pain syndromes, including epidemiology, public health, basic science, translational medicine, clinical trials and real-world data.
Related Collections
With Collections, you can get published faster and increase your visibility.
Focus Africa
The Journal of Headache and Pain is calling for submissions to our Collection on Focus Africa. Migraine is a major cause of disability worldwide, yet research efforts and healthcare strategies remain unevenly distributed across regions. In Africa, diverse populations and healthcare landscapes present unique challenges in the recognition, diagnosis, and management of migraine and other headache disorders. This thematic collection, Focus Africa, aims to enhance understanding of these conditions by exploring epidemiological trends, healthcare disparities, cultural influences, financial constraints, gender-related factors, and the availability of treatment options across the continent.
We invite submissions of original research, systematic and narrative reviews, editorials, rapid reviews, and commentaries on topics including, but not limited to:
• The prevalence, burden, and impact of migraine and other headache disorders across African countries
• Socio-economic and cultural determinants of headache disorders in Africa
• Insights into the pathophysiology of migraine from an African perspective
• Barriers to headache care, healthcare inequalities, and policy solutions
This Collection provides a dedicated platform for African researchers and clinicians to contribute to global headache science while addressing the specific needs of the region. By fostering collaboration and knowledge exchange, Focus Africa aims to drive meaningful advancements in migraine and headache disorders research and care across the continent.
Therefore, the collection welcomes researchers from author groups all with their main affiliated institution in Africa. Cross-continental authorship groups are welcome to submit their work to The Journal of Headache and Pain outside of this collection.
Springer Nature offers article processing charges (APC) waivers and discounts for articles published in our fully open access journals whose corresponding authors are based in the world’s lowest income countries (see our APC waivers and discounts policy for further information). Requests for APC waivers and discounts from other authors will be considered on a case-by-case basis and may be granted in cases of financial need (see our open access policies for journals for more information). All applications for discretionary APC waivers and discounts should be made at the point of manuscript submission; requests made during the review process or after acceptance are unable to be considered. Should applications for financial support via the above process be unsuccessful, authors are encouraged to reach out to the journal.
Publishing Model: Open Access
Deadline: Mar 20, 2026
Community pharmacy and headache care
In the sustainable development goals (SDG) context of seeking universal health coverage, the expanding gap between the supply of specialized and primary providers of headache-related health care on the one hand and the care needs of the very large number of people affected by headache on the other is a formidable but not insoluble public-health challenge. Structured headache services provide a cost-effective framework for provision of care but may still be overwhelmed by demand. Community pharmacists are an underutilized resource, potentially well able to provide the solution. This collection aligns with UN SDG-3 (Ensure healthy lives and promote well-being for all at all ages), and more specifically with SDG-3.8 (Achieve universal health coverage ..., access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines ... for all). The collection may include reports (especially comparative studies) on current pharmacy practice (scope, responsibilities and regulatory and other restrictions) relevant to headache care in countries worldwide — especially, but not restricted to, low and lower-middle-income countries; studies of pharmacists' knowledge and understanding of headache disorders and their management, theoretically argued proposals for change that, through educational initiatives, expansion of community pharmacists' scope of practice or by other means, might relieve strained headache-care systems; and studies of workload-shifting in headache care from medical to community pharmacy services (economic evaluations, theoretical or empirical assessments of benefits versus harms, and reports of pilot implementations either in headache care or in other therapeutic areas that might be pathfinders for headache care).
This Collection supports and amplifies research related to SDG 3, Good Health & Well-Being.
All submissions in this collection undergo the journal’s standard peer review process. Similarly, all manuscripts authored by a Guest Editor(s) will be handled by the Editor-in-Chief. As an open access publication, this journal levies an article processing fee (details here). We recognize that many key stakeholders may not have access to such resources and are committed to supporting participation in this issue wherever resources are a barrier. For more information about what support may be available, please visit OA funding and support, or email OAfundingpolicy@springernature.com or the Editor-in-Chief.
Publishing Model: Open Access
Deadline: May 01, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in